Jason Goldwater, MA, MPA is senior director at National Quality Forum of Washington, DC.

What healthcare problems can blockchain solve?
There are three, initially, that it has the potential to solve.
First is access to data. The way that systems have been set up in hospitals or large integrated physician networks is that the data will either reside in a centralized server or now the trend is to reside it in a cloud. That’s fine and that certainly has been effective, but you’re talking about a large consolidation of data in a centralized location.
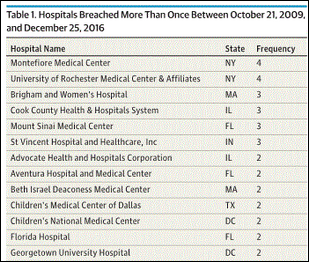
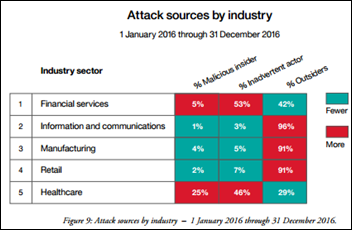
Blockchain is very different because it is what is known as distributed ledger technology. Essentially translated, that means the data is not all residing in one place. The data is residing in various different locations. Every time a change to the data is made, that change is reflected across all the locations of which the data is stored. If there are going to be threats or hacks to data, it’s easier, to some extent, to hack into a centralized location to find a large amount of patient-generated data, whereas it’s more difficult to be able to get a large amount of patient data when it’s distributed across a large number of networks.
The second thing it potentially has the possibility of helping is in the area of interoperability. That’s where most of the attention has come from with respect to blockchain. A lot of individuals are looking at this as possibly a solution to the problems of interoperability over the years, Some have even gone so far as to label it as panacea of sorts. I don’t think it’s that, but I do think it has far-reaching potential to help with interoperability because it allows data to flow in whatever syntax and whatever structure to be stored across locations.
If a provider, care team member, patient, or a patient’s family needs access to that data, the data can be delivered through the blockchain to whoever is requesting it as long as authorization has been given by the individual of where that data came from. If I’m the patient and you’re a doctor and you need to see my complete patient record to help aid in decision-making for a particular diagnosis, and I grant you access to the blockchain, then you’re able to get all of the data that has been stored. Regardless of how it is structured, you will be able to access all of that data and potentially use it.
It does not solve the problem of interpretability, which is if your system cannot read the data, it’s not computable to the system that you have. If it’s in a standard or a structure that your system cannot interpret, you’re still not going to be able to access the data, but it does allow for more free-flowing exchange of data as long as I’m authorizing you to view it.
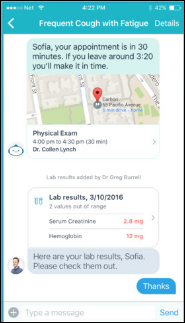
The third biggest potential for blockchain, and what I wrote about and have been speaking about, is that it can help move forward the idea of patient engagement and patient empowerment. The emphasis now is that with the amount of technology that’s around us, we’re generating more data than we ever have before, through wearable technologies and through portals. Even through genomics, with organizations like 23andMe, where you can get an entire genetic profile that you then have and can then send off to whomever you so choose.
If I’m a patient and I have data that I’m able to view, and you’re a provider and you want to view that data, or you want to examine that data and then work with me on how to improve particular aspects of my health based upon what you’re reading, we can engage in a conversation where we both have access to the very same information. You could help me interpret what that information means. I would be able to look at that data on a regular basis to be able to see if I’m making improvements. As long as I’m authorizing you to be able to examine the data, then you’re able to look at that and then work with me on aspects of health that need to be improved.
Even if we get out of the provider relationship and we get more into the performance measurement aspect of it, if I’m a patient and I have a wearable technology that measures the amount of exercise and steps that I take, if I’m on an online nutrition diary, I’m also on another website where I’m measuring my stress level and other aspects of my mental health, and I’m sending all of that information to a blockchain. If I authorize you as an administrator, provider, or a quality measurement professional to look at that data and put that into a measure, you’re able to measure the performance of the care that I’m getting. Not just at a particular episode, but over a significant period of time.
Every time that that data changes, the blockchain changes. Since I’ve authorized you to have access to that blockchain, you’re viewing that data as it’s changing. You can then view and see exactly what changes are being made in my health as a result of activities that I’m doing that may have been prescribed by you, if you’re a provider, or may have been prescribed by another entity.
Profit and legislative mandate drive much of what happens in healthcare. Who would benefit financially to move forward with blockchain, and is it implicit that the patient must control their own data?
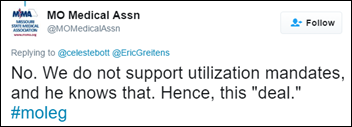
There are two incentives. You’re right, nothing really is going to change in healthcare, particularly in IT, without there being some sort of legislative intent or incentive to do so. But MACRA is upon us, so we are moving from a fee-for-service into a value-based delivery system. That has been a change that’s been evolving over a number of years. That’s not something that has just suddenly come about. That’s something that has been evolving and has been directed towards the medical associations for a long period time.
Understandably, there’s concern about that. How are you adequately going to be able to measure value-based care? You have a number of quality standards and performance metrics and you measure those during the course of an encounter to see if you have met what evidence is dictating should be done for a patient off a basis of a process — whether the structure’s in place to fit the patient, or whether the outcome is exactly what’s intended, if you have followed the correct actions. As long as that’s done, then you’re getting value for your care and the physician is reimbursed.
That data has generally either come from manual extraction of clinical records, which is starting to fade, or it’s coming from electronic health records, That has posed problems as well, because not every EHR is the same. Not every one is conforming to the same standards. Not every one is conforming to the same syntax. There’s movement in that area. There are ways of examining how that can be measured to see how we go forward, but we’re still in the beginning phases of that.
Where blockchain can assist in value-based care is that if you have a distributed ledger where data is going to be shared across a number of areas, you are authorizing the blockchain to receive the data, and you’re working with your provider to be able to look at that data on a regular and continual basis, the provider can understand what needs to be done in order to improve the outcomes of your health and what processes need to be taking place. That, in turn, then meets the value threshold for reimbursement. As such, by doing that, they’re able to continually examine and understand a patient’s health in a way that they may not have been able to before. Because it usually relied upon a patient coming in, or in some cases having a virtual visit, and they would diagnose and look at the patient then and be able to prescribe the appropriate treatment protocols.
With blockchain, you’re taking a large amount of data, personally available data that patients are generating, and being able to look at that on a regular and continual basis to drive better outcomes of care, which then in turn drives value. That’s the first thing.
The second thing is the market dynamics are changing. Twenty-some odd years ago, it was a pretty basic concept. A patient would come in, they would say, "This is wrong with me," or they would come in for a regular checkup. They would be diagnosed and the provider then would recommend the appropriate medications, labs, treatment protocols, whatever it may be. The only data that was generated at that point was the data that was generated during the encounter.
That is not the case any more. The data is being generated everywhere. There is more data available for a patient than there has ever been. It’s not just the data that would come from wearables, portals, and smartphones, it’s also the data that’s available on social media sites, where patients write very eloquently about their health. It’s available through validated instruments that they have filled out over the course of their care. It’s available through sites like PatientsLikeMe that store an abundance of patient-generated data. There’s more data available. Patients have more control and more access to data than they have.
How, then, do we take that bolus of data and turn it into something where we can use it for improvement of care? You could store it all in one location and access it when it’s needed. That’s what people are doing, and there’s nothing wrong with that. Having cloud-based storage allows you to access that data and those applications as a service, so when you need it, you get it.
Blockchain allows the data to be distributed across a variety of locations, but the benefit of that is that the patient and the provider both have access to it. I have to authorize you to look at that, and every time that data changes, every time on a daily basis, if things begin to change — my heart rate changes, my blood pressure changes, my mood changes, I’m not exercising as much, I’m not taking the medications I need to be — that data is updated and sent to the provider on a regular basis.
If the provider understands that they’re going to get that data on a regular basis and that it will aid in the decision-making, that they can put that data into an EHR and send that data around to provide access to that patient’s care, and understand that that data is then available to not only aid in decision-making, but to provide the impetus for better decisions — because the value based market is demanding that — then certainly that’s going to be an impetus to push towards better interoperability and better use of the data.
Three things come to mind as barriers. The terminology and syntax issues among EHRs, the need to convince EHR vendors to modify their systems to interact with the blockchain, and the lack of a unique patient identifier.
I’ll start with the second one. There’s no need to rip and replace. Blockchains are peer-to-peer networks. It’s a distributed ledger technology, but it’s peer-to-peer, It’s shared through numerous different systems that generate data. If you have a public blockchain – there’s plenty of them, like Hyperledger, which is written about and spoken about as an open source blockchain – EHRs serve as the access control point for what information is going to be sent to the blockchain. That would have to be done with the consent with the patient, obviously. There’s no need to be ripping and replacing. It’s a matter of, are you going to grant access to the blockchain through your system? Are you going to then engage the patient? There’s going to be continual contributions of data, That data is stored in a blockchain in a chronological, linear order, and then as it’s updated, it’s changed. There’s no real need to be replacing systems.
The syntax, the semantic structure of data, and how that data is presented is not something the blockchain universally can solve. It’s not something that you can force the issue from. But the dynamics of the market are changing to the point where value-based purchasing is going to become the norm. It’s not something that’s just going to be an option. There’s going to be a bigger demand and a better drive towards improved outcomes of care and better processes of care, but the emphasis is really going to be on outcomes. If you’re looking at the potential of blockchain to assist that, then you’re talking about being able to store significant amounts of data on this peer-to-peer network where that data is being generated from patient devices, but also being generated from an EHR, and that patient is able to work with a provider to control that access and flow of information.
Does it solve the problem of standardization? No. Does it lend itself to creating a better environment for improving outcomes for value-based care that in and of may change it? Possibly, yes.
To your third point, there’s no unique identifier. You’re correct — there’s not. Blockchain doesn’t solve the problem, but when data is uploaded to the blockchain, a patient has to authorize that access and they authorize the provider to view that. A digital fingerprint is created between the provider and the patient. That fingerprint contains all of the data attributable to that patient that’s being uploaded from the variety of devices or technologies in which the provider and the patient will use to improve care.
So, it can be attributable to a patient because a fingerprint is created in which only that block of data on the chain can be viewed by the provider of the patient, but it does not create a unique identifier. It does create a unique fingerprint. When you talk about financial transactions of bitcoins, which is where blockchain really came from, there hasn’t been any issue to date with respect of bitcoins being attributable to the wrong individual. They’ve been attributable to the individual that has the fingerprint that’s associated with it. The theory is that the same thing would work in healthcare. Has that been tested? It’s been tested in a laboratory environment. Has that been tested in a actual market? No, not yet. At least not to my knowledge it hasn’t.
What should health system CIOs and technology vendor executives be doing now with regard to blockchain?
They definitely need to be interested in it. I would not say at this point they need to immediately start implementing a blockchain and sending data there. But what they need to understand, first and foremost, is the scalability. They have a system now that stores records and stores information about patients. Whether they can send that information to other providers or members of a care team that are responsible for that patient, I don’t know.
Does blockchain provide enough scalability for them to be able to increase the amount of data they can have for a patient? Does it provide the ability to exchange data across partners that could access that where they could either add to the blockchain or they could use the blockchain to help provide care for the patient? Because if it’s going to come down to value-based services and greater outcomes of care, how can blockchain, from the scalability standpoint, be able to improve those outcomes for your environment, be able to improve outcomes for that patient, and be able to meet the dynamics of this new value based marketplace?
The second is to start to look at the access security issues with respect to blockchain. That’s always going to be a paramount issue. The real thrust right now is for patients to have access to data. It’s the patients’ data. They should have access to it and they should be able to engage in a shared conversation with their provider using the data to understand their care better and for the provider to work with them on what needs to be improved. Understand how blockchain can improve access security between the provider getting data and the patient getting data and how that dynamic would change. How that dynamic would improve outcomes, enhance patient care, and enhance patient engagement, which is another part of this value-based dynamic.
They really should also look at their data and their data privacy. How is their data stored? How is their data encrypted? How is their data protected? Is it vulnerable? Does it have the potential to be accessed and hacked? Is there a potential for a breach? No technology will solve that completely, but blockchain provides a greater ability to be able to protect data because it’s not stored in a centralized location. It’s stored in a peer-to-peer network.
The EHR on the blockchain can be access control manager. Who gets access to the data? What data flows into it? Does that significantly improve what they already have? If it does, then it’s a solution worth considering, because it can scale upwards in the ability of for them to not only gather more data, provide more data to the patient, and be able to exchange more data. It not only addresses better access security between the provider and the patient, but it may also improve privacy overall. Rather than the data being in a centralized location — whether it’s a cloud storage system or whether it’s in a centralized server — a distributed ledger provides a better mechanism by which data privacy can be maintained.

















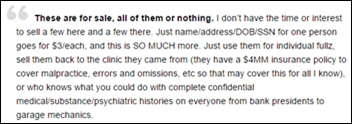



































































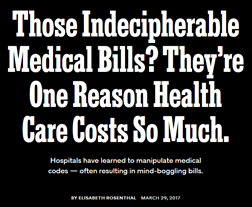


I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…