Curbside Consult with Dr. Jayne 11/12/18

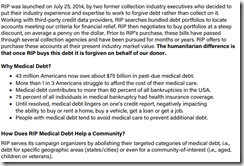
I was intrigued by the results of Mr. H’s recent poll results regarding reader attendance plans for HIMSS19. Only 28 percent of respondents will be going, although the sample size is pretty small at 216 readers. Most of the people I’ve asked recently about their HIMSS plans are under substantial budget constraints, with some employers limiting even high-level IT staffers to only one conference per year. Those with limits seem to generally choose their EHR vendor’s user group meeting, or otherwise a meeting that is more specific to projects that they’re going to be working on in coming months.
Since HIMSS released the educational sessions schedule this week, I decided to do a bit of a deep dive to see what is on the calendar that might be interesting to potential attendees or might bring value to their efforts to persuade their employer to send them.
The first place I landed was the subset of Views From the Top sessions, where attendees can “be inspired by compelling stories from high-ranking leaders in a variety of industries.” The first session that popped up was one presented by Jason Cheah, who is CEO of the Agency of Integrated Care in Singapore. I do enjoy the international sessions, often there are some progressive approaches to healthcare IT problems, although it can be tricky to find nuggets that can be applied back home since the healthcare delivery systems might be significantly different from what we have to work with in the US. I recently spent some time with some physicians from Canada and learned that although some of the issues are the same, there’s enough of a different spin on payment and prioritization of initiatives that some of the best ideas I heard would be difficult to apply at my own hospital.
Wednesday’s session titled “Transparency in Prescription Drug Costs to Help Patients Save Money” will certainly address a US-centric topic, given that the presenters are CVS Health Chief Medical Officer Troy Brennan, MD and Surescripts Chief Executive Officer Tom Skelton. They’re slated to talk about drug cost and benefit plan information transparency and how to better expose that information to patients, prescribers, and pharmacies. Price shopping is a big deal for the patients I currently serve – many are using sites like GoodRx to help make medications more affordable. It’s still a patchwork of coverage, though, as one of my patients found out when a local Walmart refused to honor the $15 price listed in the app, telling the patient it would be $50. The patient didn’t fill it at our office due to a $40 price tag in the first place, and with the drive and the confusion ended up in a situation where our office was closed so they couldn’t get it from us for less, so they didn’t fill it at all. Not good news for the teenager with bronchitis and asthma who really would have benefitted from access to an inhaler overnight.
Another Views From the Top session is titled “Defeat Nation State Actors Stalking the Health Care Sector” and covers cybersecurity best practices and risk exposure management. It sounds interesting, but likely more suited to the technical side of the house as opposed to the average clinical informaticist.
Next, I went to the section titled Reactions from the Field, which is designed to feature “market suppliers ‘in the field’ working closely with healthcare organizations to address common issues in cybersecurity, innovation, life science / pharma, or artificial intelligence.” It goes on to note that there will be four sessions with three panelists each, but no details are published. I’ll have to check back in a month or two to see what that’s all about. The Industry Solutions Sessions are also not listed in detail yet but are slated to include vendor-sponsored case studies presented in hour-long sessions.
The HIMSS Davies Award Sessions are listed and include a number of bread-and-butter type sessions covering issues we deal with on a regular basis: improvement of quality scores; reducing urinary tract infections due to catheter use; decreasing falls; improving pediatric asthma outcomes; sepsis management through clinical decision support and virtual care; clinical risk systems; and achieving the Triple Aim. Although some of the session descriptions clearly stated which organization was presenting, others used acronyms or abbreviations that left me guessing. There also were no presenter names included.
The Government Sessions header also failed to include a list of actual sessions, although it promises to help attendees “get answers to your pressing questions surrounding the Trump Administration and its impact on health and health information technology.” I assume the usual players will be making an appearance, but again will have to check back.
From there it was on to the General Education sessions, where a brand-new Blockchain Forum has been added. There are three specific sessions listed out for those of you looking to get the most current information on everyone’s favorite buzzword. I found a couple of interesting sessions interspersed among various forums, including one on counterfeit pharmaceuticals in the supply chain and another on data interoperability across non-hospital care venues such as long-term / post-acute care facilities.
There do appear to be a couple of new formats and venues for sessions. The SPARK Session (Session Providing Actionable and Rapid Knowledge) is designed to be 20 minutes of quick insights. Sessions are also being grouped into “content streams” aligned with the Quadruple Aim and allowing attendees to focus on domains of technology, information, organizational efficiency, care, environment, and societal challenges. There will also be a Learning Lounge with on-demand viewing of live-streamed sessions. I hope the room is large and the chairs plentiful because it might become the hip place to be for those with tired feet and aching backs.
From a consultant standpoint, I’m hoping there will be some good sessions in the Federal Health Community Forum, although no sessions were listed yet. I’m helping clients through a number of governmental initiatives including the Comprehensive Primary Care Plus (CPC+) program and of course MIPS, so if there’s any easier ways to navigate or advise, I’m hoping to pick up some tips. As with other areas, the details aren’t quite posted yet.
In the email announcing the session listings, HIMSS promised over 400 sessions and there certainly isn’t anywhere near that number posted yet for our consideration. It just goes to show that I should probably go back to planning my HIMSS session attendance like I have for the last several years – at the last minute on the plane while sipping a cocktail and hoping I packed the right shoes. At least by then HIMSS should have all the sessions listed and maybe some presenters.
What’s your strategy for planning your trip to HIMSS? Are the sessions important, or is it more about the exhibit hall, building new relationships, and catching up with colleagues? Leave a comment or email me.

Email Dr. Jayne.
















































I generally follow AP Stylebook style guidelines: Do not use all-capital-letter names unless the letters are individually pronounced: BMW. Others…