Curbside Consult with Dr. Jayne 12/21/20
A recent article on telemedicine, privacy, and information security caught my eye this week. It appeared in the Journal of the American Medical Informatics Association. Although it’s not a write-up of a blockbuster study, it brings up some important points that we need to address as we move forward with new ways of delivering healthcare.
Even with vaccines on the horizon, there will still be a need to deliver care with reduced contact for the foreseeable future. Health systems and providers have made major leaps forward. One of my CMIO colleagues notes that it took her system less than 60 days to roll out an implementation that they had planned to take more than 18 months. It’s amazing what can be done when resources are focused on a single project since most of us are used to trying to manage dozens of projects that move forward an inch at a time. The reality, however, is that many projects were likely sidelined in favor of the one, and I bet the re-prioritizations were interesting when projects were reassessed through the lens of a global pandemic.
For organizations that didn’t already have a plan to roll out telehealth, many went with whatever solution they could take live quickly, especially with government waivers allowing non-healthcare solutions such as FaceTime, Facebook Messenger, and more. Zoom has been heavily used, but the phenomenon of “Zoom-bombing,” along with encryption concerns and the inefficiencies of a freestanding system, have led provider organizations to look for more robust solutions that integrate with EHRs and scheduling systems.
Broadband continues to be a barrier in several areas, and even in areas with good coverage, there can still be outages. I experienced this first hand this week as my internet was down for nearly five days as AT&T came up with different troubleshooting strategies and failed solutions before it finally was resolved yesterday. If I had been trying to practice telehealth this week instead of in-person care, it would have been a nightmare. When I was finally able to schedule a rep to come and assess the situation in person, I had an in-person shift and was only able to get back online by having my favorite retirees come house-sit.
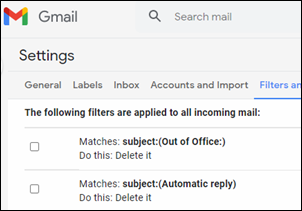
The article also had good discussion of privacy and security concerns, including the ransomware attacks that continue to plague health systems. They cited recent research which showed that employee workload has a major impact on the rate at which employees are likely to click on phishing links. Increased use of broadcast email announcements was noted as a risk for increasing workload.
One of the organizations that I work with sends entirely too many broadcast emails and doesn’t pay much attention to crafting crisp subject lines that allow employees to prioritize their reading. They also overdo the “high priority” flag and haven’t figured out to focus the audience for different emails to send a more effective message. Maybe when I finish their informatics consulting engagement I can convince them that they need more routine management consulting-type services.
There’s a technical component to privacy and security that gets most of the focus, but especially when many of us are in work-at-home situations, there needs to be more focus on the need for physical safeguards. From the number of calls I’ve been on during the last few months where small children and significant others have come walking into the middle of the call, I’m guessing there is a shortage of locks on home office and bedroom doors. Some of the calls where this happened have involved discussions of protected health information, including quality review of patient visits, so having people potentially present who have no right to the information is a concern. Perhaps a corporate policy to require that headphones be used when discussing PHI would be an easy fix as well.
One of my clients tackled the issue of people working at home by setting the idle time lockout for all their laptops at 90 seconds, which is pretty short if you’re doing work that involves flipping through written documents and taking notes on your laptop, or if you’re using multiple computers to perform different tasks while working on a project. It also discourages sitting there thoughtfully reading an email before replying, which is a skill that the world could probably use more of. I was going to try a USB “mouse jiggler” to get some relief, but enough people complained that they relaxed it a bit. For someone working in an otherwise empty house, it’s still a little short for my taste, but at least I could stop entering my password dozens of times each day.
Thinking about how technology should evolve to keep up with telehealth led me to consider other ways in which telehealth may want to evolve. Many organizations encourage their telehealth providers to wear their white coats while on camera as a sign of professionalism. I always feel a little weird doing this, since for me the white coat is a tool that I absolutely don’t need while at home seeing patients on my laptop. In medical school, my white coat was stuffed full of everything I could possibly need for patient care – depending on which service you were on, it could contain an otoscope, ophthalmoscope, reflex hammer, stethoscope (although that was normally around students’ necks since our pockets were so full), penlight, multiple ink pens, patient notecards, reference books, and more.
As physicians progress in their training, the contents of the coat are reduced and more specialized. Right now, my in-person coat typically contains a stethoscope (there’s no way that thing is ever going around my neck again in a post-COVID era), single pen, lip balm, and a pocket full of gloves since we had to take them out of the exam rooms because patients were stealing them. I don’t need any of those things to practice telehealth, and it just seems contrived to be sitting in front of a bookcase in my house wearing a white coat. I’m pretty sure patients who are calling in for my urgent care services don’t care what I’m wearing as long as I seem competent and do what I can to help them.
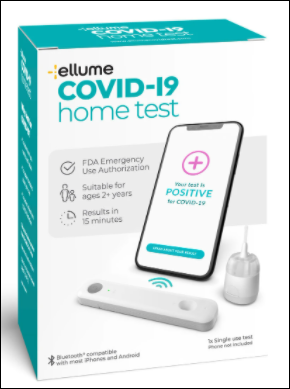
I can’t wait to look back on this post a year from now and see where telehealth has taken us. Will we have evolved to a place where patients have home monitoring and assessment devices and physicians are able to really diagnose and treat like they would in person? Or will we still be using creative exam strategies to get the information we need? Will there be a physician-enabled camera filter that can take the bags from under my eyes and remove the semi-permanent mask marks from my face? Only time will tell.
How do you think telehealth will evolve for the future? Leave a comment or email me.

Email Dr. Jayne.






























There was a time when my company went through multiple rebrands. These were relatively minor shifts, but completely unnecessary. It…