HIStalk Interviews Eric Ritchie, COO, Minnie Hamilton Health System
Eric Ritchie is COO of Minnie Hamilton Health System in Grantsville, WV.

Tell me about yourself and the organization.
We’re a Federally Qualified Health Center that owns and operates a Critical Access Hospital and rural health center in Grantsville, West Virginia. It’s an unusual designation, only of about one of three in the country where an FQHC owns and operates a Critical Access Hospital. I’m originally from the area that we service.
Minnie Hamilton has been operating this way for approximately 21 years. We operated as a standalone clinic prior to 1996 before taking over responsibility for the recently-closed Calhoun General Hospital, which had serviced the area prior to that for the previous 30-plus years.
What are your biggest challenges in running the health system?
The biggest challenge is definitely related to our rural location. We service an area that doesn’t have a lot of industry — actually it has no measurable industry — so it is an aging population. A lot of the younger generations, to provide a lifestyle for themselves, move beyond our service area. Our average patient age goes up every year, according to the demographic.
The lack of infrastructure that comes with being in rural West Virginia makes it challenging. Your patients have difficulty getting out to get their healthcare needs satisfied. When they do come to our facility, if they need a more specialized facility or a bigger hospital, there’s always a logistical challenge getting them out in a timely manner to meet those emergent situations.
The rural location is probably our number one biggest challenge and the disadvantages that come with that. Definitely in the state of West Virginia, it’s well-documented that our infrastructure, from an IT standpoint, is challenged. We also deal with that as well.
What are your most significant IT systems?
When we selected Athenahealth as our EHR, it was our goal to try to get it all under one umbrella from an IT standpoint. Athena is primarily it. We have standalone dental software that runs our dental clinics. We also operate a long-term care facility that has its own system. Beyond that, it’s just our traditional phone system. We have a partnership with Microsoft that we leverage their Office suite free of cost because we’re a not-for-profit.
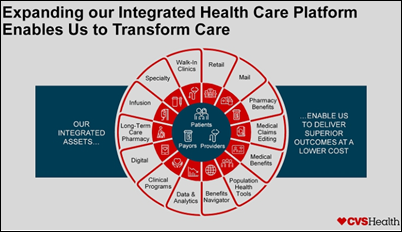
What are you doing with population or community health?
We are the continuum of care for most of our patients. We put a lot of focus on identifying, as our patient demographic ages, what their predictable needs will be in the coming years. As a facility, we have evolved over the last 20 years, as our demographic has aged, to make sure that we are providing services that prevent them from having to make that hour, hour and a half commute.
A big population in our area has diabetic needs, so we’re looking at what’s coming down the pike. A need for dialysis, more so than there is right now. That was the reason why we opened the dental clinic, to address the younger population that does exist. The long-term care was another one of those solutions.
We have a pretty simple formula. We do quarterly analysis on the referrals that we are having to send out to other facilities because we don’t provide a service. When we see a need rise up to the level affecting a measurable percentage of our population, we start exploring ideas on how to bring that service here locally, whether it’s something that we provide under our umbrella or that we simply provide space for another entity to come in and perform those services here.
You are surrounded by WVU Medicine and the trend nationally is that the big systems are getting bigger. How do you see the future of Critical Access Hospitals, both in West Virginia and across the country?
It’s very interesting and a popular topic among the Critical Access Hospitals when they get together and talk. In West Virginia, we see two predominant, large entities that are acquiring Critical Access Hospitals. WVU Medicine to the north, which is acquiring different practices up there, and then Charleston Area Medical Center to the south.
We have a good relationship with both. Right now we’re partnering with WVU Medicine, where they are sending specialists to our facility to hold office hours. They take care of the billing, so they’re not working under the Minnie Hamilton umbrella, but they are bringing much-needed services to our areas, eliminating the need for our patient population to drive extended miles to receive that service.
It really comes down to, in our experience, open communication. This is what our needs are. This is how we can help each other. Our loyalty stops at our patient population, so whatever is in the best interest of that patient population, we are going to use that as our guiding light to determine how we should move forward.
There’s always a balance where a big health system could provide resources, but they if they were to acquire the hospital, they might decide it’s not worth keeping open or they might not respect its original mission.
Based on the conversations that we’ve had with those larger entities, I think there is a real shift in the view of how a larger entity partners with a Critical Access Hospital. Our patient population is predominantly Medicare or Medicaid. That’s a financial benefit for us because of being a Federally Qualified Health Center. It doesn’t make as much sense financially for a bigger entity to become servicing a population that is predominantly Medicare or Medicaid.
What everyone is starting to realize, or at least in our experience, is that it makes more sense if we can provide the care here locally and keep that patient population close to their home place. But we are dependent on those bigger entities to provide the knowledge and the skill sets. Rather than taking over and starting to operate a Critical Access Hospital under their umbrella, I think it benefits them in the long run if they can simply be recognized as a partner to an existing Critical Access Hospital who is servicing the rural part of America. But at the same time, not overwhelming their own systems with a patient population that they can’t handle.
They want those beds. They want the ability to make sure that care is being provided. But they can’t afford to continue to expand and just increase their bed count. It makes more sense for a standalone entity like Minnie Hamilton to take care of the daily, routine illnesses or chronic illnesses that can be monitored and managed. When that special occasion comes up that exceeds our skill set, we have a direct line to a solution that can come and be a part of that care team.
The advantage big systems have is that they have other sources of revenue, while you are at the mercy of what happens in Washington, DC.
You really are. That is a burden carried by all Critical Access Hospitals. Even the bigger entities have that concern, but our reimbursement and our ability to remain operational goes as Congress and the legislature decide to fund the healthcare programs. We can in no way be profitable without that federal supplement. We just don’t have the volume to generate the revenue that’s required to run the facility as we have it set up now.
The alternative is that if a facility like ours ceased to exist in our service area, we’re looking at a two-hour time lapse for an emergent situation. We all know what numbers end up being when you’re taking 120 minutes to respond in an emergent situation.
Government officials, elected officials, those bigger entities all want to be a part of a solution that allows rural America to continue to be served by a staff capable of taking care of an emergency situation, as well as those that have chronic illness or the routine acute type settings. So they aren’t required to travel an hour and a half or two hours for care.
You had some previous problems with revenue cycle management and the cost of your IT systems. What are the lessons learned from that experience?
With a smaller entity like Minnie Hamilton or many of the Critical Access Hospitals, you need to stay very current on the rules and regulations governing reimbursement. Insurance companies continue to become more and more business-like in the sense of identifying ways and criteria that all of us have to be well-versed in and know how to apply it to maintain a level of reimbursement that we have historically experienced.
One of the ways that Minnie Hamilton is navigating that right now is that we’re making sure that we partner with vendors that bring something to the table with regards to knowledge of those ever-evolving rules and regulations. We feel it’s best for us not to bear that responsibility solely by ourselves. There’s just too much at stake.
You make partnerships. You look for vendors who have a vested interest in not only understanding those rules and regulations, but helping you as the client understand those rules and how best to leverage them. Keeping you compliant with the ever-changing regulations that are being passed down annually, whether it’s MIPS, MACRA, UDS reporting, or HEDIS reporting. For us, that is the guiding principle behind identifying possible vendors and then ultimately selecting vendors. That has to be a component of that relationship.
Given the challenges your health system has, what makes you want to keep coming to work every day?
We’re fortunate at our facility because we’re smaller. Our executive team at Minnie Hamilton all grew up within 30 miles of this facility. The patients we are serving are our family members, extended family members, or friends of family members. It’s easy for me, and really all of our staff, to recognize why we do what we do and why we deal with the headaches that we deal with.
In my experience in West Virginia, even in the bigger entities, a lot of the folks that I deal with on a daily or weekly basis are from the area or are from areas that have a lot of similarities to the demographic makeup of the state. At the core, almost anyone I’ve met in healthcare started out at more of an introductory level. At the heart of it, they’re motivated solely by that moral compass of just wanting to do right by the patient population.

































































I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…