Rhonda Collins, MSN, RN, DNP is chief nursing officer at Vocera of San Jose, CA. She is the founder of The American Nurse Project, which created a book, documentary film, and an interview series to elevate the voice of nurses by capturing their personal stories.

What was your role with The American Nurse Project?
I was the founder of the project. I worked for Fresenius-Kabi, which was the sole sponsor of it at the time. I wrote the foreword for the book. I hired Carolyn Johns to take the photographs and do the interviews.
I’m fully committed to nurses telling their stories. There’s a lot of power in allowing nurses to stand up and say, I am a nurse. This is why I’m a nurse. This is the kind of nursing that I do and the difference that it makes. The project was the opportunity for nurses to tell their stories.
How has the nursing profession changed in the past few years, especially with regard to education, gender, work setting, and leadership roles?
I think we’re headed into another significant nursing shortage. The overwhelming challenge to nursing is that we have many more applicants for nursing school than we have faculty. The issue is not that we’re short on schools or that we’re short on folks applying to be a nurse. It’s that we don’t have enough faculty, for various reasons. You have to have a certain degree of licensure to be an instructor. The pay may not be what it is in other areas of nursing.
But I would say that nursing continues to diversify. If you can imagine it, pretty much we have it in nursing. I’m an example of that. I started out as a labor and delivery nurse. I worked in hospitals for almost 10 years and went through the regular progression of management. I was vice-president of a major medical center in Dallas. I left and went into industry. I have built a career of nursing informatics and working in technology because healthcare is driven by technology like any other industry.
When you look at how we integrate all these medical devices, how we streamline communications and patient records and everything that we do, the nurse is still at the front line. Nurses have had to pay attention, to be involved in the decision-making about what goes between the patient and the information system.
Nursing is pivoted toward the technology side and pivoted toward nurses having to understand exactly what they need to do with all of this technology that we’re handed. Stuff that monitors their patients, stuff that they carry, all of those things. That is a significant change to the profession.
Nurse education requirements have increased from diploma RNs to associate’s degree to now bachelor’s and advanced degrees as hospitals reduced their use of licensed practical nurses. Has that helped create the RN shortage?
There’s two schools of thought on that. If you look on the professional side of nursing with our professional organizations, they will tell you that entry into practice should be a bachelor’s degree in nursing. I believe that the American Nurses Association and all of our other entities have taken that position and tried to provide opportunities for nurses to either be grandfathered in, especially advanced practice nurses, or to have the opportunity for the education.
The other side of that is that we are a rural country. Much of our country has vast open spaces with a limited access to healthcare. I live in Texas, which is one of those states. The notion and the support of the advanced practice nurse who does the primary care in clinics is heavily embraced in Texas. Advanced practice nurses have always had to have a master’s degree. Now we’re looking at what it would take to get advanced practice nurses to the doctorate in nursing practice.
A nurse never stops educating himself or herself. I’m an example of that — I just finished a doctorate. You just keep going because it’s advancing the profession.
It’s great that we’re creating these education and leadership opportunities, but I’ve read that the average age of a nurse is around 50 years. Will we have enough nurses working in direct patient care roles as Baby Boomers age?
The more critical issue about baby boomers aging is that they’re retiring, and they’re retiring out of the nursing profession. The bulk of nurses still practice in bedside care. There’s maybe 5 percent who have the doctorate and maybe 12-15 percent who have master’s degrees. Most nurses are either associate’s degree or bachelor’s degree and are involved in frontline patient care.
Some of the rural areas like Texas, New Mexico, and other places still use vocational nurses or licensed practical nurses. They have certainly not been phased out. Especially in areas where access to healthcare is scarce, where getting folks recruited to come out to these very rural locations, LPNs are used frequently.
Do frontline health system nurses enough influence over process, technology, and patient safety?
It’s an area that hospitals need to continue to work on. Most hospitals have a shared governance model, with decision-making from the bottom up. I do believe that those hospitals are focused on what the bedside nurses want and what is important to them.
I would also caution that with a looming nursing shortage, I’m already seeing hospitals offering big sign-on bonuses and moving relocation and all of that. We’ve already proven that that is not the answer to the nursing shortage. That’s not a way to retain nurses. Modern Healthcare just had an article about that, maybe two months ago, saying we’re doing something that we’ve done in the past that we know doesn’t really work. What we have discovered and what we understand is that people stay put. They stay in jobs where they feel valued and where they feel like their opinion matters.
Nurses are leaders. It doesn’t really matter if you have the title “leader” — you’re a leader at the bedside. You’re making independent decisions about how to care for that patient and that family. So whenever a nurse says to me, “I’m just a nurse at the bedside. I don’t really have any power,” I always remind them, you have all the power in the world. You have power to make this patient have a good experience. You have the power to ensure that this patient follows their care plan. You have the power to include the family.
This is what healthcare is about. For those of us who have been leaders in nursing for a long time, it is in everyone’s best interest for the profession and for those who work at the bedside to step back, look at it, and encourage those nurses at the bedside to step forward to offer their opinion. Then we act on that. We give them the tools that they need.
There was some research done asking nurses if they like 12-hour shifts or not. Of course it came back that nurses prefer 12-hour shifts. For the last 20 years, we’ve been trying to get nurses to agree that 12-hour shifts are too long. Nurses have been telling us, we don’t mind the 12-hour shift. It’s not the number of hours we work, it’s what happens in that amount of time. If we have the right tools, if we’re staffed properly, if we have the right policies and procedures, and we feel like our work is heard and valued, eight hours or 12 hours is not the issue. Those are the things that those of us who are leaders in healthcare need to take some time to listen to and understand.
Hospitals struggle with nurse burnout and disrespect or outright harassment. Do those affecting the typical nurse’s workday?
Absolutely, and have for decades. That is a cultural issue that each individual hospital has to address. I have colleagues that I’ve worked with that created websites to address the issues of nurse bullying. Nurses and physicians deal with violence from patients. They deal with violence from patient families and issues. Then it’s the internal bullying, nurse to nurse or physician to nurse. That is a cultural issue that has to be addressed head on and aggressively.
How much does the bedside nurse influence hospital patient satisfaction?
Probably 80 percent of a patient’s satisfaction is the experience they have with the nurse coordinating their care. Although the patient doesn’t always understand that it’s the nurse coordinating their care, the nurse gets the order for physical therapy. The nurse puts in the order and is managing five or six patients. If physical therapy is late arriving, the patient’s perception is that the nurse is late. There is a tremendous amount of coordination, communication, and decision-making by the primary care nurse to determine, when do I need to manage this patient’s pain medication so when PT gets here this patient will be comfortable enough to do their range of motion exercises? Then following that, will they be ready to eat? All of this has to be planned out, and it’s not just for one patient, it could be for four to six patients every day.
Think about what it takes to order your day. If you’re like me, you live by your Outlook calendar. If it’s not on my Outlook, it doesn’t exist. These nurses have to come in every day and go through these orders. Physicians make changes to the orders and nurses have to be able to reorder that into the patient’s care plan. I truly don’t think families, patients, or anyone — sometimes even other entities in the hospital — understand how much flows through the nurse’s hands to ensure that these patients have a satisfactory experience and leave the hospital with a better prognosis than they had coming in.
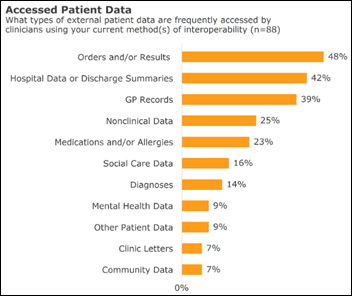
A Black Book survey suggests that nurses are getting more comfortable with technology and are feeling that their IT departments listen when they ask for system changes to improve productivity or patient safety. How has technology has affected nursing workload and job satisfaction? Do nurses have enough voice in how the technology is chosen or used?
It is a work in progress. When the clinical end user — the nurse, the physician — is involved in the decision-making with IT, the rollout goes better. The adoption goes better. You achieve the results that you want to achieve. CIOs are understanding more and more that even though a solution may fit into a hospital in a technological way — it sits on the platform or it works within their framework or integration — if it doesn’t work at the bedside, then the chances of those folks using it are pretty slim. I am seeing more and more that nurses and physicians are being involved in the conversations about what technology is used.
The role of the chief nursing information officer is rising. This role is different from the CIO or the CMIO in that their role is specifically to look at technology and how it works from the IT side of the house to the bedside, the patient. CNIOs work out from the bedside to the technology. That is a huge improvement and will make a difference in those hospitals who employ CNIOs and ensure that whatever the decision made by the hospital works for the nurse at the bedside.
This challenges patient’s perceptions of technology. It is generational. Nurse adoption of some types of technology, such as mobile technology, is generational as well. It’s what you’re used to. Sometimes we have to advise patients in the mobility world that if you see a nurse on a smart phone, they’re not on social media — they’re actually taking care of you. They’re not ignoring you. This is all to ensure that your experience with us is a positive experience.
That is changing the relationship between the patient and the nurse, or the physician, as well. We’re taking what we use in our everyday lives, what is ubiquitous to our everyday lives and makes our lives much, much easier, and now it’s coming into the healthcare environment. It’s a cultural shift, because folks on the outside would be perfectly accepting, but inside the hospital they’re like, why are they on their phone? We have to ensure that we verbalize that to the patient and family to understand that this is part of the technology growth for the health system as well.
Nurses can pursue informatics education, certification, and a specialized career track. How is that affecting the use of technology in health systems?
The formal education for informatics nurses is outstanding. I think that that’s really where we need to go. In fact, I was just in Orlando, Florida at the American Nursing Informatics Association annual conference. All of the nurses attending are involved in hospital IT in some way to ensure that technology gets to the bedside intact in a way that services the patients and the overall good.
I think we have a long way to go. Nurses for a long time have surrendered their power to IT because they weren’t comfortable with the language. They don’t really speak the language. Sometimes they feel so ill-informed they don’t even know the right questions to ask. Those of us in this world of informatics nursing have a responsibility to tell two friends, and they tell two friends, and we continue the education to insist that nurse leaders are at the table and learn to speak the language.
Decisions are being made about technology that are going to last for decades. If we don’t have the nurse’s perspective or the patient perspective in that conversation, we will deeply regret it.






















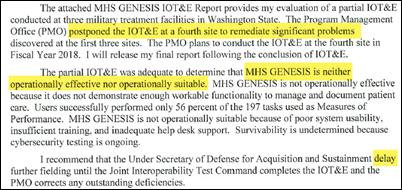
















I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…