Curbside Consult with Dr. Jayne 3/2/15

I received an email from ONC on Thursday that they were extending the deadline for nominations to the HIMSS Interoperability Showcase, citing “feedback that organizations needed more time to submit nominations for participation.” From the time the email arrived, that’s a whopping three business days until the deadline. It made me wonder exactly why the deadline was extended and what their current applicant pool looks like. If they were delaying because they didn’t have many applicants, then they hardly gave much of a window for organizations that weren’t already prepared. Was the announcement a way to raise awareness about the Showcase rather than being designed truly to solicit participants?
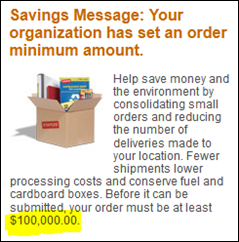
Perhaps organizations didn’t apply because they didn’t want to spend $8,000 to participate. That’s just for the kiosk at the Showcase, which includes a monitor, keyboard, mouse, power, and Internet connectivity as well as two exhibitor badges. Travel, meals, and lodging will be on top of that. We’re doing some cool things with interoperability at my health system, but they’re not about to spend upwards of $12K for developers to go show it off at HIMSS.
Whatever the reason, I can’t help but think about the ongoing list of government initiatives that have to be delayed, extended, or otherwise modified because they don’t seem to be achieving the desired results. Being a process improvement person, I’m always looking for the root cause when outcomes are not achieved or when projects run off the rails. Recently, we’ve had delays in ICD-10, Meaningful Use, and Healthcare.gov. Some of us, however, remember delays in the implementation of the 5010 claim standard and those of us deep in the weeds know about dozens of lesser-known parts of HIPAA and other omnibus legislation that are virtually unimplementable.
In medicine, we have a doctrine about ordering laboratory and diagnostic tests: don’t order it if it’s not going to change your plan for the patient. I do a lot of work with reporting from our EHR data and we have a similar dictum: don’t run the report if you’re not equipped to act on it. You’d think there would be a similar mantra about not making rules that people can’t actually follow, but that doesn’t seem to be a factor for those happily engaged in rulemaking. Only in healthcare do we come up with creatures like the “Two Midnight” rule and other similar nonsense.
My extended family is always asking about some of the wacky things that go on, such as provider-based billing, which allows hospital-owned practices to charge both a professional fee and a facility fee for outpatient visits. I’ve become as expert at explaining the Medicare Part D “donut hole” as I am at teaching patients to use a home blood glucose monitor. In trying to find some method to the madness, I stumbled on an article that attempts to explain why healthcare regulation is so complex. The first paragraph opens with a perfect summary: “Health care professionals may feel that they spend more time complying with the rules that direct their work than actually doing the work itself.”
The author contends that “regulation arises largely from a set of confrontations between opposing interests that created the system.” I agree that there are clashing agendas and learned that first hand as a young physician when the hospital’s chief of staff wanted to know why he wasn’t getting my referrals. It felt more than a little like a shakedown. He wasn’t aware that I sent nearly all of my referrals in his specialty to one of his partners, so at least his practice was seeing volume if he wasn’t personally. It didn’t matter, though, since it was apparently all about his ego. These conflicting agendas are ongoing, and “Doctored: The Disillusionment of an American Physician” talks about one physician’s struggle.
Although there are certainly turf wars at play, the regulatory soup includes rulemaking at so many levels that it’s nearly impossible to keep track of what needs to be done. I have to follow the rules of multiple hospital medical staff organizations, two state licensing boards, two specialty certification boards, one professional society, dozens of payers, the city, the county, the state, and the federal government. These rules (and non-rules that often have the force of law) sometimes conflict each other and often fail to make sense.
Several times in the last few decades, studies have looked at everything a primary care physician should be doing for his or her patients and how long that would take. An article in the Washington Post summarized the most recent data from the Annals of Family Medicine, which found that for a typical panel of 2,300 patients, the physician would have to spend nearly 22 hours a day to provide all the recommended care. That’s just delivering the care itself – it doesn’t factor in the time needed to comply with everything else a physician does such as arguing with payers, managing staff, dealing with regulations, worrying about compliance with programs, and trying to stay current with medical knowledge.
That’s what we’re dealing with in the ambulatory setting. Hospitals and health systems deal with many more rules and countless regulatory bodies. Similarly their IT departments are trying to keep the systems up and running, prevent breaches, avoid breaking something that’s required for Meaningful Use, and so on. It’s no surprise that people are not coming out of the woodwork to sign up for the Interoperability Showcase.
What regulations keep you hamster wheel spinning? Email me.

Email Dr. Jayne. ![]()

















Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…