Jay Desai, MBA is co-founder and CEO of PatientPing of Boston, MA.

Tell me about yourself and the company.
Prior to starting PatientPing, I worked at Medicare at CMMI, the CMS Innovation Center. There I worked with a team to help implement the ACO program, bundled payments, and a lot of the other new payment models coming out of CMMI. The goal was to preserve the PPO model. No prior authorization, no utilization management, no traditional managed care control, no differential co-pays out of network, no PCP as a gatekeeper. Let patients go wherever they want to go. But risk.
Therefore, we needed to come up with an attribution model that was based on alignment, not necessarily membership enrollment. In that model, when a patient goes somewhere to receive care, you don’t really have too much control over them staying in network or even coordinating the care after they finish their episode, because you don’t know about it.
That created a major pain point for providers in this new model. A very basic problem emerged, which was, "Just tell me where my patients are” in real time — when they go to the hospital, ED, SNF, home health agency, or wherever they go. After scanning around the country and looking at the solutions that were available to providers, it felt like there was an important opportunity to build something that was focused and lightweight that could help providers know in real time where their patients are.
It seems as though it should be easy to send ADT notifications. Why wasn’t that happening already and what allowed you to turn that into a significant business?
A big part of the complexity in building this business is in the need for broad market adoption. Let’s say you’re an IPA. You get your list of patients and you want to know where they’re going. There may be 10 hospitals that represent a majority of them, and then there’s a long tail of other hospitals. On top of that, there’s 300 skilled nursing facilities, 200 home health agencies, 50 FQHCs and community health centers, a bunch of LTACs, and a spattering of other community providers. That’s a big list.
Building connectivity to all of those participants requires not only the technical implementation, but engagement and a reason to do this. You need to engage them not just as data senders or data providers. For any of those sites that’s a referral site for an IPA, you need to engage them as data providers, but also as participants in the community to engage in the coordination of care with those other endpoints. That’s hard to do because it’s easier to sell a technology to one group and not worry about all the other places that they’re going to be a part of.
Our solution is about that. It’s about building the network, building the community for everybody to engage. Designing something that is light enough and gets broad participation and lift very quickly without being intrusive and with organizations that create constituency groups to do it was part of the challenge. How do you create something that’s elegant that still gets buy-in across the continuum of care, where sometimes there’s competitive dynamics that block information sharing, but still break down some of those barriers for folks to work with one another?
Who pays you, what sharing agreements do providers sign, and do they have to get patient consent?
There’s no cost to send the data. We only charge to receive information, what we call it pings. You pay to receive pings. That’s the real-time notifications.
There’s a lot of other bells and whistles to the service that I’m not describing now, but fundamentally that’s how it works from a business model perspective. It’s lightweight, it’s low cost, and it gets everybody in the community connected as both the sender and a receiver. You can join the community as a sender. You don’t necessarily need to receive, and in that world, it would be free.
For patient consent, we adhere to whatever the state rules are. In Vermont, for instance, we have a blacklist of patients who have opted out of data sharing and we will make sure not to share information on them. What we’re sharing isn’t very rich clinical information — we’re not sending lab results or behavioral health information. We provide the notifications. That could be on patients with behavioral health disease. The fact that they’re at the emergency room is what we would tell them, not necessarily that they’re there with a flare-up of a substance abuse issue or anything like that. The fact that they’re in the emergency room is something that we would be able to notify behavioral health providers about.
My point is that it’s a light level of data sharing. We seek consent in any instance where we have to. We have our own strict policies around how long is one considered a covered entity and how long is one considered a provider so that we’re not sharing data with people who aren’t allowed to see it.
As a provider, what’s my workflow when I get a ping?
There’s a lot of variability to how any given end user is going to act on a notification. They’re further variability in terms of the destination of where the patient is receiving care that will determine how they act on it.
For instance, if I’m an ACO care coordinator and I receive a notification that a patient is in the emergency room, a workflow may be in place to call the emergency room provider and call the patient to make sure that emergency room provider is aware of any case management services that may be available for the patient. Just to engage them in care coordination or case management upon discharge. They may also let the emergency room provider know that there are other supports for them in case they don’t want to admit the patient and want to take them out of the emergency room, to the extent that that’s an option for the patient and the emergency room provider feels like that’s the right thing to do.
If the provider receives a notification of a hospital discharge, they may initiate their medication reconciliation workflows or their transitions of care management workflows to get them in for a follow-up visit with a PCP or a specialist. If they get a notification that a patient is in a skilled nursing facility, they may have a regular rounding schedule or a clock that sets the timeline around when they should reach out to manage the length of stay at the SNF, largely to make sure that they’re supported with home care if that’s what’s required after the rehab period at the SNF. Again, that will be a function of the workflows.
They may want to make sure upon discharge that the patient is getting to the right post-acute care facility that’s part of a preferred network or deemed to be a high-quality provider. Another example is that if you’re a skilled nursing facility, your patient leaves your SNF, and you’re paying to receive the service when the patient bounces back to the ED, you would get notified. You may use the notification to call the emergency room to let the emergency room provider know that the patient is eligible to come right back to the SNF without a three-day hospital stay, for instance. That way, the emergency room provider can send them back into the community as opposed to admitting them to the hospital.
I can go through a long list of how our users are acting on the notifications. Home health agencies may go to the patient’s home on Day One to set up home care. They’ll show up on Day Three and nobody’s there because the patient’s caregiver never told the home care provider that they went back to the hospital. So the home health agency may use it to verify that the patient is still at home and that they can continue to deliver services. Or if they go to the emergency room, they can reach out to the emergency room and let them know that the patient has home care if they want to send them back out into the community.
Is it always providers who are at risk that buy your service or would it ever be an insurance company?
There are case management services that are being offered by insurance companies that want to initiate their workflows when their patients show up at the hospital and the emergency room. They may use their prior authorization processes as a data source, but a lot of times the ER data is not readily available on a real-time basis because the billing clerks for the emergency room will batch bill or do them later, so it won’t be as real time as an ADT message. We have some health plan case management services that are receiving the notifications.
In the example I gave you of a home health agency getting a ping, they’re not at risk, necessarily. They are just providing their home care services. Being able to know the patient’s whereabouts allows the home care provider to deliver a high quality of care.
Other groups that are interested in our services are homeless shelters and social service agencies that are providing case management. This is the big reason that I started this company. At CMS, a lot of our work was to bridge the community providers with the acute care setting. I worked a lot on some of the preventative services as well, around getting social supports — whether it’s housing supports or Meals on Wheels — also included within the care coordination workflows. The emergency room is a vulnerable time for the patient and an opportunity to engage them in their follow-up to make sure that they’re getting the right care.
What did Silicon Valley investors see in the company that made them want to invest $40 million?
I’d love to ask them the same question. [laughs] I’d love for you to ask them that question as well.
We are entirely mission-driven. We are maniacally focused on connecting providers to seamlessly coordinate patient care. Patients get care from a lot of providers — seven providers on average for a Medicare patient — and they’re across a lot of unaffiliated and disparate organizations. That results in a lot of cost, a lot of excess use, and redundant procedures. That’s the value of coordination.The work that needs to happen to prevent some of that redundant work is not complicated. It’s straightforward.
What we’ve done is design a solution that meets the provider community where they are, with a straightforward, low-cost, non-intrusive, easy-to-use solution that connects them in a way that they haven’t experienced in the past. We think that the investor community is excited about us bringing our services and spreading our mission to the rest of the country and we’re thrilled to be able to do that.
Of the syndicate that we formed here, Todd Cozzens of Leerink Transformation Partners is extraordinary. The folks at Andreesen Horowitz – Vijay and Jeff Jordan – are just incredible people. What we’re excited about is the opportunity to bring the best of two very different approaches to building healthcare IT businesses. There’s the Silicon Valley approach of hyper growth and product and network effects, which is a big component of what we do, but we are serving the provider community. We don’t make any allusions about the fact that the workflows are complicated. I’m a healthcare person. I’ve worked in the healthcare industry for over a decade. I’m not a Silicon Valley tech outsider coming into this industry.
I’m very familiar with businesses like the ones that Todd has built and the folks at Leerink have built. There’s a certain discipline to focusing hard on delivering a clear ROI to your provider organization customer, being very sensitive to the regulatory environment, and making sure that we are hyper focused on the integrity of our data and patient consent. Not just not trying to hack our way through an industry that is designed the way that it is for good reason. This is patients that we’re talking about. There’s a good reason for the bureaucracy. There’s a good reason for the slower processes and change cycle.
That said, there is some wisdom from the Valley around a product orientation. A real love for creating outstanding user experiences. I just love learning from the folks in Silicon Valley, specifically Andreesen Horowitz. They’re outstanding.
It is bringing together multiple worlds to create what I think is going to be a better company. There’s aspects of Silicon Valley that healthcare can benefit from, and there’s aspects from healthcare that Silicon Valley needs to learn. I think we’re going to be able to bring both of that into this organization.
How do you see the company evolving, especially if interoperability starts to encroach on what you’re doing?
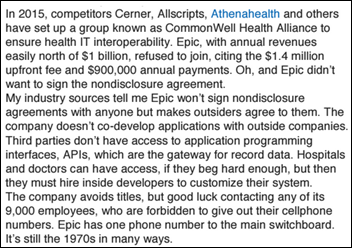
I hope that we are able to see a lot more progress on interoperability. Whether it’s through CommonWell, Carequality, or some of the other efforts happening with the established networks that may exist out there doing a lot more around clinical interoperability. I would be excited if some of that work accelerated because what that means is that there’s a switchboard or a network pulling together all of these disparate systems. Network alone doesn’t solve the problem. It needs to be network plus workflow, a really important transaction that’s delivered in a way that engages the end user uniquely.
Right now, to the extent we can rent another network, we’re certainly more than happy to do that. We partner with a lot of health information exchanges in markets where they are established and stakeholder organizations that have pulled together the data. We’re very good at taking that information and bringing it to life by getting users to adopt and love and tend to lighten the experience of using our application to solve a very important problem. But in the markets where there isn’t any network that’s the chassis, we will build it, and we have done that in many markets.
Both the network and workflow need to exist for this particular problem that we’re solving to be done well. If interoperability were to make a huge amount of progress, then that would be exciting for us, to be able to help realize the vision of the problems we’re trying to solve in healthcare that interoperability will facilitate.
Do you have any final thoughts?
I think the quote is, "I would have written a shorter book if I had more time." Building an elegant solution that seems simple requires a lot of deep understanding of the constituent organizations within the healthcare ecosystem. We’re proud that after three years, we’ve been able get to this place where what we are doing works.
We’re in six states. We have 44 more to go. We’re going to connect the whole country. We’re excited to go as fast as we can and support provider organizations out there to achieve some of the aims that they have for their organizations around improving care and lowering costs.






















































 .
.
While unsanctioned AI tools are likely causing great consternation for CIOs/CISOs, the industry has a long track record of clinical…