Newsy Items

Analytics vendor Inovalon will acquire competitor Ability Network for $1.2 billion, doubling the 2015 investment of the latter’s private equity owners.

The Wall Street Journal reports that Cigna is close to buying Express Scripts for at least $50 billion as industry consolidation runs rampant. Wow.

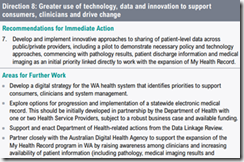
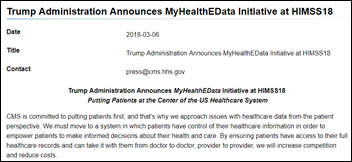
HHS Secretary Alex Azar lays out – in an admirably direct manner – his vision of the transition to value-based care in a speech to a hospital trade association, of which I’m paraphrasing. Note that he’s basically throwing down the “no more business as usual” gauntlet to the people who will be most resistant to the planned changes. He previewed some of the the items covered in Tuesday’s presentation by CMS Administrator Seema Verma and White House Senior Advisor Jared Kushner. High points:
- The hospital industry has dragged its feet on being paid for value and health systems are charging too much without delivering good outcomes.They also haven’t done enough to manage chronic diseases.
- The White House and HHS are not afraid to disrupt the status quo “simply because they’re backed by powerful special interests.”
- HHS will emphasize giving consumers control of their health information via interoperable, accessible health IT. He said, “Patients ought to have control of their records in a useful format, period. When they arrive at a new provider, they should have a way of bringing their records, period. That’s interoperability. The what, not the how … Too often, doctors and hospitals have been resistant to giving up control of records, and make patients jump through hoops to get something as basic as an image of a CT scan. The healthcare consumer, not the provider, ought to be in charge of this information.But we do know that the barrier is not always the provider’s decision to shield that information. Sometimes it’s that there aren’t systems for easily disseminating it, and we aim to work with the private sector to open up avenues that will empower patients.”
- He calls for transparency in drug pricing at all levels.
- Azar bluntly concludes, “Our current system may be working for many. But it’s not working for patients and it’s not working for the taxpayer … This won’t be the most comfortable process for many entrenched players. But those who are interested in working with us to build a value-based system will have the chance to take advantage of a market where consumers and patients will be in charge of healthcare.”

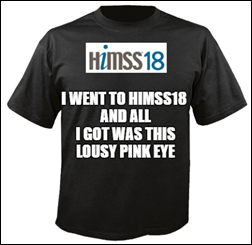
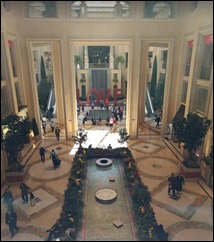
Today was overcast and cool, not that it matters much when you’re inside a windowless casino complex jam-packed with way too many people.
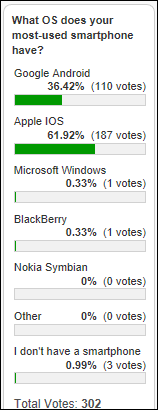
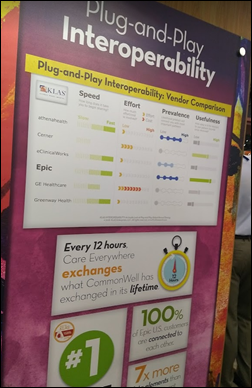
From New Health IT Investor at HIMSS: “Re KLAS. On the first day of HIMSS, I inquired about KLAS and three times got the same word from vendors – extortion. I asked Epic’s competitors and they say Epic pays nearly $6 million a year. Tonight I looked up KLAS’s public declaration of income to the VA in March 2017 and they stated $12M in annual revenue. So half of KLAS’s income is from Epic?” I disagree that it’s extortion. Vendors make a business decision to pay KLAS what amounts to advertising fees expecting to make a return on that investment in the form of sales. KLAS also claims to be the voice of the customer, but only an incompetent vendor would need a third party to tell them what their customers think. No major vendor has had the nerve – so far – to break ranks and stop supporting a system they complain about, so KLAS just keeps happily minting money. I would be shocked if KLAS only makes $12 million per year and even more so if Epic pays them $6 million. I’ve asked a few folks to guess at KLAS’s revenue and they usually say maybe $20-30 million, with those same guessers thinking Epic pays maybe $1 million. But’s all speculation since, unlike the “Consumer Reports” to which KLAS is often inappropriately compared, KLAS is for-profit, is not financially transparent, uses statistical methods that range from unstated to unscientific, and makes most of its revenue from the same companies it claims to objectively review. KLAS is not evil, they’ve just created a great business based on vendor insecurity that paying KLAS increases sales, which I would argue is more perception than reality. In fact, it would be fun to commission a truly independent and statistically valid survey to determine if providers actually used KLAS services as a major factor in their most recent system purchases.
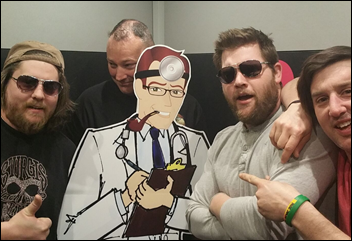
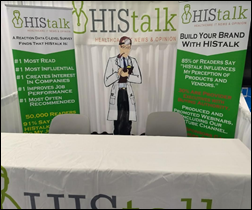
From Kodak Moment: “Re: HIStalk booth Polaroids. Saw those in a tweet – what are you doing with them?” I really don’t know – Lorre and Brianne are always full of surprises, some of which I like.

The Oneview Healthcare folks confirmed that HIMSS did indeed shut down their live Irish band and dancers in the exhibit hall Tuesday. They told me they had done the same performance for the past five HIMSS conferences without any problems, but I’m sure someone with a bigger booth complained about the noise (or that they were losing visitors to a more interesting booth). The company was pretty funny in tweeting out a doctored-up invitation in which the band and dancing references were redacted, but reminding everybody that the Guinness would still be flowing (which I confirmed in having one Wednesday afternoon).
A reader complained that the pictures I run are too small. It seems simple to just make them bigger, but I guarantee I’ve thought of all options and their pluses and minuses. I’ll explain after HIMSS and open it up to a reader vote. In the mean time, I’ll make the pictures bigger for the HIMSS posts and that will probably trigger an immediate minus – more scrolling will be required and people hate that, especially on mobile (which is why I sometimes but not always make the pictures bigger, depending on what’s in them). Part of the problem may be that I’m working from a laptop and my screen captures might not be as crisp as usual. I admit that I have no idea how that works.
Lorre said three new HIStalk sponsors have signed up in my “Cellar Dweller Special” bonus offering. Thursday is the last chance for those who could use more, less-expensive exposure over a full year than a three-day downstairs booth can provide. We have a good time with our sponsors, and while they don’t get influence over the editorial side of what I do (screw up and I’m going to say so), a some companies were unknown before their introduction as a new sponsor.
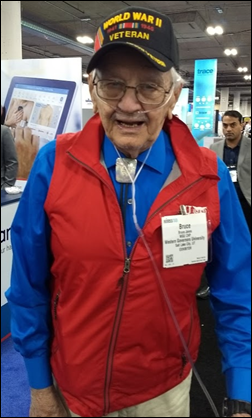
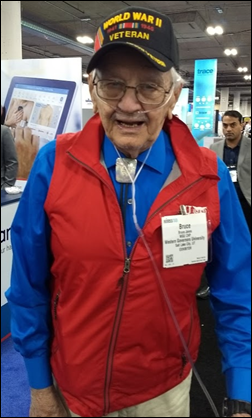
This will be the high point of the week for me. I was puzzled to see an elderly man walking slowly but ramrod-straight down the aisle by our booth wearing a “World War II Veteran” cap. I caught up with him and asked about his service. Bruce was a US Navy Seabee deployed to the Pacific theater, serving as part of the construction team that was tasked with building the structures required for the planned invasion of mainland Japan. I thanked him for his service – choking up a little bit thinking about what he has seen and done in his long life – then asked him what he was doing at the conference. He said his daughter is the academic VP of the college of health professions at Western Governors University (exhibiting in Hall G) and she brought him along as her guest. What an honor to have him at the conference – it was heart-warming to see people who were working the booths come out to shake his hand. I don’t know how old Bruce is, but I’m sure the memory of being shipped out as a young man for an assignment he almost certainly wouldn’t survive remains vivid even 75 years after the fact.

Optum was making donations for each attendee who colored in a section of their graphic, although I got so engrossed with trying to say inside the lines that I forgot to write down the details.
It seems like half the booths are, at any given moment, stuffed with video and/or audio recording equipment and people. You couldn’t walk 50 feet without trying to dodge tripods, stay out of a camera’s line of sight, or watch two people sitting on stools conversing on camera. I don’t know who will watch all that video (not me, I guarantee), but maybe I’m just out of touch with those who can’t consume content unless it’s dumbed down to short videos. I’m also questioning whether there’s enough people who have useful wisdom to fill up all that airtime, given the skimpy resumes some of the folks who couldn’t wait to start tweet-bragging that they had been asked to share whatever it is they know.
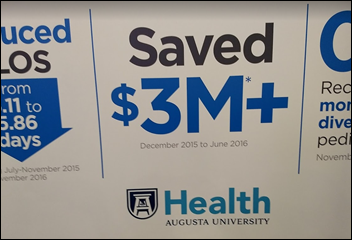
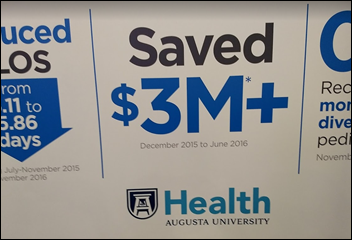
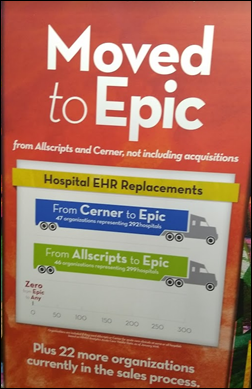
Cerner used the outside walls of their booth for promotional posters a la Epic, but instead of KLAS excerpts, Cerner instead highlighted customer successes.
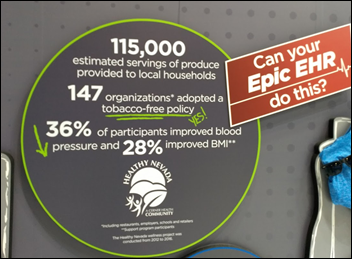
Cerner also took off the gloves inside its booth, deviating from never referring to Epic by name (“our primary competitor”) to even copying Epic’s logo.
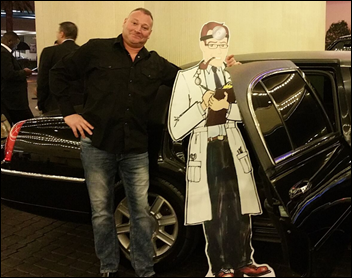
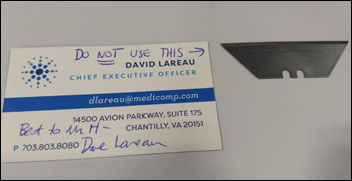
I asked this guy if he was having a good show, but he told me to beat it.

The hall has all kinds of nooks and crannies devoted to special interest tracks. I accidentally ran across this Innovation Live stage and listened in to someone’s case study (I think it was Albuquerque-based Twistle, which offers a patient engagement app).
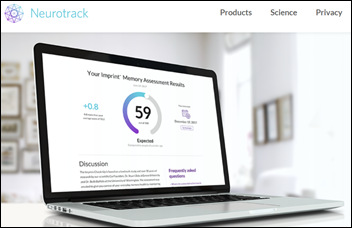
Stuck back in one of the innovator areas was Neurotrack, which uses a mobile device’s camera to track a user’s eye movements when various kinds of photos are displayed over a few minutes. It’s apparently good at identifying people who may be more likely to have dementia 3-5 years down the road, giving them enough time to implement lifestyle and mental exercise changes. The company has an investor from Japan and has made some inroads there, since insurers there pay twice for Alzheimer’s (once upon diagnosis and again at death) and thus will pay for early detection that may support prevention.

Think all the cool kids are in the upstairs exhibit hall? We got Uber in Hall G, y’all.

Another great ice sculpture, provided that you see the point of making ice sculptures (and I admit I kind of don’t, especially when they are made like a giant, shaped ice cube instead of hacked from a block).

Athenahealth Chairman Jeff Immelt and CEO Jonathan Bush were hanging around the rather dead Athenahealth booth that’s about as far from the main exhibit hall thoroughfares as you can get.
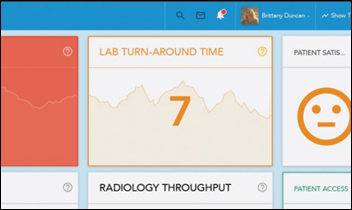
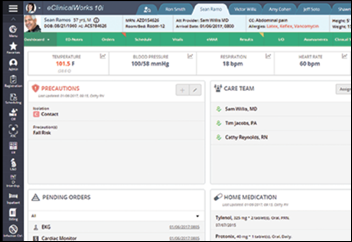
I stopped by the booth of South Korea-based Bestcare, which is always an interesting experience (“from Korea, like K-Pop,” one of their folks explained with an attempt at humor last year). This is the best-looking product on the floor as far as I’m concerned, with a slick UI and innovative ideas like a graphical patient journey timeline. I would show you what I’m talking about, but like last year, they turned me down cold when I asked to snap a picture and their handouts don’t show screens. Anyway, they’re trying to get into 13 US hospitals, but I see challenges that go beyond language and culture – they don’t have a billing system, the terminology is not always US standard (like “ward” instead of “nursing unit”), and they brag that they will modify the source code to accommodate a customer’s needs, which creates an upgrade nightmare.
Harris Healthcare’s person who engaged me was friendly. I asked if Orlando Health was still using the former QuadraMed Affinity and she said yes – it will be 20 years upcoming. I didn’t mention that they’re planning to replace it (and Allscripts Sunrise and whatever they use for ambulatory) with what I assume will be Epic or Cerner.
Some company had a guy pouring chilled wine at 10 a.m.
I visited AssessURhealth, which offers a five-minute patient mental health screening questionnaire usually given in a physician office’s waiting room. Patients respond more honestly to questioned asked by an app rather than a person, and the physician practice is notified if their answers suggest immediate further questioning about any intentions to harm themselves or others. I asked the crass question of who pays for the service and it’s the doctor’s office, since they may generate more billables even while doing a good deed.
I strolled by the Aprima booth just as our sponsor sign fell over on the table, after which I noticed one of the company’s employees rushing over to reverentially place it back in place like the Mona Lisa had just crashed to the floor.
The best booth person I’ve seen was Hanna from Zayo. I care very little about bandwidth provider and to be honest I’ve never heard of the company, but Hanna’s sparkling repartee got my interest. She’s a pistol down there in Hall G.
I had to watch Bob Garner in action at the Cantata Health booth again. Within 60 seconds of my arrival, he had described in considerable detail how an attendee’s brother-in-law had passed away, even giving his full name. She basically froze, unable to comprehend what she had just experienced, and I saw her wiping tears. Bob immediately told another attendee how his brother had passed away and he also just stood there dumbfounded.
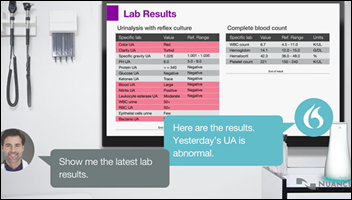
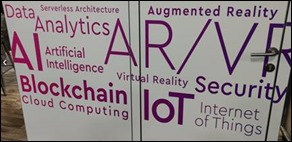
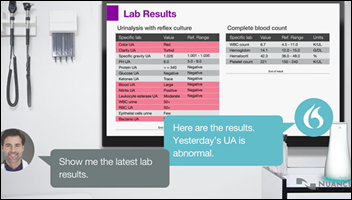
I signed up for an impressive AI presentation by Nuance CMIO Reid Conant, MD. He showed how a doctor in an exam room outfitted with a wall-mounted speaker-microphone can conduct a complete patient session using their voice alone just like when you talk to your Amazon Echo or Google Home device and it speaks back to you. The virtual assistant technology integrated with an EHR is fantastic – it can fill in discrete data fields and answer questions such as “has the patient had a flu shot?” The doctor can say, “Hey, Dragon, show me the two most recent chest X-rays,” then say, “Read me the radiologist’s impression” and then say, “Add to Susan’s task list to recheck the lungs.” The PCP can say, “Call the on-call hospitalist” and have it launch a VOIP call to create a handoff. Nuance developed the virtual assistant / virtual agent technology years ago for the auto industry. It was impressive and seems to be available now. It’s the best hope I’ve seen for letting the doctor focus on the patient, skip the effort and distraction of typing, and create a satisfying EHR interaction instead of clicking without gaining useful information (even scribes can’t give machine-generated suggestions). Epic is apparently demonstrating its Nuance integration this week and Meditech is on deck.
Tomorrow is my last day at the conference, so my last recap will be Thursday evening. Safe travels, especially those who left the Northeast in winter weather and now have to return in equally bad conditions. Feel free to send me any conference observations as we tie a bow around HIMSS18 and call it done.

























































































































































Move your quotes to where they should be and it's no longer politics-in-the-blog, but instead a fact that's true at…