News 8/25/17
Top News
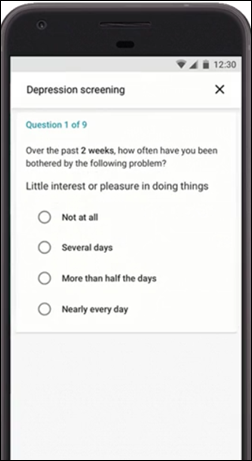
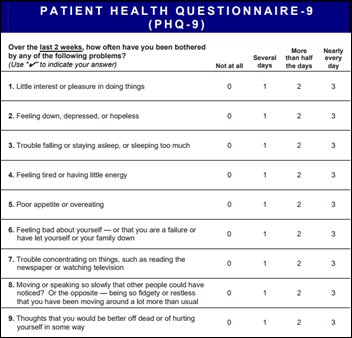
Google offers users who search for “clinical depression” on a mobile device an option to take a PHQ-9 online depression test, offered in partnership with the National Alliance on Mental Illness in hopes of increasing the percentage of depressed people who seek and receive treatment.
Reader Comments

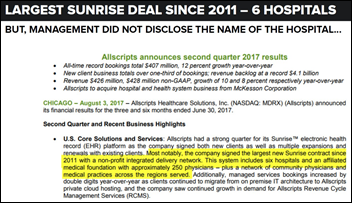
From CinderFella: “Re: Verity Health. HIStalk had the edge on Hedgeye’s analysis over a month ago, with a reader commenting on the NantHealth purchase of Verity saying that it would buy ‘his Nant-whatever stuff’ and Allscripts products. The real story is that Verity scrapped a year’s worth of evaluations as it was looking to implement a new EMR. The selection process was still finalizing and a go forward choice was TBD, but it wouldn’t have been Allscripts.” I’m a Wall Street lightweight, but I would be uncomfortable as a shareholder of either company with the Allscripts investment in NantHealth, Patrick Soon-Shiong’s personal investment in Allscripts, and now NantHealth’s rumored pushing of the products of both companies on non-profit Verity, especially given that NantHealth seems to have made quite a few “sales” of its own products that looked more like mutual back-scratching than objective purchasing decisions that suggest market momentum. I suppose Verity being forced to choose a product it didn’t want is a legitimate sale, if indeed they have lost that choice, but it smacks of desperation from both companies. Maybe Allscripts also worries about that perception, too, since it hasn’t named Verity as the mysterious new client it signed.
From HIE Watcher: “Re: Informatics Corporation of America. Hearing it is being acquired by the SSI Group.” Unverified. I’ve sent an inquiry to ICA with no response so far.
From Orange Vest: “Re: LinkedIn. How do you choose which connection requests to accept?” I pretty much accept all invitations, declining only those that are obvious scams (like someone who works for a Chinese air conditioner manufacturer who has no overlapping connections), although sometimes that opens me up to annoying messages from recruiters or overzealous salespeople who I squelch quickly. I really don’t do anything with LinkedIn except (a) look up people who have changed jobs, and (b) sometimes check to see if somebody’s connected with me or is in the reader-started HIStalk Fan Club to decide if I’m willing to reply to their email.
From Dreydel: “Re: Devoted Health. I don’t have access to the full story, but Todd Park’s LinkedIn says he’s the founder. I bet other ex-Athena execs are involved.” I don’t pay for WSJ either, but Athenahealth co-founder Todd Park’s LinkedIn says he’s the co-founder and executive chairman of insurance startup Devoted Health.
From Publius Tullius: “Re: Epic in Denmark’s Capital Region. The projects are going so poorly that Epic was cut in the first round of the bid process to support the Southern Region. Stories go back to February related to project under-scoping, missing functionality, and budget overruns.” PT provided a ton of links to Danish sites describing Epic project problems, with some Google-translated headlines above.
HIStalk Announcements and Requests
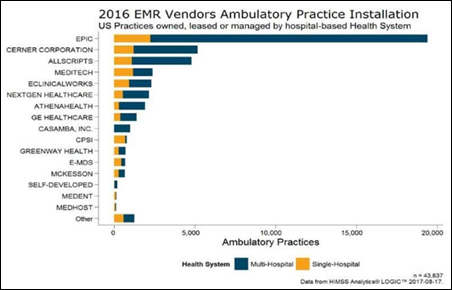
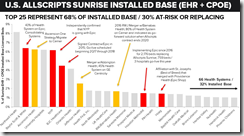
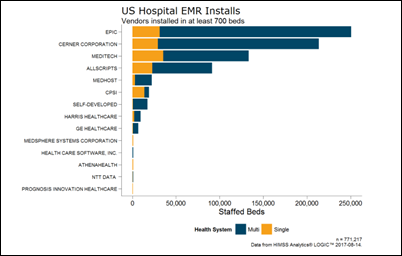
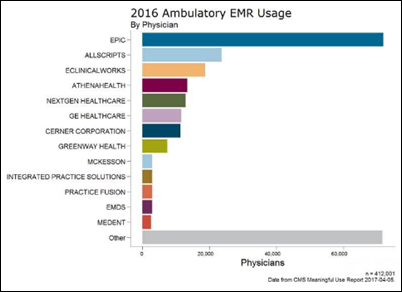
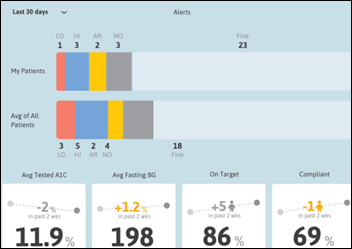
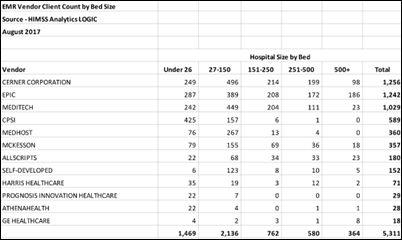
Blain Newton of HIMSS Analytics sent over another interesting analysis, this one from its Logic database that shows the EHR user count of physicians who are employed by, leased, or managed by health systems. Epic has a four-to-one lead over Cerner and Allscripts in doctor count, nearly equal to all other vendors combined since its customer base is mostly huge health systems. That also means that Epic has displaced a lot of EHR/PM vendors in practices as hospitals acquired them and put Epic in. It also makes InterSystems very happy since they license Cache by concurrent user.
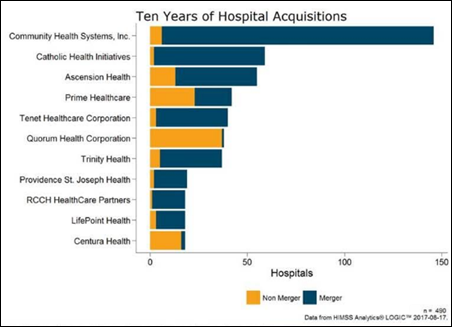
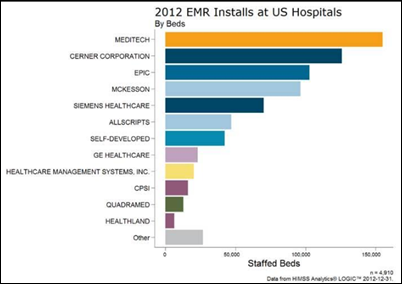
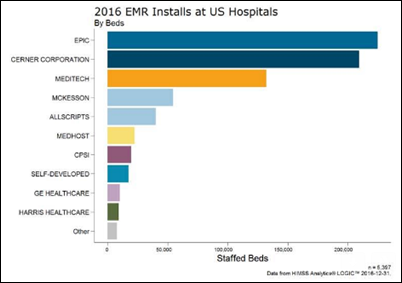
Blain also provided this graph showing those organizations, both for-profit and non-profit, that have made the most hospital acquisitions in the past 10 years. Such acquisitions drive a good bit of the EHR market as acquired hospitals are moved to the corporate EHR standard.
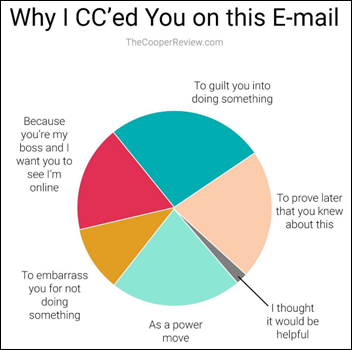
This, as they say, resonates with me.
So does this, since I am always baffled that more people play the lottery when the prize goes up. Are these folks who couldn’t be bothered for only $100 million?
This week on HIStalk Practice: Alaskan providers share challenges, triumphs with HHS Secretary Price. Allscripts makes it easier for physicians to participate in clinical trials. The Institute for Women’s Health succumbs to keylogger virus. Wellpepper CEO Anne Weiler shares why virtual assistants and interactive mobile treatment plans are poised to meet consumer healthcare expectations in a big way. LifeWorks NW VP of Clinical Services Mark Lewinsohn expects new population health management technology to boost its participation in the national demonstration project for Certified Community Behavioral Health Clinics. Behavioral healthcare stakeholders lament telemedicine’s slow progress in MA. Petaluma Health Center becomes data-driven FQHC. DoD honors ChartLogic. Dispatch Health expandsto Arizona. In a new monthly series, PRM Pro Jim Higgins outlines the ways in which physicians can use patient relationship management technology while still maintaining the human touch.
I’m disappointed that nobody bothered to make an Eclipsys-related eclipse pun.
Listening: new from 29-year-old Minneapolis-based hip hopper Lizzo, whose Missy Elliott-style brash confidence includes more explicit lyrics than I like, but I overlook that because her music is a joyous, soulful bridge between the late 1960s Motowners and today’s rappers. I’m also listening with nostalgia to the unparalleled R.E.M., which ceased to exist in its original configuration as a foursome and one of America’s greatest bands 20 years ago, their unexpected high harmonies still giving me chills last night when the family chain restaurant I was in surprisingly played “Fall On Me” on its canned music system.
Webinars
September 13 (Wednesday) 1:30 ET. “How Data Democratization Drives Enterprise-wide Clinical Process Improvement.” Sponsored by: LogicStream Health. Presenter: Katy Jones, program director of clinical support, Providence Health & Services. Providence is demonstrating positive measurable results in quality, outcomes, and efficiency by implementing clinical process improvement solutions in arming operational and clinical stakeholders with unlocked EHR data. Providence’s army of process engineers use their self-service access to answer questions immediately instead of waiting for reports to be written and double checked for possibly inaccurate information. The presenter will describe practical applications that include antibiotic stewardship, hospital-acquired infections, and comprehensive knowledge management.
Previous webinars are on our YouTube channel. Contact Lorre for information on webinar services.
Acquisitions, Funding, Business, and Stock

Agfa-Gevaert is considering spinning off its health IT business that includes vendor-neutral archive, PACS, image sharing, data aggregation, patient engagement, and digital radiography.
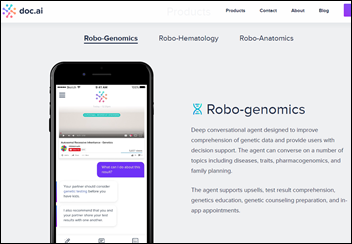
Startup Doc.ai comes out of stealth mode in describing its AI-powered “silicon doctors” medical dialog system. Its CEO is the co-founder and former CEO of Scanadu, which seems to have fizzled out following the retirement of its Tricorder-like vital signs device that earned tons more press than it deserved as technical limitations kept dumbing it down.
Sales
Pomona Valley Hospital Medical Center (CA) chooses Imprivata’s biometric positive patient identification solution.

The VA and DoD sign a 10-year contract with Fujifilm Medical Systems USA to make the company’s Synapse enterprise imaging portfolio available to government healthcare providers. The maximum contract value is $768 million.
People

Grattan Smith (RelayHealth) joins Loyal Healthcare as VP of business development.
Announcements and Implementations
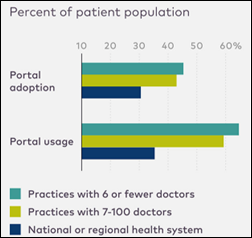
An Athenahealth survey finds that patients of small physician practices are heavier patient portal users than those of regional and national health systems, with respondents offering these suggestions to improve use:
- Let patients know that the portal is the primary way the practice will communicate with them.
- Help patients sign up while they are in the office, creating an email account for them if necessary.
- Review their labs and chart entries from the portal on a large monitor during their visit.
- Remind new patients to register on the portal before their first visit.
- Commit to responding to patient questions within 24 hours.
- Use services like Solutionreach that text patients when their lab results are ready to view on the portal.
Government and Politics

The President’s political appointees have turned HHS into a remarkably shrill and partisan White House lapdog, loudly criticizing the laws they swore to uphold. The latest example is this statement from HHS Principal Deputy Assistant Secretary for Public Affairs (and former Koch Brothers employee and aide to former Governor and now VP Mike Pence) Matt Lloyd, who instead of encouraging healthy people to sign up to create better ACA risk pools, dutifully does his part to perpetuate the “let it fail” agenda with campaign slogans instead of responsible statements:
Obamacare failed to create a thriving, competitive market that offers the kind of coverage people want to buy at prices they can afford. On Obamacare’s exchanges premiums continue to surge, insurers continue to abandon wide swaths of the country and choices continue to vanish – an unfortunate reality for the American people who are required to buy Washington-approved health insurance or pay a fine.

The Supreme Court is reviewing a lawsuit that argues that Google’s trademark of its own name should be nullified because “Google” has become a synonym for “searching the Internet.” The term “genericide” refers to former trademarks that became plain old words because of their non-specific usage, among them “thermos,” aspirin,” and “videotape.”
Privacy and Security
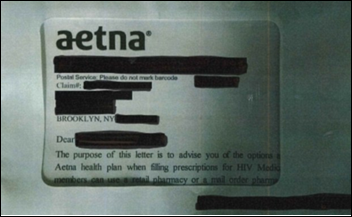
Aetna exposes the HIV status of 12,000 patients in several states by mailing HIV medication prescription information in envelopes that contain an overly large window.
Other

MD Anderson Cancer Center (TX) credits its cost management efforts – which include laying off 800 employees – for several straight months of profitability that have swung it into the black for the fiscal year, digging itself out of a $169 million hole.

Fast Company magazine covers the drug and blood delivery drones being used in Rwanda, where startup Zipline has in its first 10 months’ of service made 1,400 deliveries of 2,600 units of blood using its 15 drones, 25 percent of those involving life-saving emergencies. The service will go live in much-larger Tanzania next year, hoping to make it “the first country in the world to achieve 100 percent in-stock rates at all health facilities and hospitals” for anti-malarial drugs, HIV medication, vaccines, and insulin.

A nursing home owner pays $13 to acquire a Missouri hospital that BJC HealthCare bought and then closed nine months later, probably hoping that BJC is being overly cautious in warning of potential asbestos problems and high maintenance costs.
Pharma bro Martin Shkreli, who was famously banned from Twitter for his creepy harassment of reporters, is buying Internet domains that are associated with the names of journalists who have criticized him, then putting up web pages that mock those people. He then offers to sell them back the domains for several thousand dollars, an extortion-like scheme not unlike his Turing Pharmaceuticals pricing strategy in being simultaneously despicable yet legal. Shkreli says, “I wouldn’t call these people journalists. They are the unwitting recipients of liberalism subsidy from large media and telecom companies … only a few notches above the white supremacists we hear so much about these days.”
Colorado and Maine have enacted laws that require veterinarians to check pet owners in doctor-shopping databases in hopes of detecting drug users who obtain addictive drugs through their pets. Some states require vets to perform such a check, while two-thirds of states explicitly prohibit it, with the president of the California Veterinary Medical Association explaining, “I’m a veterinarian, not a physician. I shouldn’t have access to a human’s medical history.”
Weird News Andy follows up on my mention of CuddleCot, observing that people took photos of their deceased children back in Victorian times because they were unsure of the then-new technology’s role in memorializing their dead loved ones. I recall a movie that led off with a series of photos like these, where it brilliantly added no explanation until it became obvious about halfway through what I was looking at. Memento mori.
In England, a hospital CEO is criticized for refusing to accept $3,200 donation for ECG equipment, saying that the fundraising team of men who’ve run an annual hospital bed-pushing contest for 25 years are demeaning nurses by dressing in their female uniforms.
Sponsor Updates
- Nuance announces that 600 healthcare organizations chose Dragon Medical One in the past year, also adding 25,000 users in the past 90 days.
- EClinicalWorks will exhibit at the NACHC Community Health Institute & Expo August 27-29 in San Diego.
- Hayes Management Consulting will exhibit at the AHIA Annual Conference August 27-30 in Boston.
- People: Laura Kanov joins HBI Solutions as SVP of product strategy.
- Impact Advisors donates more than 5,000 personal care products to active troops overseas.
- Ingenious Med will exhibit at the SHM-VA Chapter Meeting August 30 in Virginia Beach, VA.
- InterSystems will exhibit at the annual SHIEC Conference August 27-30 in Indianapolis.
- ConnectiveRx is a finalist for the 2017 PM360 Trailblazer awards.
Blog Posts
- While Not Perfect, Bundles May Still Be Our Best Bet (ECG Management Consultants)
- How technology empowers healthcare providers to achieve accessibility, affordability and availability (Elsevier Clinical Solutions)
- Brown Clinic: Superusers Building Value (EClinicalWorks)
- How to Boost Physician Engagement with Claims Data Insight (Evariant)
- Rethinking Customer Relationships (Access)
- Will I be able to advance in my career as a consultant? (Nordic)
- Reimbursement Analysis – A Critical Component to the Implementation of New Services (Hayes Management Consulting)
- Healthcare Digital Transformation: What, Why & How? (Part 3) (The HCI Group)
- Changing the Paradigm of Patient Communication (Healthgrades)
- Your guide to the MACRA 2018 proposed ruling (Meditech)
- One Moment That Mattered – A Physician’s Perspective on Patient Education (Healthwise)
- Change is Constant, How Do You Manage It? (Iatric Systems)
- Considering Telemedicine? Don’t Be Afraid. Funding is Out There. (Impact Advisors)
- Top 5 Tips When Using a Clinical Service Desk (Leidos Health)
- Protecting medical devices to build cyber resilience (Imprivata)
- Best Practices for Maximizing Your Healthcare Marketing Effectiveness (Influence Health)
- Final Countdown: Annual Thought Leadership on Access Symposium 2017! (Kyruus)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne, Lt. Dan.
Get HIStalk updates. Send news or rumors.
Contact us.


































































I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…