Ron Remy is CEO of Mobile Heartbeat of Waltham, MA.

Tell me about yourself and the company.
Mobile Heartbeat has been in existence since 2009. The current product was introduced in 2011. It’s my second project working together with the technology team that started the company. I’ve been in technology my whole career. I was an early employee of Sun Microsystems, going all the way back to 1985, so I’ve been in the technology industry for a long time.
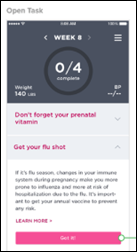
Mobile Heartbeat makes a product line called MH-CURE, which is a clinical communications and collaboration product. It’s designed for acute care and affiliated ambulatory facilities of hospitals. It runs on IOS and Android smartphones and is available both on-premise, with servers inside the hospital’s data room, or a cloud offering via our cloud partner, Parallon Technology Solutions.
What do clinicians want from mobile apps other than message exchange?
The most important aspect is to know who’s on the care team for each and every patient, as well as the status of those individuals. Particularly in the larger facilities, you may not personally know every member of the team that you’re on. You need to be able to instantly recognize who is the nurse, who is the physical therapist, who is the cardiologist taking care of that patient, You need to know exactly what their status is — online or offline, in the facility or out of the facility — and then be able to communicate to them with a variety of methods — secure text, a phone call, a video chat, or even a page.
All of those are the communications capabilities, but if you don’t know who to contact, whether they’re available, why they are relevant to you, and what their context is, the communication systems aren’t all that impactful.
What kind of outcomes to customers see?
We talk about a value hierarchy. You get started with implementing mobility in smartphones and their applicable software — which includes our class of software, Mobile Heartbeat, as well as your mobile device management software — and your infrastructure to support those. Your wireless network, your servers, your security. Then layer on top of that our software and the smartphones.
The first thing that you need to look at to make sure you’re getting to the Holy Grail, which is better patient outcomes, is the adoption ratio. How many users are on this mobile network that you’re providing? We tend to quote Metcalfe’s law. It’s an interesting telecommunications law that the value of a network is equal to the square of the number of nodes on a network. For a 10-node or a 10-user network, that value is 100. For a 1,000-user network, that value is a million. It’s much more valuable. If you don’t get high adoption rates, if you don’t get a lot of users on your network, the value is relatively low.
Now that you’ve got your adoption rate high, you start looking at how people are communicating with one another. Who is texting who? Who is calling who? How often? You start to analyze those patterns. Why are people communicating with one another? If you know why and when, then you can start optimizing the workflows around that. Take Lean thinking and apply it to your workflow.
One of the greatest learning experiences early on at Mobile Heartbeat is that the number of ancillary staff members — not necessarily just the nurses and doctors — that you’re in communication with on a regular basis is extremely high. If you exclude those people from your mobile network, your mobile program, you’re missing out on some great workflow improvements.
Once you improve your workflows, the best possible thing that you can achieve is higher quality and better patient outcomes. Very few customers are at that point. They’ve not deployed mobility for that long a period of time. But everyone needs to get there. That’s the top of the pyramid — higher quality, better patient outcomes.
How do you go about analyzing that and what kind of insights can you gain from looking at how they’re using the system?
We have a team of three informaticists, nurses with an informatics background, that assists clients in this analysis. A system like ours creates a huge amount of operational data. The first thing to do is to extract that, do some data mining on it, and see what the communication patterns are. Who is calling whom, who is texting whom and when?
The patterns might tell you that there’s a huge amount of texting going on between the nurses and the warehouse, surprisingly. Why is that? Maybe it’s because they are constantly having to track down supplies. They’re always in contact with the warehouse trying to locate something that they need desperately for a patient. Now that you know who’s texting whom, you can look at the rationale behind that and start to optimize that.
The next level of optimization, and we’re just beginning to do that, is to look at using natural language processing to not just look at who’s texting whom, but also look at the actual content of those text messages. You can get some real insight on that.
Let’s go back to that same analogy of the nurse constantly contacting the warehouse for a specific item. Using natural language processing, you know that they’ve been requesting a specific item all the time. If you know it’s a major workflow request, let’s make that item a little bit more available. Maybe stage that item in the nurse’s central station. Now you’re starting to take this communications system and apply it to workflows, to make those workflows more efficient and to raise the quality and the speed of what you’re getting done inside the hospital.
What kind of integration with other systems is offered or beneficial?
Huge. That’s probably the biggest requirement. The most obvious one to get started is to the electronic medical record, specifically the ADT feed coming out of the EMR, to know which patients are in and out of the hospital. That’s a requirement for having a care team directory and a patient list available to your clinicians.
The second is into the nurse call system of the hospital so that nurse call alerts and alarms aren’t randomly sent to the unit, but instead are directed to the correct responder’s smartphone. That’s a requirement of any system like ours.
Integration to the lab information system makes critical lab results available to the clinician. They’re looking at a patient and they want to see exactly what’s going on with their lab results.
Integration to third-party messaging systems. That’s a generic term, but I’ll give you an example of what one of those is. There’s a tremendous amount of effort in predictive analytics around sepsis prevention using patient data and maybe even population health data to predict that a specific patient is going to go into sepsis. The system that does the analytics makes the determination that a specific patient might be a sepsis risk. Now you have to tell somebody to take action. The integration to that third-party system has to come from that system into Mobile Heartbeat and get sent to the correct clinician taking care of that patient. We’re the last-mile delivery for all these third-party messaging systems. That’s an absolutely critical integration that you have to put in place.
To foster that, we’ve built a fairly comprehensive API set. One of those APIs handles incoming messages from third-party systems and directs them to the correct caregiver. That message can have multiple choice responses, so the caregiver, the nurse, the physician gets the message, it pops up on their smartphone, and they can indicate their response and have that go back to the initiating system to take further action. Maybe it kicks off another alert or alarm or another message. All of that integration is a requirement.
Clinicians use to have a belt full of gadgets because each application had its own device. How do you figure out how those applications can coexist on the device that a user is assigned or brings in from home?
Let’s start physical and then go to logical. When we started the company, we realized that the utility belt effect was powerful and we needed to address it. You’d look at a clinician and they might have a pager and two voice-over-IP phones on their belt walking around the facility. The first step was to consolidate all that onto one device. The advent of the smartphone and its capabilities made that, obviously, the perfect device. That’s where most industries that were consolidating any type of telecommunications or communication systems were looking.
We built our software to take advantage of a couple of key features. The first is to use voice-over-IP for inside the facility, so that you’ve got a voice-over-IP phone that is available for making phone calls over the WiFi network.
The second was to take a look at those old-school pagers that everyone wanted to get rid of. They were all wearing them on their belt. They wanted to get rid of the pager, but they couldn’t get rid of the actual paging service, because the workflows that they’ve been using for 15 years required that paging capability. We developed the ability for sending and receiving pages to come directly into our application using the existing pager service.
That was the first level of making this a much more efficient product and getting rid of some of those utility belt things that you’ve seen in years past. We think that trend is going to continue. It’s pretty obvious that people want to use their smartphone.
The second part of that is, early on, we asked clinicians what they wanted to do on the smartphone. The answer really shocked us. It was, I want to do everything on it. I never want to get in front of a workstation again if I don’t have to. Because when I’m in front of a workstation, I’m not with a patient. With my mobile device, I can be with a patient, so I want everything on that.
That led us to enable another API set that we call the InterApp launcher. You can leave Mobile Heartbeat and go directly to another application. No extra login, so you log in once to the system using your Active Directory login. You log in to every application as you move to it and you can pass patient context. For instance, I can leave Mobile Heartbeat, look up the exact same patient in AirStrip, and view the live waveform of that patient seamlessly, just by clicking inside of Mobile Heartbeat. I don’t have to do any manipulation of the new application. That is the next level of integration we see.
Where do you see clinical communication going in the next five years and how will the company be involved?
Apple announced in their recent earnings call that our largest customer just purchased 100,000 IPhones to launch a corporate-wide mobility program throughout all their hospitals. We’re the core software of that mobility program. That is an absolute milestone in the industry, seeing major players announce that they’re going into mobility in a big way. Software to run on those devices, Mobile Heartbeat and others, is a key component to the rationale behind this.
A year ago, we installed our product at Sunrise Medical Center in Las Vegas, Nevada. It’s a good-sized facility one block off the Las Vegas Strip. When the Route 91 Harvest Festival shooting happened in October, 214 of the injured patients made their way the ED of this specific facility via Uber, police car, or with a bystander. We didn’t really know much about it at the time since it happened in the middle of the night here in Boston.
We were a core component of that facility’s ability to triage, treat, and successfully take care of those patients. To get the staff at the right place at the right time. To broadcast out to everybody, both inside and outside the hospital, what needed to get done.
The learning from that is going to be industry-wide. If you do not have a communications platform in place — both physically with phones as well as your network and the software you’re using — then you’re really not prepared for that kind of event. I don’t want to cast doom and gloom, but being prepared for these types of mass casualties in any good-sized facility is something that requires a lot of care and preparation. We believe that the technology that we build is one of the components of being prepared for that.
Our software and our own products are very exciting, but the industry as a whole is just as exciting. We love to see potential clients picking up mobility in any form. We’d obviously love our product to win every single time, but we’re more excited when they make a determination that smartphone technology is the way to go inside their hospitals. It’s a big step forward in healthcare in the United States.
Comments Off on HIStalk Interviews Ron Remy, CEO, Mobile Heartbeat























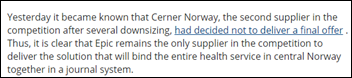















































That, or we see if Judy will announce Epic's new Aviation module (probably called Kitty Hawk) that has integrated Cruise…