Brian Yarnell is founder and president of Bluestream Health of New York, NY.

Tell me about yourself and the company.
I got started in healthcare 10 years ago. Prior to that, I worked in digital media, consumer behavior, and data-driven analysis for retail, manufacturing, marketing, and sales. I have quite a bit of background dealing with consumers and big data. I sold my first health tech company about seven years ago to Hillrom. That was a business called Starling, where we built a replacement for a nurse call system that routed out throughout the hospital and used intelligent workflows.
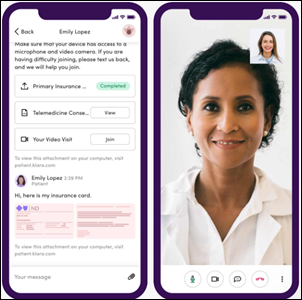
We shifted gears and founded Bluestream after that, with the idea of figuring out a better way to bring real people, through video, to a patient’s bedside. At the time, we didn’t really anticipate what was going to happen outside the hospital. We were thinking through how we could better provision these relationships between a remote provider and a patient.
Providers rushed to offer telehealth services via whatever video platform was quick and easy to roll out, but the novelty of interacting with patients by video has worn off. What virtual health platform capabilities are needed to provide a good patient and clinician experience?
Things have evolved fairly quickly. I think of it as a continuum. Those technologies that you mentioned were effectively video, which is a commodity at this point. Beyond the basic video connection, things have evolved from telehealth all the way to what I would call virtual-first healthcare. If you think of it in that context, the video piece is the last mile, but it’s really about opening up front doors for patients and meeting them where they are and how they want to be engaged.
The idea of patient portals and downloadable apps has generally not succeeded. The big things that people ought to be focusing on for virtual care is, how do you get in front of a patient, wherever that patient is, and however that patient feels like engaging? Then for clinicians, starting to take some of these brick-and-mortar workflows and make them virtual so that you can do all the great things that you might do in person, but do them remotely.
What elements of a virtual visit most strongly affect patient satisfaction?
We recently added Net Promoter Score, thinking about my marketing background prior to healthcare, to the platform. We know specifically what impacts patient satisfaction. It’s not just the bedside manner of the clinician. It’s what happens when somebody shows up a day early, an hour early, or 20 minutes early for an appointment. You can’t leave people in limbo. You have to be “consumery” in terms of how you engage folks and walk them through this process, even if they show up at the wrong time.
Making experiences that feel like a consumer-driven website. Give people information, expectations, and tools to engage, even if they are not necessarily at the front door at the right time. Then, post-visit, what happens when you wrap up with a clinician? What happens when something goes off the rails and you have to reconnect? All along the way, from showing up early or showing up on time to the visit, dropping the visit, concluding the visit, providing a real framework that still hand-holds the patient and has that consumery feel without being overly technical, overly burdened with lots of bells and whistles.
What virtual options can be offered to patients who have limited technology or bandwidth?
One of the things that we’ve seen as being successful is getting folks like MAs and assistants to tee up the call for physicians. You certainly don’t want the physician troubleshooting cameras, networks, and things like that. But you can have lower-cost, higher-availability resources work with the patient first and do a handoff.
But as you said, some folks aren’t going to get there in terms of tech. What we’ve seen be successful is automation to reconnect these people, to literally point out where you have to click to accept camera permissions. But some folks, like my mom, will never get there, and in those cases, you have to be willing to work with telephones. We’ve seen people doing emergency medicine consults , ET3 [emergency triage, treat, and transport] programs where the reality is that a large portion of the population is going to pick up a phone and dial it. You have to be able to route those visits in with the same attention and same priority as the people who are fully into the smartphones and video.
Health systems initially saw virtual visits as a distraction that should be turfed off to third-party companies that provided not only the platform, but the providers. Now that virtual visits are here to stay, are they treating them more like a full-fledged, branded patient experience?
Absolutely. You hit on a really important point. If you gave a hospital a $1.5 billion a year and a half or two years ago, they would have built a new wing. Now, they have to be thinking about how to build virtual experiences.
These vendors that you talked about that offered a lifeline of virtual visits with the provider network behind it will compete for those patient relationships with the hospitals as the world shifts towards more consumer-facing, on-demand care. The hospitals need to think about how to implement these programs to prevent their vendors from cannibalizing their core business. That becomes important in a transition into a value-based framework.
How does virtual health avoid becoming commoditized, where consumers see all encounters as equal and just choose the cheapest or first-available provider?
Consumers expect it immediately and pervasively. What you’re talking about is this preponderance of front doors that appear to come from all different places.
We and other vendors are starting to equip health systems and traditional healthcare delivery platforms with the ability to cast this wide net. Even though you may come through an insurance company’s website, a phone number on the back of your insurance card, a kiosk in a homeless shelter — very different experiences and a different type of front door — you’re going to start funneling those visits into a common pool provider. People like Teladoc have done that for years. The difference is that health systems are getting smarter about getting in that game and funneling visits from non-traditional places into their provider group.
Healthcare didn’t follow other businesses in looking at the lifetime value of acquiring and retaining a customer. Is that changing?
Absolutely. We have customers all across the spectrum, from people who just pay the bills of ambulatory visits to those who fully participate in these risk-based programs. The more sophisticated folks are looking at the cost of acquisition and the cost of attrition.
What happens when a non-traditional player, such as Walmart, CVS, or Amazon, gets your patient? They’re not coming back. When you get into this modality where you are getting compensated for the cost of keeping the patient healthy, the lifetime value of patients goes up substantially. Smarter health systems, more strategic entities like some of the pay-viders, are playing that game of, how do you capture as many relationships as you can and keep them? Because you want to be on the winning side of that equation of people who are getting paid to manage a population effectively.
How does a health system’s marketing strategy change when those relationships are established during virtual visits and that involve consumers who may not require a health system’s services for a long time?
We’re seeing more sophisticated health systems, even the traditional ones, get smarter about using tools that let them take the providers they already have. A lot of them are large physician employers, and they have a pool of providers. What they don’t have is access to a patient until that patient has a heart attack or gets hit by a car. To empower those providers to get in front of patient, they are establishing commercial partnerships with large, self-insured employers, with insurance companies, and with municipalities that need healthcare coverage in housing projects and homeless shelters. Establishing lots of diverse front doors — whether it’s a walk-in clinic in the inner city or a health clinic in a Federally Qualified Health Center — and proactively identifying.
They cast a wide net to get patients. The branding might not even be their own, but they’ve got to be funneling those patients to the providers that they are already paying to be on the bench.
Are we in the early days of virtualizing the clinician workforce, where most of them already prefer to live in urban areas?
The hub-and-spoke model is a real thing, being able to have centers of excellence and making them accessible to remote communities, whether it’s because they are socioeconomically disadvantaged or because they are physically remote. The big risk is brain drain. You don’t want to be in a situation where you have no local providers who have expertise any more, because if somebody walks into a hospital and needs follow-up care, they want to have a good experience with a local community member. You’ll start seeing some of that shift into more urban hubs or more centralized hubs, and it’s a little bit of a risk.
Most people would be happy if virtual primary could deliver results equivalent to in-person visits. Are areas that can deliver arguably superior outcomes, such as behavioral health and chronic condition monitoring, drawing equally enthusiastic interest?
We do a lot of behavioral health. We do it inside acute settings, like emergency rooms and inpatient units, and we do it outside of acute settings. The big difference is, are you trying to keep someone out of the hospital and from incurring healthcare costs, or are you trying to adequately address somebody’s needs when they set foot in the door? Either case is a big one, low-hanging fruit with an event that has the potential to cost a lot of money and cause a lot of headaches if you don’t address it up front.
Behavioral health is a good one. We see the measurable impact with our customers and our partners. We can bring in a behavioral health expert, such as a clinical psychiatrist, to write an order for a patient in well under an hour, when in an ED, it might otherwise be a one-day or a three-day wait. It’s a big difference.
Outside the hospital, I would lump in behavioral health with access to things like emergency medicine, these mission-critical things that cause people to go to a hospital or to incur additional costs. We have 911 and ET3 programs that drive down the number of visits by 50%. It’s a big deal, and there’s a reason people are focusing there.
Are health systems interested in having their providers virtually help paramedics, long-term care, and home health providers who otherwise don’t have many options except to send the patient to the hospital’s ED?
Definitely, and even more so as you think about the systemic cost of care delivery. New York City Health + Hospitals is one of our customers. They tie directly into the 911 system. They deliver their services down into SNFs. They tie into first responder devices in ambulances and fire trucks.
The underlying theme there is that they don’t want people going to the hospital. So when you dial 911 and it’s not life-threatening, they are going to get you in front of a clinician. If you need a paramedic, they’re going to try to get you virtually in front of a clinician. Even when you show up in person, they don’t want transport you, because the systemic cost of moving someone from a SNF back to the hospital is somewhere in the range of $10,000. You can absolutely prevent that from happening if you have the right safety net in place in terms of clinicians and folks like that.
What changes do you expect to see in the virtual visit concept and in the company’s business over the next few years?
What will drive the evolution of our business as a platform provider, and probably more importantly the business of traditional health systems and payers, is this shift towards value-based care and on-demand access to care. That’s just ubiquitous, and it will be painful for health systems to adapt to do that, because they are used to filling beds and physically getting their hands on people.
There are a lot of new folks coming into the market. Amazon and Walmert are better equipped to present consumers with what they want, when they want it. A lot of work will go into equipping these traditional providers with the tools to rise to meet consumers where they are. The mantra of the American consumer is that “I know what I want, and I want it now.” This notion of trying to make a better patient portal and that type of thing is never going to succeed. You have to give people what they want and then work out how to route these things intelligently and drive critical outcomes from them.
Comments Off on HIStalk Interviews Brian Yarnell, President, Bluestream Health























Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…