
Jayne Goes to the Hospital
I’ve enjoyed reading the posts this week from our patient advocate HIMSS attendees. They all have interesting stories to tell from the patient perspective.
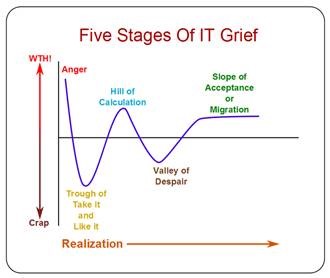
Recently I took off my doctor coat and became a patient advocate as I accompanied a coworker through her knee reconstruction process. Although she didn’t have it done at my hospital, she had it done at one that is part of a large multi-state health system that advertises its relentless focus on quality. It was eye-opening to see behind the curtain at someone else’s facility and to look at what goes on in a typical patient’s experience.
Her journey started after an ill-fated adventure vacation when she called me for an orthopedic recommendation. Since we work together, I asked why she didn’t go with one of the surgeons we know well. Her answer – privacy concerns – didn’t surprise me. She was able to get an appointment the day after returning home and was immediately scheduled for an MRI. Unfortunately, her surgeon’s office didn’t tell her she needed to schedule an appointment to receive the results, so she ended up calling a couple of days after the MRI only to be told she’d have to come in the following week.
That’s the kind of patient aggravation that’s totally avoidable. I had previously referred hundreds of patients to this particular practice as a primary care doc and never had that kind of complaint before. I did some digging with colleagues, and it turns out the practice was recently acquired by a health system that requires them to use a centralized scheduling service. Apparently the ball gets dropped a lot. It didn’t make me confident since I had referred her, but at that point, what can you do?
After receiving her results, she was scheduled for surgery at a hospital across town. I asked her why she selected it since the surgeon operates at multiple places. Her response this time did surprise me: that’s the first choice they gave her and she really didn’t consider other options. It just goes to show that no matter how much we think patients agonize over quality scores and other factors, sometimes they really don’t care.
Since she’s single, she asked if I would go with her and stay at her place the night after the procedure until she was sure she could get around the house. I agreed and we spent the night before sharing a bottle of wine and laughing about being young, sassy, and having your own personal notarized advance directive. After years of hospital work, she said she wasn’t crossing the threshold without it.
As we were leaving the house the next morning, the hospital called asking if she could come any earlier. Not likely since her scheduled arrival time was in 25 minutes and the hospital was 20 minutes away. It kind of surprised me that they’d bother calling patients to come early if it was likely that they’d already be on their way. That should have been a harbinger of the adventures we were about to have.
We arrived on time, only to find the parking lot where she was told we should park to be marked with “no surgery center parking” signs. Twice around the block and several one-way streets later, we made it to a parking garage.
The surgery center lobby was vacant except for patients and a sign-in kiosk. She registered and it took more than 15 minutes for anyone to call her up. So much for the need to arrive early!
The first question she was asked was whether she had traveled to West Africa in the last 21 days. The second was whether she was ready to pay her estimated patient portion in advance since she’d get a discount if she paid pre-op. Once her credit card was swiped, she was handed a laminated HIPAA and consent document (which had to be 8-point font) and told to “sign the signature pad when you’re ready.” There’s no way patients who are already nervous about a surgery are going to actually sit there and read it. I wonder if it would even hold up under legal scrutiny given the way it was presented.
By this point, I was totally taking notes on my phone since I knew a blog entry was likely to come out of this. The registrar asked if I’d like to receive text updates during the surgery, which I thought would be interesting to see how it worked.
With the paperwork done, we headed back to the outpatient surgery holding area. After being specifically told to keep her undergarments on (a fact which will become pertinent later, I promise), she changed into her low-fashion hospital gown and revealed the fact that she had marked her opposite knee with “NO!!!” in Sharpie. The nurse immediately jumped on this and belittled her, saying that she shouldn’t have done that because it would be confusing to the OR staff. Making a patient feel bad because they have a genuine (although humorously stated) concern about the risks of wrong-site surgery should never happen. She finished the intake process (after asking again about West Africa but never about the advance directive) and scurried off.
Luckily the anesthesiologist was a little more sensitive, kindly explaining that they have never had a wrong-site case at the facility and describing the multi-step process that they have in place to prevent it. The surgeon would meet with the patient, review the consent, sign the correct knee with “YES” and his initials, and this would be witnessed by patient and staff before the patient received any medications. They would repeat the process once the patient was anesthetized and before the surgeon started the procedure.
He was reassuring, but also stated we’d need to remove the “NO!!!” so it wouldn’t confuse the OR team. She agreed, but I wondered if the OR team couldn’t tell the difference between YES/initials and NO!!! that there might not be other issues at play.
We joked about the buffalo plaid sheets on the outpatient surgery gurneys. Our hospital has plain white, so we were snapping pictures. A second nurse came in and asked if the first nurse had finished the intake process. Um, I don’t know, since I don’t know what your intake process is. Wasn’t it in the chart? Apparently it wasn’t.
The second nurse finally logged in to see what had been charted, then proceeded to ask my friend specifically what the first nurse had done: Did she listen to your lungs? Did she use lidocaine when she started the IV? I pasted my best quizzical look on my face to see if she’d notice, but she was too busy charting another professional’s work to pick up on it. After copious clicking had gone on, the first nurse returned, asking “Oh, are you doing my charting?” and the second nurse admitted to it. I wonder what values she charted and whose login was used?
Shortly after that, the OR holding area called for my friend, so they got ready to wheel her off. The problem was the surgeon hadn’t come by yet. The nurses also realized they hadn’t completed some of the pre-op orders, but didn’t want to mess up the schedule, so off they went. I was given the option of carrying her bag of clothing with me or putting it in a locker – of course I chose the locker. I walked with her to the doors of the OR holding area and crossed my fingers that they would write on the correct knee.
The hospital has the same waiting room for the inpatient and outpatient surgery areas, but there was no one at the desk. I selected a seat close to an electrical outlet and started catching up on some work. A few minutes later, I received a text that she was “now in the operating room.” A few minutes after that, a staffer in scrubs and a cover gown arrived and asked for the “Jane Doe Family” and I raised my hand. She walked over and handed me a clear Ziploc bag stating “she forgot to take off her underpants” in a loud stage whisper. Luckily the rest of the room couldn’t hear her over the Shark vacuum infomercial that was playing on the communal TV, but I know my friend would have been horrified.
As she left, a hospital volunteer arrived to staff the desk and explained the monitor they have on the wall that shows the patients’ initials and a color-coded bar that says where they are in the grand scheme of things – pre-op, OR, procedure in progress, procedure complete, recovery, post-op, etc. I liked the idea and I liked even better the family member that interrupted, asking for the remote control. They found an episode of “Gunsmoke,” which was much more appropriate for this particular waiting room demographic.
I received a “procedure has started” text and set my timer so I could plan the rest of my afternoon. I was able to accomplish a massive email cleanup with very few distractions from Marshal Matt Dillon, then took a break for lunch.
The cafeteria was chock full of motivational posters for staff as well as banners celebrating their “Top 10 Hospital” recognition from an organization I had never heard of. Regardless, it was nicer than my own hospital and the food was better, so I gave the experience a 10 myself. I continued to receive “the procedure is still in progress” texts every hour or so. Once I returned to the waiting room, I also received hourly updates from the waiting room volunteer who actually said, “She’s still in surgery – whoop de do, I know” at least twice. It has to be boring saying the same thing all day and she was sweet, but nevertheless I doubt the hospital would appreciate it.
Once I received the “patient is now in recovery” text, I found a good stopping point and packed up my laptop. The surgeon came out (wearing rubber rain galoshes with his scrubs, which was a new one for me) and went through her surgical photos with me. I have to say, the innards of her knee looked pretty ragged in the “before” photos and much more glamorous in the “after” shots. He told me she’d be “going home on crutches” and that he’d leave a script for pain medication.
I knew he was straight out of fellowship, but he looked even younger than expected. Despite feeling old, I figured that being proficient in the latest and greatest techniques outweighed any concerns about duration of practice – I wasn’t even aware the procedure she was having existed before she told me about it.
The volunteer stepped away and asked that someone answer the phone if it rang. It did, and I was told to “go back to the outpatient holding area.” I went back to the outpatient surgery lobby and it was closed with a sign directing me to the front desk. I figured going to the front desk would be more hassle than finding my way to the holding area, and made it there after only two wrong turns. My friend was in a holding bay and awake, so I stepped to the bedside and immediately received a look of annoyance from the nurse. “She just got here. We’re not ready for you yet.” I apologized and told her that I had been instructed to come up and backed away. They didn’t tell me where to go, so I just stood there feeling stupid.
Once I was allowed back at the bedside, my friend was still pretty doped up. The staff offered the ubiquitous eight-ounce can of Sierra Mist and her choice of Cheez-Its or pretzels. Another nurse yelled, “We’ve been out of Cheez-Its for months,” which set the stage for our tour through the post-op process. The staff printed her discharge instructions and went through them with me, explaining that she had received two nerve blocks in her leg and they would last for at least 18 to 24 hours. That was news to both of us! I started wondering how I was going to get her out of the car and into the house since managing stairs, a tall lanky athlete, and a dead leg might be quite the trick.
As we went through the instructions, we found several conflicts on dressing changes and showering. I had questioned the “leave dressing on until showering” and “shower after seven days,” which resulted in a call to the OR to clarify with the surgeon, who had started his next case. Next was a search for the prescription, which the nurses assumed I had been given in the waiting room. A call to the OR revealed the surgeon had taken it with him. Last, there were no instructions for how often and how long to use the high-tech ice water therapy machine he had ordered for her (which incidentally insurance didn’t cover, but we have enough mutual friends with sports injuries to scrape one up from someone with better coverage). Yet another call to the OR. I can only hope that as a young surgeon, he’ll learn to double check things or develop a process, because three calls to the OR to clarify orders is too many. On the other hand, maybe his hospital’s $200 million EHR might have an order set?
Since she had been drinking fluids, eating solids, and not feeling nauseated, the nurses announced she could get dressed and go home. That was when my radar went up. In my post-op universe on the other side of town, we want to have a patient complete some critical functions (such as emptying the bladder) after they’ve had general anesthesia and a bladder catheter. I didn’t consider three pretzel sticks to be “eating solids” and my friend was still pretty dopey, not to mention completely unable to move or even feel her leg. I asked about the crutches since the surgeon said she’d be going home on crutches and they said he didn’t order any. I gave the quizzical look again and she said that even if they had an order, they couldn’t dispense them because it was after 4:30 p.m. and the physical therapists had gone home, so no one could do crutch training. Then she added that I could rent them at the pharmacy if I wanted them.
I reminded the nurse that my friend had zero control of her leg and I had no idea how I was going to get her out of the car and into the house. What did they suggest? Another nurse chimed in and said, “I don’t think crutches are a good idea anyway. They’re not stable. She really needs a walker.” I asked if we had an order for that. She said no, but they had a walker she could try. I suggested that maybe we try the walker on the way to the bathroom since she hadn’t been yet.
She barely made it the 20 feet to the bathroom since her toes were dragging and she had to lift the leg from the hip to get it to swing through as she advanced the walker. I couldn’t believe that as a facility that does this every day, they had no plan for this. I guess maybe all the other patients bring their own crutches or walker. I took the opportunity while she was in the bathroom to start calling septuagenarian relatives who have had knee replacements to see if anyone had a walker I could pick up on the way home. I was grateful for success on the first attempt.
While she was in the bathroom, she figured out that she was missing some clothing she had been wearing pre-op. She asked where it was and was not amused by my answer that they brought them to me in the waiting room. I dug them out of my laptop bag while we strategized on getting her dressed. She wasn’t keen on having the nurses assist, so I helped her wrestle the dead leg (with its huge bulky dressing and rigid brace) into her clothes. While the bay curtain was closed, we overheard the nurses buzzing around since someone had taken their specialty wheelchair that is set up for a patient with their leg locked in an extended position. One never wants to hear, “We’ll just have to rig something” when you’re being discharged from the hospital.
Being out of the hospital gown (and also free of mind-fuzzing medications) must have been empowering because my friend started to let the staff know how much she was not amused by the discharge process, the multiple order conflicts and omissions, and the apparent lack of a plan for what is likely a common set of events. A supervisor stepped in and I slipped away to get the car, knowing she could handle herself. I pulled into the circular drive as instructed and discovered it was full of cars left for the valet but not addressed. I had to double-park in the traffic lane and go back in, where I found the nursing supervisor offering her best service recovery tactic. It involved (no kidding) a “XYZ Hospital” mug with a can of soup, tied up with cellophane and a bow. I actually laughed out loud at this point.
Soup in hand, our patient announced she was ready to go and the supervisor wheeled her out, taking a route which required me to manually open two doors on the way so she could wheel the patient through. I guess there is no way to take a patient out in a wheelchair that either uses automatic doors or assumes the family will be there to open them. What if I was out waiting with the car? It’s a small thing, but if there’s anything that the events of the day proved, the small things count.
Our patient immediately became nauseated upon trying to get into the car, resulting in a frantic run by the nurse. Luckily we avoided any actual vomiting, but I guess it’s something the family should be ready to handle.
We headed into the sunset to pick up the walker, drop off the prescriptions (couldn’t she have been given the script at the pre-op appointment when she scheduled the surgery?) and wrestle the dead leg into the house. Luckily she’s an athlete and was able to do some kind of parallel bars lift and twist maneuver to handle the steps, but I worried about her banging the dead leg around. She made it to the sofa and we fired up the ice therapy machine. I ran out to pick up her prescriptions and provisions. Three bags of ice, 90 Percocet, two Red Box flicks, and a medium pizza later, we were stocked.
The night passed uneventfully, although I couldn’t resist snapping photos of her wearing compression stockings with her walker. Some day when we’re of “Golden Girls” age, we’ll look back and have a lot of laughs. The dead leg started waking up after 8 a.m. the next morning but it was more than 24 hours before she could really move it. I violated the post-op orders and changed her dressing the next day since they had three battlefield dressings on there. It was so thick I didn’t think the ice therapy was making it anywhere near her knee. and once she was no longer numb, it was confirmed.
After two days. she ditched the walker for crutches (borrowed from the high school basketball player up the street) and started physical therapy a few days after that. Her overall prognosis looks great and I have successfully resisted the urge to ask her if I can examine what has got to be a seriously rock solid knee. It will be a while before she’s wearing stilettos again, although if there’s anyone who could manage them on crutches it would be her.
I still wonder though what other people do in these situations. Do they really leave a grapefruit-sized dressing on for seven days? Or do they just call the office? Do they bring their own crutches to surgery? Do they know to ask for the post-op prescriptions in advance? Do they know to bring something for possible carsickness? Are they savvy enough to take off all their clothes even when told to leave some of them on?
I wasn’t the patient, but for a healthcare system that increasingly demands quality, the whole process was certainly something. The next time I am asked to review post-op order sets or pre-op protocols, I’m going to look at them with a new perspective.
What’s your patient-side story? Email me.

Email Dr. Jayne.















Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…