Curbside Consult with Dr. Jayne 7/23/18
Every time CMS releases new proposed rules, I feel like the circus has come to town. The most recent offering includes 1,472 pages of bliss and is open for public comment until September 10.
I used to try to read them on my own, but found it too hard to get through them in a timely manner. I’m grateful to the people who have dedicated time to review and summarize them for the rest of us. It seems like most healthcare media outlets are trumpeting the “historic shift” for ambulatory Evaluation & Management (E&M) codes, so I decided to do a little deeper dive myself. Most recent federal proposals trumpet their aim to reduce administrative burdens, so I was curious whether they had truly found the “easy” button.
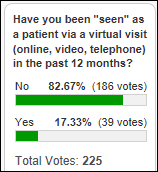
This document is a double whammy, addressing both the Medicare Physician Fee Schedule and the MACRA Quality Payment Program. There’s a whopping 0.13 percent increase in the fee schedule, which frankly I would rather have had them just keep it static than to try to explain various updates and adjustments. There are new G codes for preventive telehealth services that may be enticing for primary care physicians.
Our enthusiasm is curbed, though, by the continued insistence on EHR support for Appropriate Use Criteria for Advanced Diagnostic Imaging. That’s a measure that has been created, delayed, stayed, and revisited for the last several years and now will start in January 2020, with a year-long testing period but no enforcement. Providers can apply for hardship exceptions if they have poor Internet access, EHR vendor issues, or uncontrollable circumstances. CMS is relaxing a bit in allowing AUC tasks to be performed by ancillary personnel rather than requiring the provider to do the work, so that’s a good thing. It will be interesting to see how much of a difference the use of AUC really makes. In my market, we’re already well trained by commercial payers so that we don’t order tests that aren’t indicated.
The Accountable Care Organization programs received an update, with some measures being retired and a new one added. I didn’t spend too much time on the ACO part of the rule, since it’s expected that CMS will release a separate ACO regulation in the near future. I jumped to the part about outpatient E&M coding, which wasn’t as exciting as I expected. Providers will have the choice to document and code their visits based on the current schemes (formulated in 1995 and 1997) or through either a framework around time and medical necessity, or one around medical decision making. Rather than the distinct charges we have now for visits under the 99202-99205 and 99212-99215 codes, a blended rate is proposed.
Not surprisingly, there is a shift towards the lower end of the range rather than a shift towards the higher end, and for those of us used to performing and documenting high-level visits, it will be a cut. This may be made up for by the reduced documentation requirements, but for providers used to maximizing their use of macros, personal defaults, and templates, the perceived reduction in work isn’t going to make up for a more than 10 percent reduction in payments. If you’re not optimized on your EHR or don’t document efficiently, it may be a boon, but not for every practice.
As far as MACRA, MIPS, and the Quality Payment Program, CMS is just shuffling things around again. Advancing Care Information has been renamed Promoting Interoperability, and additional providers are being invited to the party: physical therapists, occupational therapists, clinical social workers, and clinical psychologists. From a quality perspective, all-cause readmission is being added as a measure for groups. Quality reporting will remain full-year, despite provider groups lobbying for a change.
Quality measures that CMS has identified as ineffective will be dropped, potentially saving physicians $2.3 million. Additional quality measures will be added, including four that address patient-reported outcomes. Reporting for Improvement Activities will be 90 days, however, along with Promoting Interoperability. Use of Certified EHR Technology that complies with the 2015 edition is mandatory. Within the Promoting Interoperability category, new elements are available for Prescription Drug Monitoring Program (PDMP) query, verification of an opioid treatment agreement, and expansion of electronic referral loops by receiving and incorporating information. Vendors will need to incorporate functionality to track and report on these elements, and I suspect that many do not currently have that capability.
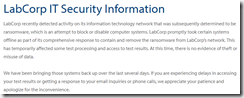
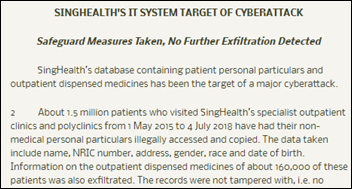
Security Risk Analysis remains a required element. I continue to find practices that think that this is somehow the responsibility of their EHR vendor and who don’t understand that it’s the covered entity’s responsibility, with EHR vendor compliance being only one piece of it. Organizations are required to assess how they handle Protected Health Information in a variety of different settings, whether in person, on paper, on the phone, etc. which may or may not have anything to do with the EHR. If you don’t know your organization’s plan for Security Risk Analysis, it might be worth a discussion.
As was true previously, participation in an Advanced Alternate Payment Model such as an Accountable Care Organization means a practice doesn’t have to keep track of all the changes in the Merit-based Incentive Payment System (MIPS) model. The APM track is definitely where CMS wants providers to be, adding a 5 percent bonus for them. CMS is also pushing providers to be ready for programmatic updates on a regular timetable with its move to combine QPP with the Physician Fee Schedule. If this holds, providers can plan for updates to both in July and November instead of playing the waiting game.
Still, each time a new rule or proposed rule comes out, the chatter in the physician lounge increases. In my market, we’ve seen a number of established clinicians opt out of Medicare and even more choose to move to cash-based practices whether they involve retainer / concierge fees or not.
My practice remains firmly opted out of MIPS although we accept Medicare patients without restrictions. It remains to be seen whether there will come a time that the penalties outweigh the extra work that will be required to avoid them. So far, we’re diversified enough that it’s not an issue. As I work with practices that don’t have the luxury of non-participation, I’m thankful for that day a couple of years ago when we disabled the “Meaningful Use Content” checkbox and our lives got quite a bit easier.
Given the published comment period on this proposed rule and the typical CMS schedule, we’ll know in a couple of months whether any parts and pieces will be thrown out or modified. Based on this proposal compared to all the feedback that has been submitted on other proposed rules, I’d bet there aren’t too many material changes.
What is your take on the proposed rule for MPFS and QPP? Leave a comment or email me.

Email Dr. Jayne.

































![image[30] image[30]](https://histalk2.com/wp-content/uploads/2018/07/image30.png)





In fairness to the person on the thread the other day: Now THIS is politics on the blog. :)