I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…
News 11/16/18
Top News
Pointed fingers fly at a House Veterans’ Affairs EHR subcommittee meeting, with most aiming towards VA program director John Windom once he let it be known an additional $350 million in personnel costs would be part of the Cerner project’s already $16 billion budget.
Windom attributed the hiring costs (part of the “fuzzy math” some committee members have complained about) to EHRM office downsizing and the need to have “highly qualified subject matter experts to grade the implementation efforts of Cerner. Those people cost money.”
Other items of interest from the oversight meeting:
- Computers – most of them at least five years old – will be replaced six months ahead of the Cerner implementation at most VA facilities.
- The DoD and VA will use the same web address to access the online system.
- The agencies will share a patient identity management system.
- Progress checks should be made every 90 days over the life of the 10-year project, a recommendation in line with Cerner President of Government Services Travis Dalton’s promise that the VA project won’t suffer from a lack of frequent engagement with implementation sites – a problem that has plagued initial DoD sites in the Pacific Northwest.
- Leadership over the joint DoD-VA project is still in doubt. VA Secretary Robert Wilkie has said he will take the lead, while Windom told the committee that acting Deputy VA Secretary Jim Byrne is in charge.
Reader Comments
From Ginsu Sharpener: “Re: CommonWell. Launching a search for a technology vendor.” The company will issue an RFP in December 2018 for “interoperability infrastructure and services.” I assume these are the services that RelayHealth has provided since CommonWell’s founding in 2013. They’ will explain more in the RFP Bidder Call on Friday, November 16 at 4:00 p.m ET.
From Watcher: “Re: ONC proposed rule from Tuesday. #3 supports a safe harbor for care coordination, which would significantly benefit social determinant and social care workflows.” HHS OCR issues an RFI to solicit the public’s views on whether HIPAA rules prevent or discourage providers, payors, and patients from sharing information for care coordination and case management. One item specifically addresses creating a safe harbor for good-faith PHI disclosure for coordinating or managing care. The change is being considered under HHS’s “Regulatory Sprint to Coordinated Care,” which hopes to remove regulatory barriers that impede coordinated, value-based care.
From Hanzi: “Re: Centra Health. Blames its Cerner implementation for its loss.” The health systems nine-month report says Cerner went live on September 1, increasing staffing costs while reducing clinic volumes. It spent $65 million on Phase I. Year-over-year operating income dropped from a $18.8 million to –$2.7 million.
From Curved Air: “Re: 3M. We were notified that one of their administrator accounts was compromised. We’re in the midst of our investigation. I figured it’s the same issue as the anonymous report you posted early.” That is correct. Two C-level readers say they received a communication from the company, but haven’t seen public reports otherwise.
HIStalk Announcements and Requests
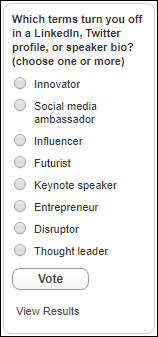
I’ll report the results of this poll over the weekend, so it’s last call to vote (exit polls suggest a possible upset in that “disruptor” is even more loathed as a self-assigned adjective than “thought leader.”)
Webinars
December 6 (Thursday) 11 ET. “Make the Most of Azure DevOps in Healthcare.” Sponsor: CitiusTech. Presenter: Harshal Sawant, practice lead for DevOps and mobile, CitiusTech. Enterprise IT teams are moving from large-scale, project-based system implementations to a continuously evolving and collaborative process that includes both development and business teams. This webinar will review healthcare DevOps trends and customer stories, describe key factors in implementing a DevOps practice, describe how to assess Azure DevOps, and lay out the steps needed to create an Azure DevOps execution plan.
Previous webinars are on our YouTube channel. Contact Lorre for information.
Acquisitions, Funding, Business, and Stock
In the UK, RenalytixAI raises $29 million in an IPO that will be used to fund the launch of AI-enabled applications for the early detection of kidney disease and transplant management. The company was spun out of Mount Sinai Health System’s New York-based commercialization arm, and will use de-identified data from the health system’s Epic EHR in its product development.
Allscripts rebrands its Payer & Life Sciences Division to the far more confusing moniker of Veradigm, offering clinical workflow, research, and analytics software and services to providers, payers, and health IT and life sciences companies.
People

Loyale Healthcare names Timothy Sykes (Regroup) as VP of sales.


Health Catalyst appoints Jason Jones (Kaiser Permanente) chief data scientist and Elia Stupka (Dana-Farber Cancer Institute) chief analytics officer / SVP of life science.
Sales
- Dartmouth-Hitchcock Health (NH) will use technology from Philips to develop a tele-ICU program at Dartmouth-Hitchcock Medical Center and Cheshire Medical Center.
Announcements and Implementations

Casenet announces GA of its TruCare 7.0 population health management software, including chronic care guidelines from MCG Health.
Wake Forest Baptist Health (NC) implements tele-ICU services from Advanced ICU Care at three hospitals.
LogicStream Health releases a drug shortage app to help hospital pharmacies identify and manage drug shortages, noting that manual process require up to 10 hours to evaluate each shortage as organizations experience 3-4 per week, basically a full-time pharmacy department position.
A new KLAS report on healthcare management consulting finds that health systems are seeking help with value-based care transformation (top choices: Premier, Optum / Advisory Board, McKinsey); financial improvement (Huron, Deloitte, Navigant); strategy (McKinsey, The Chartis Group, Deloitte); and consumer experience (Press Ganey, Huron, Optum / Advisory Board). The high-mindshare, cross-industry firms are Deloitte, McKinsey, and Huron, although KLAS notes that McKinsey and Huron are also the two lowest-performing firms.
Surescripts announces that its Real-Time Prescription Benefit tool, launched last year, has increased prescriber count 40-fold and has been used 30 million times within EHRs to look up patient-specific drug price and alternative information. CVS Health says prescribers switch non-formulary prescriptions 75 percent of the time and higher-cost meds 40 percent of the time, saving patients an average of $130 per prescription.
Other
A New York Times analysis of hospital mergers in 25 markets reveals what most of us already know from Econ 101 – less competition has resulted in higher prices, despite hospital PR efforts touting the contrary. Admission prices have gone up between 11 and 54 percent in the years following mergers in the analyzed areas; they tick up even further once acquired physician groups are taken into account. The cost of replacing or integrating the health IT systems of acquired organizations isn’t mentioned as part of the price increases, but I’m willing to bet it has a strong downstream effect on patient pocketbooks.
The New York Times also looks at the incredible wealth made by the family-related owners of Wall Street-backed private hospital chains in China that control 8,000 facilities, 80 percent of the private hospital total. The hospitals, overseen mostly by overwhelmed local governments, have been caught fabricating patient testimonials, claiming 100 percent cure rates, falsifying doctor credentials, and using outdated or dangerous treatment protocols. The original founder made his money selling a homemade remedy for scabies door to door, overcoming his lack of medical background in recognizing that the country’s medical system was a mess. His company grew quickly as the government realized public hospitals could not handle a rapidly growing population.
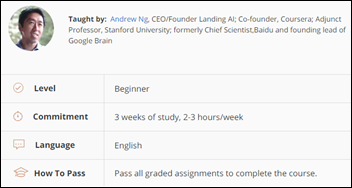
AI celebrity Andrew Ng launches a Coursera program aimed at non-technical business leaders called “AI For Everyone.” The three-week course requires 2-3 hours of work per week and opens in early 2019.
Sponsor Updates
- EClinicalWorks will exhibit at the Annual Pain Care for Primary Care event November 16-17 in Bayside, San Diego.
- Healthfinch launches the first of a four-part e-book series, “Introduction to Prescription Refills Requests.”
- IDC MarketScape names Lightbeam Health Solutions a leader in its US Population Health 2018 Vendor Assessment.
- Visage Imaging will preview its new Visage 7 technology with AI capabilities at RSNA November 25-29 in Chicago.
- Surescripts reports a fortyfold increase in adoption of its Real-Time Prescription Benefit tool since it launched last year.
- Meditech publishes a new case study, “Union Hospital’s Journey To Stage 7.”
- Nordic releases a new podcast, “Expert advice on preparing your MSSP submission.”
Blog Posts
- Physician Burnout – the EClinicalWorks Solution (EClinicalWorks)
- Time to Change the Conversation: Take the Next Step Forward in Revenue Integrity (Hayes Management Consulting)
- Should you implement a true enterprise imaging strategy? (Hyland)
- Keeping up with Meditech Expanse (Iatric Systems)
- QPP Final Rule for 2019: Overview (Impact Advisors)
- California Consumer Privacy Act: How will it impact healthcare? (Imprivata)
- Hyper-Local Growth Strategies for Profitable Service Lines (Influence Health)
- 4 Keys to Keep Your RFP Process as Painless as Possible (Spok)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates. Send news or rumors.
Contact us.








I thought Travis Dalton did a good job not insulting our intelligence and not lying… “hard lessons,” “should have done it differently.”
On the other hand … Lawmakers balk at $350 million. Really? They have a $20 billion system (MHS+) that has been live for almost two years and doesn’t work. $350 million is just such a tiny sliver of the cost that a broken enterprise system imposes on a health system. The lost productivity of tens-of-thousands of physicians, nurses, therapists, and other users not only dwarfs the $350 billion, it dwarfs the $20 BILLION.
Why is nobody in Congress demanding answers about Director Behler’s report which clearly recommended “delay further fielding”? There’s some bizarre assumption that these problems are in the past and these lessons are “learned.” A 33% improvement over terrible is still terrible. Someone, everyone, should be asking for an update on the state of the system TODAY.
Well the DoD just spent another $100M, now well over $6B, on an audit of its spending that was years overdue, failed abysmally, and has no timetable for when it will be able to produce a credible audit to Congress or other third-party entities.
Still the only federal agency which hasn’t conducted this audit since Congress mandated it in 1990 that all federal agencies conduct such as audit.
Even the DoD admits they can’t account for trillions in spending since 1998 and that doesn’t include black budget items estimated now annually at $60B.
No federal agency has anywhere the amount of theft, cost overruns, and out right waste that the DoD commits. It’s mind boggling.