EPtalk by Dr. Jayne 6/13/24
I get a lot of emails advertising webinars and educational opportunities. I don’t usually take advantage of them because my schedule is busy and the invites don’t arrive with enough notice to allow me to attend. However, a recent email from one of our local HIMSS chapter sponsors caught my eye.
It met all the criteria. I received it several weeks in advance, the topic was interesting, and it was advertised specifically as an educational session. I blocked my calendar and registered. I logged in well in advance, only to find a blank screen and no indication that I was receiving the audio or video feed. I appreciate a moderator who addresses attendees with some kind of “Thank you for joining, the session will begin in three minutes” kind of welcome so that you know you’re in the right place and everything is working.
It was well after the top of the hour and the webinar hadn’t popped up yet, so I refreshed the window and discovered that it had already started and I had missed the intros. It also was less of a formal education session than talking heads, with no agenda or educational objectives. I had yet to hear anything about healthcare IT in the first 20 minutes (although I did hear a lot about AI being used to predict the likelihood of a criminal reoffending and about autonomous vehicles), so I gave up.
If you’re putting on a webinar, here are my recommendations. Advertise your offering accurately. If it’s not going to be a formal educational session, don’t make it sound like one. Words like “chat” or “roundtable” indicate a less-formal presentation. Also, know how your platform works. If it won’t automatically refresh for early-arriving attendees, add a chat message to advise them to refresh the screen regularly so they don’t miss anything.
Anyone who has ever been in a clinical role in a hospital is used to hearing “The Joint Commission requires it” about policies that may or may not be subject to Joint Commission review. The Joint Commission recently released an update that clarifies its position on using secure texting for patient information and orders. Organizations can use that modality for orders as long as the information is secure, encrypted, and captured in the EHR with timestamps and author information. This brings The Joint Commission into line with CMS policies, although having providers enter orders directly into the EHR remains the best practice for order entry.
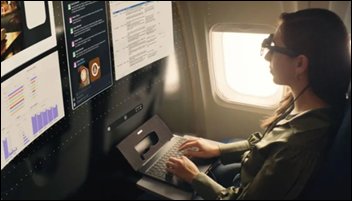
A friend clued me in to Spacetop, an augmented reality laptop that is under development and is available for reservation. Along with “the first spatial OS designed for productivity,” the G1 model is priced at $1,900 and will start shipping in October. Prescription lenses for the retro-looking glasses are included, although I would be more impressed if it included technology where the user could input the details of their eyeglasses prescription and have the system adjust the visuals automatically. It advertises a 100-inch visual canvas with a form factor that “fits a standard laptop bag with the glasses safely stored in hardcover.” The glasses include speakers and microphone for use during online meetings, although unless I’m interacting with a bunch of users with the same device, I think that would seem a little strange. If the company is looking for beta testers, I know a sassy CMIO who would love to give feedback.
From LaSalle Gal: “Re: MyChart. My health system sent me an email recommending that I turn on all the notification settings. Although it had technical instructions for toggling the notifications on, it seemed like a missed opportunity to educate patients on what it means to receive notifications, especially for patients who may not want to see test results before they receive a communication from their physician.” I reviewed the original email and I agree. It would have been easy to insert a sentence or two about how the organization releases results along with instructions for suppressing notifications that you don’t want to receive. I also thought this section was funny: “Even if a toggle is already green, you might not have all notifications turned on. To make sure all notifications are enabled, just switch each toggle off and then back on.” That doesn’t instill confidence to this user that the settings are accurate and functional. I’d be curious to see data about how many patients may have accessed the communication preferences settings in the weeks after this communication was sent.
Based on my comments about certain clinicians struggling with handwritten orders during downtime events, another reader sent this piece from NPR’s “Shots” blog that addresses the benefits of writing by hand. It summarizes some of the benefits of handwritten work, including better letter recognition in children and better conceptual understanding of material when adults take notes by hand. I own a set of amazing medical student notebooks from the 1920s (thanks, eBay!). It’s interesting to imagine the student sitting there, jotting his thoughts about the fact that “we are really just starting to understand the mysteries of the thyroid.”
Pet peeve of the week: the phrase “building an organizational muscle.” At best, it makes me think of bodybuilders oiled for competition, and at worst it reminds me of an old drug company ad for a diabetes medication that anthropomorphic characters such as Hungry Muscle, Burned-Out Pancreas, and Upset Stomach. (Side note: in trying to remember what the drug was, I discovered that you can buy the Hungry Muscle plushies online, so I know I didn’t imagine it. I also learned that there is a thing called the Medical Advertising Hall of Fame.) Whether you’re building an organizational muscle for change, for quality, or some other buzzword, there are better terms: “a culture of change” or “a commitment to quality” come to mind.
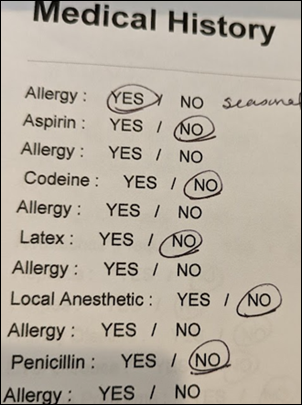
I spent part of the morning being a patient at my local health system. For the most part, the information I provided during the online check-in process was used, including an update to my health history and a review of systems. They required a new scan of my insurance card, however, even though I’ve had another appointment within the last 30 days and the card was scanned then. The receptionist also asked me the standardized COVID exposure questions that were appropriate several years ago, including whether I had any international travel within the last year or the last 30 days. I’m not aware of any recommendations for travel screenings in healthcare environments, so it felt like an organization that just isn’t staying current. It made me wonder how often the organization is reviewing its patient experience, as well as its ability to keep current with infectious disease recommendations.
How often do you reassess your patient registration and check-in processes? Leave a comment or email me.

Email Dr. Jayne.




















The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en