Mike Linnert is founder and CEO of SymphonyRM of Palo Alto, CA.

Tell me about yourself and the company.
The team and I have been doing customer relationship management solutions for large consumer service brands for 15 to 20 years. We’ve had the privilege to work with some of the biggest brands in the country, such as American Express, AT&T, Wells Fargo, and Verizon. We’re taking the learnings from those industries — how they take data, how they distill data down to action, how they use it to proactively engage their customers — and bringing that insight into healthcare. There’s a real opportunity for it.
How does healthcare compare to other industries in its use of customer relationship management systems?
We’re 10 to 15 years behind. You can see it in a few key ways. Healthcare is just starting to think about how to proactively reach out to our customers. Traditionally, the business model was that we waited for them to need us and call us, then we focused on providing good access. The paradigm is shifting. It’s both a competitive imperative and a business imperative, but it’s also a health imperative to drive healthier, happier customers. Health systems are beginning to aggressively reach out.
You see pockets of it starting to happen, in particular, with organizations that are looking at population health and starting to take some risk. They’re moving from “we have a lot of data” to “we have lists that we need to call or execute against.” We’re seeing it more aggressively by organizations that have taken more risk, or those that have the luxury of being able to be forward thinking. But they’re in the early stages. They haven’t thought about how to use technology to drive it, haven’t identified the business metrics that indicate that they’re doing well, and haven’t institutionalized the process.
Health systems historically didn’t want to make it obvious in a customer-facing way they were running a business. Is it a change for them to be behave like a for-profit business in going after new patients, upselling services, and measuring doctor loyalty?
I would say it’s less about thinking about being a profitable business and more about improving delivery to customers. Other customer service industries have found a way to take the business they have, distill it down to a few key metrics, and then take action based on those metrics. Can we distill all our data down to value, delight, loyalty, and next best action for every single customer we have?
The most important of those is the next best action. A health system should be able to answer the question of, if I had the privilege of talking today to any one of the million people that I have in my patient / customer database, what would be the most important thing I could say to them? That involves looking across the health system. We execute in different silos — the population health team, the primary care team, case managers, care coordinators, revenue cycle, and on and on. I need to grab all the data from all those different groups and distill it down to action. What do we want to do?
Then I need to the able to prioritize those actions by combining what it takes to keep my patients healthy and loyal, the capacity I have available to serve them, and the metrics that drive my business. The metrics I use to drive my business don’t have to involve profitability. Some look at growth. Some look at profitability, because no money, no mission, and I need to run the health system. But if my goal is delight, I’m measuring how happy my customers are with me. That’s an important metric and it impacts my next best actions as I allocate them.
People miss the concept of stirring capacity and business metrics into patient need. When I’m looking for the right patients to reach out to proactively, I don’t want to call a patient and extol the virtues of an annual wellness visit if their doctor doesn’t have any capacity to do annual wellness visits for the next three months. If I’m going be proactively reaching out, I need to prioritize who I can serve the best right now. That’s a fundamentally different way of metric-driven thinking.
How much overlap exists between pure analytics systems versus your system of using analytics to drive consumer engagement?
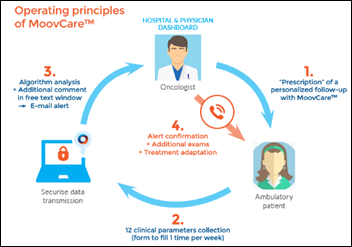
We think of ourselves as an algorithm-driven CRM company. It has two parts. Part one is getting all the data that we can, factoring in the corporate priorities or imperatives and the available capacity. Running algorithms that map the combination of those three variables into next best actions for everybody. That’s part one, the analytics.
Part two is how to engage customers around those next best actions. Engaging them is where a traditional CRM takes over, but they’re not well married to that next best action data analytics piece within healthcare. Once we inject those next best actions, we can start looking across the different silos of the business and saying, for this list of patients, the population health team is the most important next best action. The population health team might determine that their metrics are driven by the imperative around driving down per-member, per-month costs, which is really a proxy for making sure we’re seeing the right numbers at the right venues and the right times.
I’ll give you a tangible example. Some of our clients are coming to the conclusion that the next best actions that can help them bend the cost curve and drive patient delight are weekly or monthly phone calls. Maybe we take our high-cost, high-need patients and put them on a schedule. We’re not calling to say “you have a care gap” or “we have some coding gaps we’d like to get closed with you.” We’re calling to say, “Hey, how are you doing? We noticed that you’re consuming a lot of care. How can we help you better map into the services we have that are maybe more appropriate for you, making sure we’re seeing you in the right venue?”
We find that those weekly and monthly calls aren’t necessarily just health focused around how the patient is feeling, their pain, or their medications. They evolve to be things like, “How did you do last week? You were going to do a 5K, how did it go? How’s your family doing?” It’s in the context of those weekly calls that we discover the things that we can be doing to help. Referrals to job placement, referrals to food banks, getting a patient to see a primary care doc for an emergent issue before it turns into an ER visit.
This sounds like new ground for hospitals in having non-billable patient conversations. Do you coach them on what they should be doing?
We work together with our clients. Our business model is fewer, bigger clients. We talk to every one of our clients every day. As we learn things with different clients and we see things work, we’re constantly sharing.
But the driving force usually has to start within the medical group or the executive team. There has to be a metric or an imperative that gets reduced down to next best actions. Calling people with a potentially high need is not enough. You need a true metric that says, the way we’re going to measure success around this effort — and I’m grabbing a random one — is that we’re going measure per-member, per-month cost and customer delight. If we do that, then we can show that based on those metrics, we can identify the actions that drive those metrics. We can reduce our next best actions to a dashboard that we can manage against. It’s not spinning up an effort, but rather trying to drive a metric, and in service of that, here are the things that we’re going do.
Frankly, things go pretty fast. If you don’t see the metric moving the way you want within a month or two, then something’s wrong. If we’re doing a good job of tracking both activity and accomplishment, we can say that the metric is not moving because we didn’t get in touch with the patients we said we wanted to. Or, we got in touch with them, but our schedules are such we weren’t able to get them in for the appointments we wanted them to have. Or, we got them scheduled, but some of them no-showed the appointment.
If you’re tracking that, you can decide what to do differently. You should be able to be reduce whatever issue you’re tackling to next best action and what to do differently for each customer.
Are those health system and medical practice efforts segregated by whether a given patient is covered by a risk agreement versus being billed under fee-for service?
Some of those things get considered some of the time. We’re looking for the opportunities to create value for our customers. What do they need from us? You make a really good point that when people come to us, it’s easy. We just do the things that they ask for or the things that we believe they need. When we switch that and say we’re going to go to them and we’re in the proactive outreach business, we have a problem. If we have a million people in our customer database, we couldn’t call all of them today even if we wanted to. If somehow we could call all of them today, we don’t have appointments or services available for all of them today. Now we’re in the business of trying to figure out the most important people to call.
You’re correct that part of the decision involves corporate priorities. If we have a priority around our ACO and one of our priorities for our ACO patients is driving down per-member, per-month cost, then we look at those people who might have the the biggest impact and what things we can do for them, then call them first. Those things can range from consuming care in the right place to leveraging social determinants of health. If we know financial security is a challenge for you right now and that drives your health, then let’s make sure that we’re talking to you about referral to job training or job placement and engage around some of those things through the proper channels.
What best practices have you seen for health systems improving their relationships with physicians?
You have to be really clear if you’re going to have physician outreach. What’s the purpose? What is the definition of success? We see a lot of physician outreach teams meeting with providers and talking about referral patterns, but it’s not clear how you measure them. An executive team could say to the provider outreach team, we want you to make sure our providers are reducing leakage. That’s probably the most common one we see.
But some of our more sophisticated customers are also saying, we want to educate our providers about what’s going on in the system and where we think we’re moving forward. Or, we want to educate our providers about our solutions to help them drive their quality metrics. Or, we want them to understand that we have marketing programs they can take advantage of. That’s one aspect.
The other aspect is that if we do next best actions the right way, we’re having a pretty big impact on provider satisfaction. Systems that have moved into population health are using their population health system to surface lists for the primary care office, such as those people who need retinal exams or breast cancer screening. The lists help offices hit their quality scores, but they create another administrative burden for the office. Now the office has to figure out which lists move which metrics, which metric they are furthest behind on, and how they can find time to do outbound calling. That’s a challenge for them.
The right way to do that — and the way any other industry would do it — is to say, let’s look at those lists as yet another feed into our candidates for next best actions. Then go to the office and say, we have one list. We’ve run the algorithms for you. We’ve prioritized the most important people for you to reach out to.
If we’ve done that right, we can even offer to take that outreach effort out of the office. And if I’m really looking forward, instead of having you remain accountable for your quality scores, let us the central health system be accountable for reaching out, driving the right patients to you, getting them on your schedule and into your office, and letting you know the most important things to do with them while they’re there. That puts you in the business of engaging the patients, doing the things you see as most important. Just make sure to check our list of why this particular patient is in your office or why we reached out to them to come see you.
Do you have any final thoughts?
Healthcare is evolving really fast. If you look forward five or 10 years, most health systems are under-serving their customers today. They are under-investing in their customers and in proactive outreach. If they can generate these lists of next best actions, use the data and lists they have, inject their business imperatives and capacity availability, and map next best actions for every single patient, then they can engage in proactive outreach in a way that drives patient health, drives patient delight, and hopefully reduces provider burnout. It also drives financial performance.
That really is a big change because it requires rethinking about metrics and where they are going. We’ve taken in over five billion lines of data in pursuit of coming up with these next best action plans for every single patient in our universe.
The imperative we see is that if you don’t do it, somebody else will. There are a lot of people coming into healthcare today who are trying to compete with health systems. Their number one observation is that most patients are not tightly tied to those systems, so they have an opportunity to insert themselves between the health system and the patient and grab that customer relationship. If health systems can start mapping the next best actions and engage in proactive outreach, they can drive the relationship they want to have.
I would love people to think about us as the next best action guys. Being able to reduce all the data to actions, not just presenting more data, is the critical thing that will happen in healthcare. It has proven successful in every other consumer service industry.
Comments Off on HIStalk Interviews Mike Linnert, CEO, SymphonyRM





































































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…