Luke Bonney is co-founder and CEO of Redox of Madison, WI.

Tell me about yourself and the company.
I’ve been working at Redox, on Redox, for just about seven years. That’s a long time and a lot more gray hair. Redox is the platform to make healthcare data useful for healthcare’s builders, the people building and scaling healthcare technology.
What have been the most significant interoperability advancements of the past few years?
Our world at Redox is all about how to make healthcare data useful for builders, who to us are the people building and scaling technology and healthcare. We obsess about these people, because through enabling the people who are building technology, everybody will benefit. Patients will benefit, providers will benefit, and you and I will benefit. Great builders build great technology that drives incredible experiences. Those experiences are what drive outcomes. That’s where we need to see meaningful change in healthcare. How do we drive and inspire outcomes?
At Redox, we are constantly obsessing about imagining a world where people can build and scale healthcare technology and be completely unencumbered by the nastiness and complexity of healthcare data, which I know sounds crazy because it is nasty and complex. But we think about a world where with a couple of clicks, people could compose experiences for their users. That’s what we obsess about.
Over the last couple of years, we have continued to focus on healthcare data access and integration. Today, working with Redox means that you have access to existing connections to over 2,500 healthcare organizations across the US and now in Canada. We have integrations with dozens of major payer organizations. We have expanded to not just be focused on clinical data, but financial and payer data, connections into existing clinical networks like Carequality, CommonWell, and a whole bunch of HIEs. We are now connected to 50 out of 50 state public health departments.
We have a lot to be proud of that we’ve focused on in the last couple of years. When we talk to our customers, they say they work with us because we help them focus their engineering efforts and their product efforts on building a truly differentiated product by taking all this nastiness off their plate. We also help them accelerate their sales cycle. We help them get live and implemented faster at all these different locations.
Today, it’s all about data access and integration. As we look to the future of Redox, we will focus on additional problems where we can make healthcare data useful and valuable for builders.
Looking at the industry, I would go to the pretty exciting impact of regulation. I know that might sound weird since regulation is almost always a nasty word, but when it comes to 21st Century Cures, I am definitely in the camp that 21st Century Cures is a game changer, and in a good way. It is definitely not perfect, like any regulation that runs 700 or 800 pages, but it absolutely redrew some of the major goalposts and expectations around healthcare data. The requirements around info blocking and enabling FHIR are good. I think they are incremental. Access is only one component. Standardization and normalization of data are equally if not more important when we think about downstream use cases. We have seen a huge amount of positive change in the impact in the payer world and the payer landscape.
The saying we use at Redox is that what Meaningful Use was for providers, 21st Century Cures, and specifically the CMS patient access rule, is for payers. It has been a major forcing function for payers to modernize their technology. 21st Century Cures is fundamentally making healthcare a friendlier place for builders and innovators by curbing a lot of the power of major incumbents. From where I sit, that is fundamentally a very good thing.
Explain TEFCA and how it changes your business and the industry.
Where I’m super excited about 21st Century Cures, I think TEFCA is a different situation. Had TEFCA been regulated in a way similar to 21st Century Cures, with clear incentives and/or penalties, we would be a huge fan, because we are fundamentally aligned with the world that TEFCA imagines.
To just state what that is, TEFCA has two core components. It’s a technical framework and a legal framework that allows networks to communicate with one another. It imagines what they think of as a network-of-networks environment. We love that. We think that that would fundamentally change the landscape.
However, as it stands right now — and this is where I think there is huge opportunity — TEFCA completely optional. It provides the framework. In an industry where large change is so typically aligned to hefty incentives, reimbursements, and penalties, TEFCA doesn’t have any of that. Maybe the long story short there is that we believe in TEFCA, we believe in the future it imagines, but we don’t have strong confidence that it’s going to meaningfully shift the industry because of how it is structured.
Having said all that, there’s a number of products we support, connectivity to Carequality, CommonWell, and other networks that we support. But we’re just not convinced it’s the game changer.
ONC is reluctant to apply a heavy hand and instead wants to clear the way for market forces to drive advancement. Where would that market pressure come from to make TEFCA universal?
TEFCA has the framework around what’s called a Qualified Health Information Network, a QHIN. Without going into the tactical details of what qualifies as a QHIN, a couple of networks fit that mold at a high level. CommonWell and Carequality would be classic examples. They support a use case, which is the treatment of care or the transition of care use case, where data is exchanged. The classic example is that your primary care doctor is in New York, you’re in Florida, and you get in a bike accident. CommonWell and Carequality allow that record to get pulled from New York to Florida so that the doctors treating you there have your medical history. That’s a clear use case with appropriate incentives for hospitals and clinics to participate.
It’s harder to imagine future use cases where those alignment of incentives occur, where people would meaningfully come to the date table and agree to share data. There’s some compelling stuff around payments and patient payments where there could be meaningful market pressure.
Your question is a really interesting one because while the painted future is interesting and exciting, it’s hard to imagine a path to get there simply through pressure from market conditions. This is where we need to think about the actual incentives of these organizations, their willingness to share data, and whether they see it as the right thing given the specific use case.
Has the original interoperability idea of paying those who contribute data and then charging for its use gone by the wayside?
I don’t think that model is off the table. I just don’t think it has seen a ton of traction. Where there is traction involves life sciences companies that want to pay for large, de-identified data sets for R&D purposes. But beyond that, there just hasn’t been a ton of traction. That is not at all me saying that we should disqualify that or put it to the side. If there was, I think that would be super exciting. Those are the questions that will be interesting to track. Is it going to enable that world or not? Do we see the early signals that something like that could emerge?
Technology vendors, startups, and health systems themselves are finding it profitable to broker a data connection between providers and life sciences companies. Will additional use cases emerge?
I think we are early days. There’s a ton of opportunity. Costs are high to administer clinical trials. The match rate, how easy is it or hard is it to identify patients to enroll in the clinical trials, is still super high and inconsistent. The data itself is part of it. Another huge part of it is decentralized clinical trials, where there’s a ton of innovation.
We are early days. That’s a fun and interesting spot to look for for innovation. Drug companies have lots of money that they are willing to put to work.
Do we have now, or will we have in the future, a healthcare technology ecosystem?
There has always been an ecosystem. It’s the question of how big and how impactful that ecosystem is.
Going back to the conversation around 21st Century Cures, you can look at a lot of interesting data. Look at the total amount of funding over the past five years that has gone into digital health. It has been one of the fastest growing categories compared to any other technology sector over the past five years. That’s an incredible sign that people everywhere see healthcare as not just a place where innovation is needed, but for anybody who has been a patient or provider, that innovation is needed and possible.
We’ve been saying for a long time and with a straight face that there is an ecosystem. Now it is probably more apparent to a growing audience. But we also think that it’s necessary. Like many other industries, there isn’t a single person or a single company that will meaningfully move the needle. It needs to be many people working on many problems.
That is one of the fundamental viewpoints we carry. It’s about empowering this entire class of builders. It hasn’t happened overnight, but it’s much more significant than it was yesterday, and I think three years from now, it will be twice as big. It is super exciting.
Now that cloud has finally found its healthcare footing, including technology companies like Oracle and Microsoft acquiring big health IT vendors, where does it go from here?
I’m glad you asked this question. Big tech is making serious moves in healthcare. For those of us who have been in this space for a while, we’ve seen different moments where bets were getting placed. I now have conviction — and not just me, but others — that fundamentally, healthcare delivery in the US is going to look different three to five years from now because of the impact of Amazon, Microsoft, and Google.
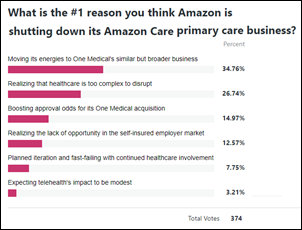
The other thing I would say is that it’s not just big tech, but also groups like CVS, Walmart, and others that are making big moves, such as Amazon buying One Medical and CVS’s purchase of Signify. An interesting detail that stuck out to me when Amazon purchased One Medical is that alongside that, they announced that they are winding down what they had previously been calling Amazon Care, which was their initiative around a nationwide telemedicine offering. That tells me that that Amazon, in this case, is moving out of testing different hypotheses, having multiple bets, and solving for optionality and they are moving into a more unified, aligned approach now that they have been in market for a little while. This is a trend that I see across big tech. They have spent some time studying healthcare and now they are making their big bets.
It’s not just the cloud. It’s the technology companies that offer the cloud that are super interesting. When it comes to big tech and the ongoing shift to cloud infrastructure, this has been a core part of the Redox thesis from the very beginning. Hospitals, clinics, payer organizations, and life sciences groups are all right now making massive investments in their cloud infrastructure. It’s because what they all have is data, and what they are realizing is that these big tech companies and their cloud infrastructure has the most robust functionality when it comes to driving value from that data.
I see big changes. The dollars being spent will threaten some incumbents in the space, because change is always scary. But I also think if we all take a step back and look at it from the viewpoint as a patient, I’m incredibly excited, because this is what has happened in other industries and the end result is ultimately a more user-friendly, consumer-friendly experience. It’s real. it’s big. We are in the midst of it right now, and three to five years from now, healthcare is going to look different.
How will today’s financial market activity change the industry?
On the one hand, healthcare is, and will continue to be, relatively resistant to recessions. As we know, the demand for healthcare doesn’t closely associate with the state of the economy. I would say that overall demand hasn’t changed a ton. Where we do see impact is more specifically related to capital markets and the fact that valuations have come down significantly. Companies that need to fundraise in the short term are finding it harder. This is concentrated in some of the startup and SMB folks. This means that a category of customers and builders in the space that are tightening belts to extend runway. There’s some of that in the short term.
In the long term, I don’t see it having major, major impact. Any time we have a cycle like this, in some ways, it’s pretty natural. It will impact some more than others. We are watching it closely, but overall impact to us hasn’t been significant. We have it pretty balanced. We support SMBs all the way up to the Fortune 5.
As we all know, this story is also not done. It will be interesting to see how this unfolds over the next couple of quarters and year because there are tons of investment dollars available. It will be interesting to see when those investment dollars start to come back into the market. History can help us learn from other experiences, such as recessions, 2008, and the dotcom bubble bursting. It’s not totally uncharted, but we are paying attention to it pretty closely.
What will be important to the company over the next couple of years?
Most important for us is to continue to obsess about our customers. You heard me refer to them as builders. We are early days with the impact that builders are going to have in healthcare. It has never been more apparent to me that now is a great time to be a healthcare builder. We will continue to obsess about the people we support and continue to obsess about the use cases that we support. Doing that means we need to continue to power broader and broader sets of data to exchange.
We’ve broadened from being clinically focused to many types of data. Today, Redox is focused on data access and integration. As we look into 2023 and 2024, the interesting opportunity for us is to start to support more and more of that healthcare data journey on its path to ultimately being useful. We are working on some exciting things that you will start to hear from us later this year and early 2023. It will enable a whole other class of builders.
With all the craziness going on in the world right now, there has never been a better time than right now to be a health tech entrepreneur. Now more than ever, healthcare as an industry is primed for change. My closing statement is to all of the builders out there. Don’t wait on the sidelines. Come on, let’s do it. There’s plenty of work and plenty of opportunity for impact.
















































Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…