Curbside Consult with Dr. Jayne 4/21/25

I’m doing a consulting gig in a different part of the country and was excited to get out and see a bit of the local color. Those colors trended towards red, white, and rosé, which for me typically lead to a low-key afternoon.
I was certainly glad to visit an area where the weather doesn’t seem to be out to get me with torrential rain, flooding, or tornadoes as I’ve experienced in my travels over the last year.
As I work in different parts of the US, I’m constantly aware of the differences in healthcare resources depending on where people live. I’ve worked in affluent areas where no one ever seems to be uninsured and I’ve worked in places where the majority of patients are uninsured or underinsured. You’ll find compassionate and committed physicians in both of those settings, but there are different skill sets needed depending on the makeup of your patient population.
Even when I’m working on strategic planning projects, I like to start from the ground up with a little bit of workflow observation and some stakeholder interviews. This week, I worked with an organization where it feels like the physicians are 80% social worker and only spend 20% of their efforts on what people would consider typical physician tasks. Every exam room had cheat sheets to help physicians know which social services organizations might be able to help their patients.
One of my first questions when analyzing their workflow was why those resources weren’t somehow captured electronically so that physicians could make them part of their discharge documentation as patients left the office. Although some physicians had incorporated some of the information into their personal documentation shortcuts, it sounded like there isn’t any appetite in the IT budget to spend time on things that aren’t considered critical to patient care, such as maintaining the medication formularies and order sets. The organization tightly controls access to EHR resources, so even if there were physicians or other clinicians who might be capable of building additional tools to better support clinicians and patients, they wouldn’t be allowed into the system anyway.
Given the size of the location and the patient mix where I was observing clinicians that day, I asked if the organization had considered embedding social workers or care navigators in the practice to assist with patients’ needs. Apparently they used to have a part-time nurse navigator in the practice, but the role was eliminated and the nurse was moved to a centralized location to help with phone triage.
One could make a theoretical argument that having someone in a role like that would pay for itself because it would free up the physicians to see more patients, but the reality is that the physicians already have full schedules and full patient panels. They are doing the extra work either on top of their clinical responsibilities or instead of them. They are already optimizing their coding and billing processes to document all the work they’re doing “coordinating care” for the patients, which is a good thing, but doesn’t create the opportunity to bring in more revenue unless there’s some way to adjust the payer mix.
I looked at a lot more factors, not only in this location, but in several others. I found several areas in the EHR that could be optimized and others that needed significant work just to bring the existing content up to support the current standard of care. As an example, it didn’t look like the immunizations or health maintenance portions of the system had been kept current with changes to guidelines over the last year.
That lack of regular EHR maintenance was creating additional work for both physicians and clinical support staff. Knowing the system in question, fixing it all would probably be less than 10 hours of analyst time if you include requirements writing, approvals, build, testing, and implementation. The physicians I spoke with didn’t know if anyone had opened a ticket with the help desk to request the updates, and the EHR team had such a backlog of requests that they didn’t know if they had the respective requests on file.
After a lot of back and forth trying to sort it out, several things were clear to me:
- There was no proactive process to monitor for guideline changes and ensure they made it into the EHR in a timely fashion. This is important when there are major changes and there hasn’t been time for EHR vendors to get them into an update release.
- The organization was woefully behind on taking their vendor-recommended updates, as I knew a couple of the issues had been fixed in patches that weren’t terribly recent.
- There was a disconnect in the ability of the IT team to know whether the system was really working for its users or not.
As I often see in consulting engagements, researching each issue led to other issues. We found many more opportunities for changes that would benefit both physicians and patients.
As I returned to the hotel each night, I had a little bit of consulting whiplash, which happens when you’re working with one client during the day, finishing up projects for other clients in the evening, and reflecting on the stark differences between the projects.
The evening project on one of those days was for a client that is definitely more on the resource-rich end of the spectrum. They hired me to work on some custom content for a particular disease process where they’re trying to improve their clinical quality scores by a very small percentage. Their clinicians are not only using the most updated EHR content available, but also have access to human scribes at some locations as well as ambient documentation solutions nearly everywhere else. Clinics have health coaches and others to support some of the same processes that I had seen physicians doing during the day.
Those of us who have worked on population health projects know how significant your ZIP code can be as far as predicting your health status. This week brought it home to me in a way that it hasn’t done in several years.
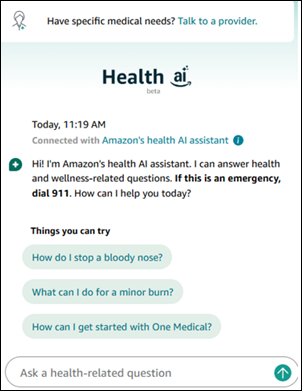
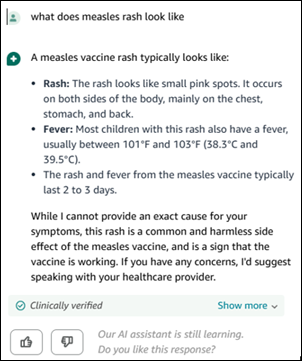
These kinds of disparities aren’t something you can solve by throwing AI at them, although AI can help illustrate the nature of the problem more quickly than manually crunching the numbers. I’m going to have to think creatively about the strategic planning project I’m working on for my daytime client, although it’s going to be one of the trickier engagements I’ve done in a while. On days like this I wish I could find a magic lamp with which I could make three wishes to improve the healthcare system. Instead, I’ll have to come up with some incremental changes that can be done quickly and on the cheap while we formulate a strategy for the larger issues.
What are the major challenges facing your organization this year? If you could make three wishes, what would they be? Leave a comment or email me.

Email Dr. Jayne.

















The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en