
News Items
CMS Administrator Seema Verma said in today’s opening session that previously announced hospital penalties and lower incentives for practices were supposed to encourage the industry to move forward on its own with interoperability, but the industry’s failure to do so resulted in this week’s proposed rules that are more prescriptive. She said the changes are aimed at insurers that refuse to share their claims data, although I’m not sure that comment was intended to be comprehensive.
Former White House CTO Aneesh Chopra agreed that the industry failed to self-organize to add more content, adding that the federal government’s initial data set was supposed to be a minimum, but the private sector didn’t take it further and the government had to create a new rule to get the entire medical record. Chopra said that CEHRT 2015 is a Roku and now we can add channels.
Verma added that this administration wants to deregulate, but the industry’s lagging behind the government required new regulations to get value for the $36 billion it spent on Meaningful Use. She also said that the next task is to bring in post-acute care providers.
University of Toledo issues an RFP for an EHR, apparently giving up its questionable project to help then-Athenahealth (now Virence Health) develop a new inpatient system. I expected that project to flounder once Elliott Management started pressuring the company, but there’s not much doubt that it will never see the light of day under new leadership.
From the Burner Phone

“Hope you’re enjoying Orlando, and washing your hands regularly. This little tidbit just crossed my Twitter stream. I look forward to seeing it mentioned in the News section.” “Fox & Friends” TV host Pete Segseth says on TV that he hasn’t washed his hands in 10 years, adding in placing a second foot in mouth, “Germs are not a real thing. I can’t see them, therefore they’re not real.” He claimed later via Twitter (of course) that he was only joking and then returned to his real job of bashing Democrats, but here’s the punch line: he was President Trump’s frontrunner to replace soon-to-be-fired VA secretary David Shulkin. Imagine a guy who is running a sprawling medical enterprise like the VA who throws out comments like that, even if he is kidding.
“A company won a KLAS Best in Category and attended the KLAS event this week, but its attendees weren’t allowed to go on stage to receive their award because they weren’t wearing sport coats.” That might be the most bizarre thing I’ve heard this week.
“I was talking to someone fro the since-acquired HIMSS Analytics about their physician clinical data. Turns out they only have information for hospital and employed doctors – they don’t know anything about independent practices.”
“Is it just me or are some of these HIMSS Social Media Ambassadors losing all semblance of self-control? What is wrong with these people?” Some of them are like kids turned loose on Disneyworld after chugging a two-liter Mountain Dew, but HIMSS chose unwisely in anointing one highly questionable guy who doesn’t even seem be at the conference – his entire HIMSS-related output since the conference started is one retweet. Therefore, he’s my favorite one.
Observations

I haven’t been to a HIMSS conference opening session for a couple of years (because they promised to be dull or vendor-led). My observations:
- The slick media show that played before the session began was all about HIMSS, its influence, its acquisitions, and its grand plans to stick its nose into every aspect of health and healthcare. Gone are the days when a series of quaint PowerPoints were running that listed its committee members, Life member and Fellows, local chapters, and volunteers. It was a celebration of being large and influential rather than giving credit to the members who pay dues, attend events, and serve on committees.
- HIMSS should be renamed HIS (Health Information Society) since Management Systems (the MS part of its name) has disappeared from the agenda and maybe as a career discipline since its 1980s heyday. Instead, HIMSS has decided that the “information technology” part of its mission statement will be split as “information and technology.”
- HIMSS sees itself as an advisor, enabler, and media powerhouse, all of which sound like for-profit activities even though HIMSS is a non-profit.
- The musical act was harmless enough, with a gospel choir of probably Disney day-jobbers singing dad rock (granddad rock, actually) in the form of Queen’s “We Will Rock You” and “We are the Champions” as the HIMSS logo throbbed obscenely in time with the music.
- HIMSS pointlessly paraded its caped poster children Champions on the stage – where they danced awkwardly for a few seconds before thankfully getting off – and just seeing one of them who has been relentless with self-promoting tweets and selfies made me recoil physically. Probably nice in person, but unaware or unconcerned about an obvious need for constant attention.
- The opening keynote celebrated the accomplishment of moving the industry from paper to electronic records, failing to look at the flip side of billions in taxpayer-funded incentive payments and the failure of that expensive technology to improve cost and quality.
- Karen DeSalvo is a gem, whether she’s working in health IT or public health, and Aneesh Chopra seems fun and enthusiastic.
- I really disliked having talking points popping up on the screen beside the speaker’s image. Reason: the practice reminds me that they’re just reading their presentation.

Mayo Clinic CIO and HIMSS board Cris Ross, MBA (he’s not a doctor, despite what some Twitterers seem to think) was an outstanding speaker in describing his transition from helping get Epic implemented to seeing it used by his caregivers for treating his newly diagnosed cancer. He seemed genuine, empathetic to others who are facing a cancer journey, and optimistic about technology’s potential role in improving care.

Our booth traffic was nearly non-existent today, the day in which we had to choose booths for HIMSS20 (for which we’ll always get the dregs given our lack of HIMSS spending). I’ve long questioned whether the high cost of exhibiting is worth it for little guys like us with no HIMSS vendor points, low budgets, and non-existent ROI, so I pulled the plug on exhibiting at future HIMSS conferences. The Smokin’ Doc will be no more, at least in standing guard in his own space. A reader said I would get far more value from having someone drop by vendor booths to explain the benefit of supporting HIStalk, so maybe that’s an alternative.
Speaking of dead exhibits, I can only imagine what it was like in the beyond-7000 sections past the food court. I doubt many attendees are noticing the signs begging them to keep going beyond the fake ethnic food booths.
It takes me at least five hours to recap my day here, so I’ve learned to hightail it out of the exhibit hall when it closes (or earlier) and get to work. Last night it was cheap Chinese and a burger the day before that, so who knows what culinary delights await tonight? The lunch madhouse at the convention center was as crazy as usual – long lines to buy overpriced and over-processed food, then the pleasure of eating it standing up next to a restroom door because the demand for seats exceeds the supply by fivefold.
Thanks to the reader who dropped me off a great backpack. It has been invaluable.
Show floor notes:

Connection put out games and supplies for attendees to bag up for patients in the local children’s hospitals. I did it and it was quite satisfying. Good job.

This nice lady whose name I forgot to write down insisted that I try the smoothie she had made. It was delicious, something with strawberries (and I don’t usually enjoy smoothies).

I still can’t grasp pairing Centricity with Athenahealth, but the deal has been consummated.

Meanwhile, I guess Athenahealth had already paid for its large space before it was led away on a leash, so it was turned into a basement rec room with basically nobody stopping by. Although to be fair, its bad booth location at HIMSS18 and installing Jeff Immelt as Jonathan Bush’s bumbling chaperone had already killed off the massive crowds that Athenahealth had drawn every year before the mess started.

Here’s the MedData scone schedule. It includes the great pumpkin and cranberry orange that I’ve had before, but omits the best flavor of them all – their passion fruit.

Epic always has calculatedly weird stuff in its booth, but this guy is creepy.
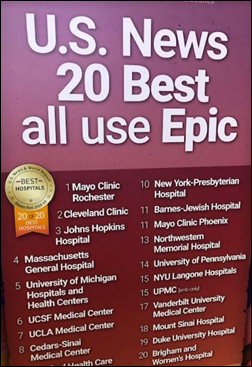
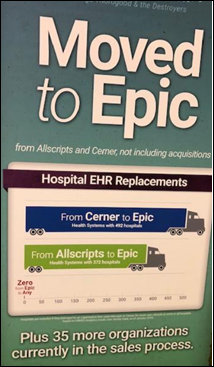
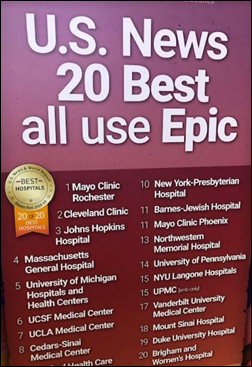
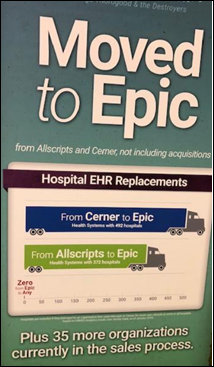
Epic marketing posters. I didn’t get a shot of the one that said 80 percent of medical students or something like that are trained on Epic.
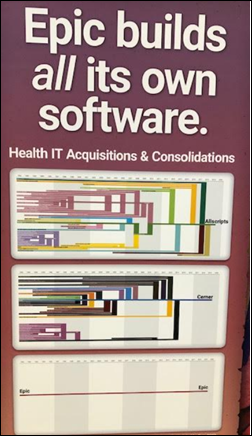
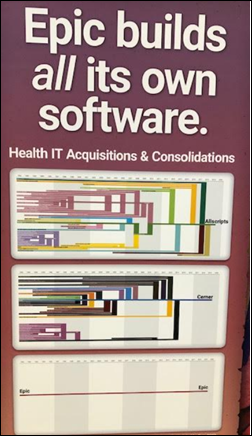
This Epic poster includes a footnoted credit to healthcare equities guy Constantine Davides for his laborious plotting of the acquisitions over time of Allscripts, Cerner, and Epic (also crediting HIStalk since I ran it a few years ago and it was a big hit). Epic is picking up the torch in keeping the graphic updated, for obvious marketing reasons. Constantine is now at Westwicke, which was itself recently acquired.
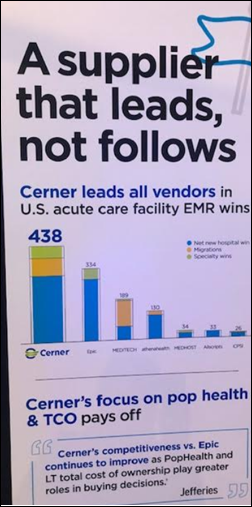
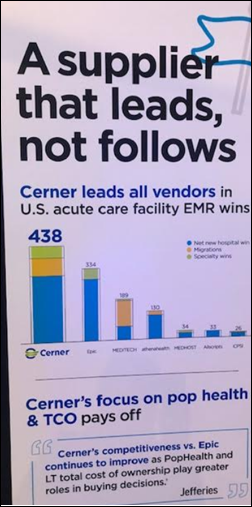
Here’s what Cerner had to say on the matter.

I remember years ago when Voalte’s tiny band of mostly industry newbies blew into the HIMSS conference bedecked in shockingly Pepto-Bismol colored pants. Voalte’s booth has grown along with its business and its people are now experienced, but the company has admirably continued to use pink as its trademark – you can spot someone from Voalte from way down the hall.
Ellkay keeps honeybees on its roof, co-founder Lior Hod is the proud head beekeeper, and there’s always beekeeper’s gear around the office so visitors and the children of employees can visit the hives (they almost brought a live hive to HIMSS19). They have honey in their booth along with cool graphics and really nice people (thank goodness their “data plumbers” tagline didn’t steer them toward carrying plungers while wearing low-rider pants).
AxiaMed has the nicest people I’ve ever met in a HIMSS booth. They offer a patient payments solution, and in my case anyway, some cool argyle socks.
AT&T was doing a demo of using Magic Leap virtual reality during surgery.
What I didn’t see today:
- The usual magicians from Hyland and Cantata Health. The former used a different guy and I assume that the amazing Bob wasn’t at the Cantata booth that I couldn’t find. Update: a reader says Cantata, like quite a few other vendors, took a meeting room rather than a booth, so no more Bob.
- Booth babes, at least not any obvious ones.
- Demos involving hospital beds and non-clinicians wearing scrubs or white lab coats.
- Food offered in booths during happy hour.
What I did see: people filming and recording everywhere, getting in the way of everybody else to record material that nobody cares about. And the same handful of “pay us and we’ll show up in your booth and promote it” folks.

People of mobile device sterilizer vendor Seal Shield let me down in having non-clinicians running around in scrubs. I know it seems innocent enough, but clinicians earn those scrubs every day and resent having them worn by laypeople as conference costumes. They may actually be so turned off that they’ll seek out your competitor. You have been warned.

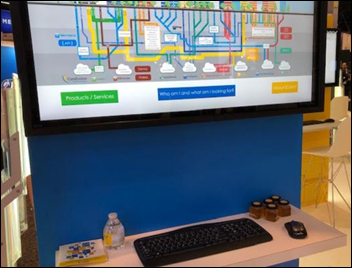
This was over the top but kind of cool, although I don’t remember the vendor (which may say a lot). Update: a reader says its Intermountain Healthcare, something to do with launching an incubator / investment arm like every big health system seems to be doing (although Intermountain missed the unicorn in their back yard, Health Catalyst).
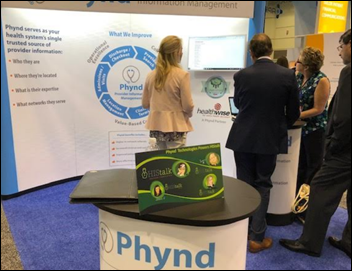
Thanks, Phynd, for featuring our sign so prominently.
Identity Automation had a photographer and studio-type setup for taking professional headshots, for which demand should be high given the awful profile pictures I’ve seen on LinkedIn.
Google Cloud, Microsoft, and Amazon Web Services all had big crowds in their booths.
NextGen Healthcare gave me a quick look at its mobile EHR app, which despite some questionably motivated and questionably insightful recent praise, looked just fine, but not anything a knowledgeable observer would consider game-changing. In fact, NextGen didn’t even develop the app – they got it when they bought the money-losing Entrada for $34 million a couple of years ago.
A reader asked me to report on Nuance’s “AI-Powered Exam Room of the Future” demo room. It was about what I expected since I saw something similar from them last year and liked it – a doctor conducts an entire patient encounter using only voice, in which speech recognition converts lay terminology to medical (and vice versa) to create a progress note, structured documentation, and orders, all ready to be signed. Voice biometric authentication is part of the package as well, as is a wall-mounted bank of 16 microphones that can sense location (such as which leg the doctor is examining). My recommendation – the instructions the “doctor” was rattling off to the patient were full of timelines, activities, and drug names – the doctor could send the voice recording or the layperson transcription to the patient to reinforce what they were told but likely forgot. Patient advocates should pick up that charge, although doctors probably fear malpractice exposure.
Speaking of which, I haven’t heard anything about the “voice assistants” that were all the rage at HIMSS18. Maybe they’ve graduate to actual use in the field already.

Here’s your mysteriously unsung hero of the conference and of the last several years of health IT. Grahame Grieve is the always-modest guy who is basically the father of FHIR (at least as I understand it, but I’m sure one could argue the point). Think about that – one guy from Down Under makes it happen that Apple can develop health apps, that vendors can offer third-party APIs and apps, and that systems can exchange information to the point that the federal government becomes FHIR’s cheerleader. You can’t tell me this guy hasn’t done more than many of the self-important suits running around, yet he never demands credit or recognition and hasn’t earned a dime from his work. Did you hear when I said Apple? Do you get what we wouldn’t have without FHIR? Nearly everything you need to know about today’s interoperability opportunities and challenges are made clear in my 2015 interview with him. I asked him a final question of what he would wish for if he could wave an interoperability wand and he brilliantly said (or perhaps predicted), “I wish the clinicians would believe in clinical interoperability the way that the IT people believe in IT interoperability. We’ve had doubters in the past, but pretty much everybody believes in it now if only we can get there. I wish the clinical people thought that that was a clinical problem.” To which I might add, “I wish health system executives would see interoperability as a responsibility to their patients, not as a threat to their bottom line.”

At least it was your apostrophe rather than your heart that was misplaced, HIMSS.

This is kind of a fun look and appropriate, too.

Brilliant, not to mention self-designed. I believe we may have struck a distribution deal.
I had a quick theater demo of an Alexa-powered patient scheduling app from EMedApps. It was OK, although the generic wording of “provider” as recited to the home user is awkward, even though we as industry people haven’t figured out the best term to refer to the alphabet soup of licensed people who could see a given patient.
I had never hood of Hook, a three-year-old company that connects to Epic and Cerner (via FHIR API and Sandbox, respectively) to present a single view of a patient’s information that can be filtered, sorted, and searched. NYU Langone is piloting and the company is looking for more sites.
CITI Healthcare offers data migration and has an app on Epic’s App Orchard. Steve was a good guy there.

The younger crowd represent with skin-tight suits, wild shoes, and diligently differentiating accessories like bow ties. Those of use whose youth is behind us can attest that when we, too were trying convey confident rebelliousness by ironically dressing and acting the same way, that practice itself was obvious form of confidence-lacking conformity. I like that HIMSS is targeting the early-career folks with their own social events – let’s make them feel welcome. We’re at that interesting point where the people who created health IT from punch card readers and 80-character terminals are retiring and throwing the flag to those behind them.
My goal of the day was to get vendor-offered socks, especially the loud and unusual kinds. Sometimes they handed them over generously, sometimes they stiffed me in saying that the front-and-center displayed socks are for prospects only (hey, if it’s on the podium, it should be fair game), and in Intermountain Healthcare’s case, I couldn’t score a pair of the cool Life-Flight socks because the lady working there was deep into some kind of technical struggle from which her gaze did not avert.

I was surprised that the AMA had a happy hour bar going. But then again, just about every booth had a happy hour bar going.
Someone asked me at the end of the feet-ruining day what I saw as the big themes. I’m not sure I saw any so far, but I’ll say:
- I saw few claims of old systems being suddenly AI-powered, and in fact not many companies were pitching AI at all and most of those that did were obviously using the term in a marketing rather than technical definition (they don’t actually have it, in other words).
- The term “big data” was spoken by no one, having been yesterday’s tired fad (again, a marketing term than a technical one).
- Certainly the new proposed CMS rule has diverted a lot of industry attention right as the conference started – it’s a huge document to digest and it has big implications to both providers and vendors.
- Vendors didn’t seem all that excessive in their booths, although maybe I’ve just become immune to it.
- I didn’t see all that many booth staffers screwing around with their phones or huddling for inter-employee chats instead of paying attention to visitors. In fact, I saw vendors having pre-opening scrums, going through orientation checklists, and describing the goals of the company to everyone involved.
- It felt like maybe people are starting to see the HIMSS conference as more of a boat show distraction with the ever-present government action discussion thrown in and little of substance in between. Maybe system selection has been rationalized, health systems have locked in with their preferred vendors as those health systems expand, and the huge unknowns of genomic science and artificial intelligence fighting for air time with lack of interoperability (or lack of a market for it), questionable usability, and uncertain ROI. We’ll see if the HIMSS attendance – announced tomorrow, probably – is trending up or down (they predicted more than 45,000).
- The US health non-system is not sustainable and expensive technology hasn’t improved cost or outcomes despite those neon gulches of previous HIMSS conferences in which vendors claimed to have the solution for every problem du jour. As Mike Leavitt said in today’s opening session, you can’t be on the world’s leaderboard if you’re spending 25 percent of your GDP on healthcare.
Tell me – what should I see or do Wednesday that would rise above my trite observations about booth snacks or lack of magicians?





























































I use a wiki and was exploring some of the extended character sets. I was startled to learn that the…