Monday Morning Update 8/10/20
Top News
VA OIG looks at how VA facilities and its community providers use HIEs.
The report finds that all 140 facilities have access to VA Exchange and VA Direct, but only 28 are using the latter because they weren’t offered training from DirectTrust or none of their community partners are using DirectTrust.
Twenty-two of 48 lower-acuity facilities still exchanging information via scanning, faxing, or mailing.
Users of Joint Legacy Viewer complain about cumbersome sign-on and poor data quality.
VA has 56 contracted VHIE community coordinators, but noted high turnover and engagement that “ranged from a high level of participation to little or no participation.”
OIG concludes that the Cerner implementation will improve the ease of exchange among VHA, DoD, and community providers.
The report recommends that the VA review barriers to using VA Direct, evaluate VA Exchange and VA Direct training programs, increase the number of community partners including other HIEs, and evaluate the work of the VHIE community coordinators. The VA accepted all four recommendations.
Reader Comments
From All the Marbles: “Re: newly rich Livongo executives. Does it even matter since they were all loaded before?” I’m speculating since I don’t know what it’s like having that kind of cash, but my reaction:
- Assets, not income, makes you wealthy, since you then have financial autonomy that nobody can take from you. Whoever signs your paycheck could stop doing so tomorrow. These folks are set for life.
- Everybody can find ways to spend ever-increasing amounts of money, but at some point pretty early in the wealth continuum, diminishing returns would kick in and the pleasure of buying a fourth house or third luxury car wouldn’t provide much of a thrill. I speculate that money makes things easier to some point, then starts making them harder and causes stress over losing a chunk of it via bad investment.
- Self-made people with big fortunes feel the psychological need to prove that earning it wasn’t a fluke, so they rarely sit poolside like a trust fund brat knowing they can’t outspend their interest and instead try new ventures (either the rich-person’s hobby kind or something a team can run day to day for them).
- I suspect rich, older folks realize that you don’t see hearses pulling U-Hauls, so they look for benevolent ways to publicly spend their money instead of bringing out the worst in squabbling, greedy family members.
- Everybody has some magic number that, given their personal expenses and ambitions, would allow them to live out their days comfortably free of job worries. In that sense, just as time is money when you’re making it, money is time when you want to stop making it. That might be a $1 million net worth for one person or a $50 million net worth for another and the combination of risk taken, luck, and the time value of money is what will or won’t you there, hopefully in time to enjoy the result. I suspect that every one of those newly minted Livongo centimillionaires passed that point long ago, so while I’m sure they are thrilled to be sitting on an even larger embarrassment of riches today than last week, it won’t change their daily lives.
From Prime Spot: “Re: hospital parking. Lots of Twitter chatter about how it’s expensive and unfair to charge patients and families to park.” Hospital parking is always a mess, and I was shocked the first time I took a job with a health system that charged employees and even visitors for parking. My reactions then:
- Hospitals never have enough parking due to an absurdly large number of employees, doctors coming and going, patients and visitors coming in for ambulatory services on the same campus, and car-driving salespeople running around all over the place. We did an analysis of where employees and visitors were parking off campus and it was shocking — they would walk a half-mile to park in a residential neighborhood, either to find an available space or to avoid paying.
- Sometimes as an employee you can’t get a spot even though you’re paying monthly for one, and if you’re really unlucky, you might get relegated to offsite parking that involves a bus ride each way that isn’t nearly as nice as its off-airport counterpart
- Hospital and university transportation services departments, like most bureaucracies, keep finding new ways to spend money on employees, vehicles, and infrastructure because they seem themselves as generating big profit, and all of that profit comes from permits and tickets.
- Hospital garages and parking lots are often located in areas where unrelated parking is in high demand or as part of a school where students will take up any available space, meaning that visitors wouldn’t get a spot if the per-hour charge wasn’t a deterrent to those with less motivation. Hotels charge paying guests $40-80 for overnight valet parking given the same demand with lack of alternatives.
- Hospitals sometimes don’t own their on-campus garages or contract out parking / valet services (I always picture mob involvement).
- It’s always funny that despite all the ways hospitals extricate money from patients under sometimes questionable circumstances, the only services for which bitter comparisons are made are parking and cafeteria.
- I personally would avoid on-campus appointments whenever possible, foreseeing sitting in traffic amidst impatient employees and lost visitors and then hiking quickly knowing I’ll be late (assuming I even know where I’m going from the bowels of the parking garage, like the “follow the yellow lines to the blue elevator, go up one floor, then cross the annex bridge and go down one floor” kind of hospital directions). I don’t like having my first aggravating customer experience before it even begins. Buy a dying mall and stick your doctors there.
HIStalk Announcements and Requests
![image[88]_thumb image[88]_thumb](https://histalk2.com/wp-content/uploads/2020/08/image88_thumb.png)
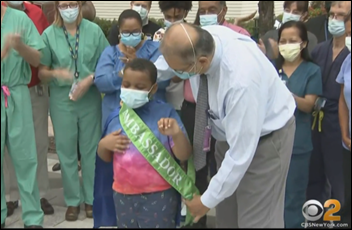
HIMSS21 attendance is, for the most part, out of the control of HIMSS and instead will be driven by pandemic status, poll respondents say.
New poll to your right or here: For those assigned to work from home: would you return to campus if the company required it in the next few weeks? Basically a yes/no answer is the only one an employer will offer, so do you feel strongly enough about not returning that you’ll accept termination for refusing?
Thanks to the following companies that recently supported HIStalk. Click a logo for more information.
![image_thumb[59]_thumb image_thumb[59]_thumb](https://histalk2.com/wp-content/uploads/2020/08/image_thumb59_thumb.png)
Several readers saw my mention of new Donors Choose projects and sent generous donations to fund another round of them, with their dollars boosted by matching funds from my Anonymous Vendor Executive as well as third-party matching sources. Here’s what I fully funded:
- A document camera for Ms. E’s elementary school class in Salinas, CA.
- A webcam, laptop stand, and wireless keyboard for Ms. H’s elementary school class in Timbo, AR.
- Lighting, headset, device mount, and easel for Mx. Smith’s third grade class in Las Vegas, NV.
- Digital resources for Ms. G’s elementary school class in Seagoville, TX.
- Digital resources for Ms. D’s kindergarten class in Hoskinston, KY.
- Five headsets for Ms. S’s elementary school class in Santa Ana, CA.
- Daily journals for online sharing for Ms. M’s second grade class in Oxnard, CA.
- Math manipulatives for remote learning for Ms. S’s elementary school class in Waco, TX.
- Classroom supplies for Ms. D’s middle school class in Collinsville, IL.
- Flocabulary vocabulary learning for Ms. H’s elementary school class in Las Vegas, NV.
- Digital resources for Ms. R’s elementary school class in Philadelphia, PA.
- Agriculture books for Ms. J’s middle school class in Kinston, NC.
- Math manipulatives for Ms. F’s elementary school class in Wyandanch, NY.
- 50 take-home library books for Ms. C’s elementary school class in Calumet City, IL.
- 25 sets of headphones for Ms. S’s elementary school class in Houston, TX.
- A document camera for Ms. E’s elementary school class in Steelton, PA.
- Remote video learning equipment for Ms. R’s elementary school class in Oklahoma City, OK.
- Social distancing and teaching supplies for Ms. B’s elementary school class in Irving, TX.
- A document camera for Ms. T’s elementary school class in Apopka, FL.
- Sight word games for at-home use for Ms. C’s elementary school class in Hempstead, NY.
- A webcam, microphone, and earphones for online instruction for Ms. T’s middle school class in Chicago, IL.
- Online language proficiency tools for Ms. M’s elementary school class in Fairdale, KY.
- Digital social studies content for Ms. K’s middle school class on Connellsville, PA.
- Lighting for teaching virtual classes for Ms. T’s elementary school class in Mission, TX.
- STEM kits for Ms. A’s kindergarten class in Sacramento, CA.
- Headphones and a USB camera for Ms. N’s elementary school class in Harbor City, CA.
- A USB headset for Ms. B’s elementary school class in Kenner, LA.
- Take-home math materials for Ms. H’s elementary school class in Madera, CA.
- 20 magic boards and binders for Ms. M’s elementary school class in Chicago, IL.
- Math and science books for recording for online lessons for Ms. P’s elementary school class in Philadelphia, Pa.
Webinars
August 19 (Wednesday) 1:00 ET. “A New Approach to Normalizing Data.” Sponsor: Intelligent Medical Objects. Presenters: Rajiv Haravu, senior product manager, IMO; Denise Stoermer, product manager, IMO. Healthcare organizations manage an ever-increasing abundance of information from multiple systems, but problems with quality, accuracy, and completeness can make analysis unreliable for quality improvement and population health initiatives. The presenters will describe how IMO Precision Normalize improves clinical, quality, and financial decision-making by standardizing inconsistent diagnosis, procedure, medication, and lab data from diverse systems into common, clinically validated terminology.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Sales
- NIH will extend its use of OpenText’s Content Suite and AppWorks for electronic document management and workflows.
- Transaction Data Systems chooses Waystar for claims processing by its independent pharmacy customers.
People

Mee Memorial Healthcare System (CA) promotes Rena Salamacha, MS to CEO. She previously served as IT director, CIO, and chief strategy and technology officer, COO, and interim CEO.

Lisa Crymes, MBA (Change Healthcare) joins Preventric AI as chief marketing officer.
Announcements and Implementations
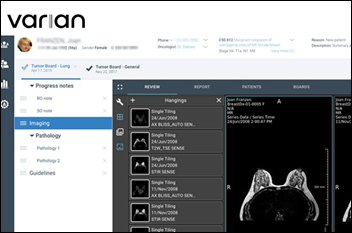
Elsevier expands its integration of its ClinicalPath (formerly Via Oncology) oncology decision support tool with Epic, including launching from Epic using SMART on FHIR, applying cancer staging data from Epic, navigating within Epic, queuing up treatment within Beacon protocols to reduce manual order entry, and documenting details as a note.
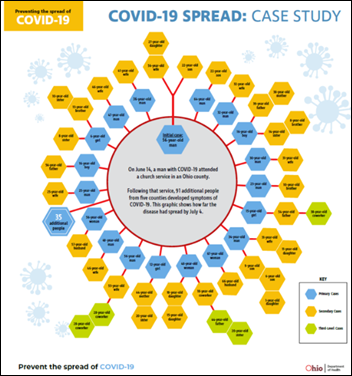
COVID-19
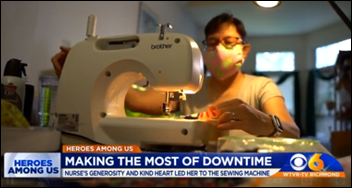
![image[94]_thumb image[94]_thumb](https://histalk2.com/wp-content/uploads/2020/08/image94_thumb.png)
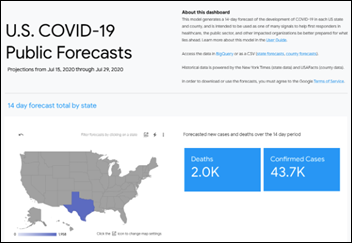
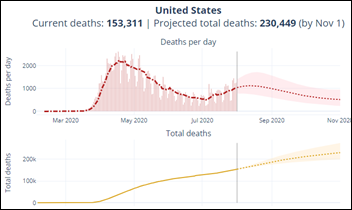
A New York Times analysis of CDC’s count of higher-than-expected death counts – probably caused by COVID-19 along with the situations it has created – at over 200,000 from March 15 through July 25 versus the official count of 161,000. This is a good full-impact number that would include the pandemic’s effect on stress, failure to seek medical care for other conditions, financial challenges, and failure to correctly account for deaths. I assume that it this number would also be subject to undercounting given the presumable decrease in deaths by accidents.
The field hospital created at Sacramento’s Sleep Train Arena sees just nine patients in 10 weeks, with $12 million in cost from rent paid to the Sacramento Kings, facility upgrades, and payment to 250 staffers. One traveling nurse company billed $428,000 to provide five pharmacists and five pharmacy technicians. Those involved say there was never a real plan on how to integrate with possibly overburdened hospitals and the state admits that it should have used local data to determine how to set up its 15 field hospitals.
Bill Gates says US COVID-19 tests are “complete garbage” because of delays in getting results, suggesting that paying companies for them only if the results come back in 24-48 hours would “fix it overnight.” He is optimistic overall, however, predicting that diagnostic and therapeutic innovation in the “rich world” will end COVID-19 by the end of 2021, with the rest of the world following a year later. However, he says it will take years to bring the global economy back to the levels of early 2020. He also notes that he would want remdesivir or dexamethasone today if hospitalized for coronavirus, but in 2-3 months the tool chest will expand with other antivirals and antibody therapy.

It’s been a busy COVID-19 week for one Georgia high school:
- The school suspended two students for taking a photo that showed a packed school hallway and sharing it to social media.
- After a national outcry, the school lifted the suspensions.
- Six students and three employees reported to the school that they had tested positive.
- Two brothers who reported experiencing symptoms were found to have gone to school Monday without wearing masks or social distancing, with a family member saying they didn’t realize the severity of the virus and weren’t encouraged to wear masks.
- The school moved to distance learning only for Monday and Tuesday while awaiting the results of contact tracing. They have told parents that they will notified Tuesday evening whether in-person instruction will resume.
Other
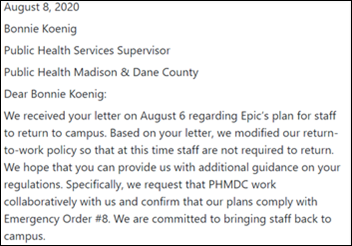
Epic changes its Monday mandatory return to campus, allowing employees who feel that their personal situation makes it unwise for them to return safely to campus to continue to work from home while Epic awaits further guidance from the county health department. Epic says Cleveland Clinic, a public health expert, and an epidemiologist are reviewing Epic’s plan, which originally called for bringing the first group of employees back to their offices on Monday and all employees working on campus by the end of September except for those at high risk, who could request an extension through November 2.
China’s Communist Party newspaper warns readers to “beware of health-tech firms’ snake oil,” which is pretty good advice. Its points, as written by a health policy lecturer in the London School of Economics:
- Big US tech companies have promised that analytics and AI will reduce costs and improve outcomes, but individual patient data is subject to subjective clinical judgment and is often plagued with missing records and lack of standardization.
- Those big US tech companies don’t know much about healthcare, and they rarely back up their black box algorithms with studies that prove their value.
- Predictive models are only as good as the data they are given, and since their assumptions are based on what is already know, they are best at reviewing the past and present rather than predicting the future.
- AI developers are, intentionally or not, just as biased as the rest of us, and using current healthcare data makes those systems prone to replicating past failures and successes.
- Hospitals and regulators shouldn’t just turn over patient data to developers – they should be actively involved in the design and deployment process.
Sponsor Updates
- The Dealmakers Podcast features PatientPing co-founder and CEO Jay Desai.
- Pure Storage’s Pure Good Foundation celebrates its fifth anniversary and announces that it has raised $2.3 million for charitable contributions.
- The Voice First Health Podcast features Gabe Charbonneau, MD and his use of the Saykara AI Assistant.
Blog Posts
- Addressing key questions and misperceptions of the 2021 E/M changes (Nordic)
- How to Beat the Prescription Drug Discount Card Game (OmniSys)
- Purpose Born of Frustration (OptimizeRx)
- From High Touch to High Tech: 5 Key Factors That Will Drive the Trajectory of Telehealth (Pivot Point Consulting)
- Better, Stronger, Faster: Leveraging the Amazon Cloud to Scale to the Demands of Telehealth (PMD)
- Five Reasons Health Systems are Prioritizing Integration with Specialists (Premier)
- (Re) Introducing Single-Sign On (SSO) (Redox)
- Why Remote Work is Not the New Normal (SailPoint)
- How healthcare prepares for cloud computing (Spok)
- Krames on FHIR: Blazing a trail in personalized patient education (StayWell)
- CMS Price Transparency Rule is Fast Approaching (Surescripts)
- Marketers, Clinicians, and Care Managers in the Patient 360 Ecosystem (SymphonyRM)
- Tufts Medical Center Elevates Human Experience in the Midst of the Pandemic (Vocera)
- How Advertising on LinkedIn Can Help Drive Patients to Your Physical Therapy Clinic (WebPT
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.











































 .
. 













Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…