Curbside Consult with Dr. Jayne 1/26/26

Significant portions of the US are experiencing arctic temperatures and significant snowfall this weekend. As the storm approached my area, I touched base with nursing staff at several hospitals to see how they were ensuring adequate staffing despite deteriorating road conditions.
They generally offered options for staff to sleep on campus, but approached the situation in drastically different ways. One hospital enticed nurses to sleep on campus to guarantee attendance, paid a retention bonus for the time between shifts, and provided meals Another sent a text message that was less than welcoming, treating those who planned to stay at the hospital as a burden by telling them to bring their own bed linens and towels. I’m betting that employee satisfaction differs between those facilities.
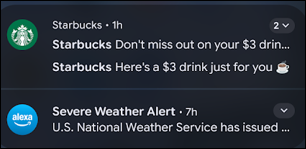
Speaking of things that didn’t resonate well during the storm, the marketing folks at Starbucks should reconsider their tactics during winter storms. While the National Weather Service was issuing advisories and our city and state public safety officials were urging people to stay off the roads, Starbucks was blowing up my phone with discount drink offers.
It seems like it would be easy to suppress those promotions in area codes where people shouldn’t be on the roads, whether they’re customers or employees. People who have storm-belt area codes might live elsewhere in the US, but I would guess that they are in the minority. Better yet, come up with a promo code that people can enable that becomes active in three or four days, when they start to tunnel out and are looking for a treat. My city is still focusing on clearing interstates and critical roads, so I will be staying put for a while.
We became skilled at pivoting to virtual meetings during the COVID pandemic, so I was surprised to see some meetings cancel off of my schedule even though they could have been held as web meetings or even as old-school conference calls. I could understand this for small organizations that might have let their virtual meeting subscriptions lapse, but these cancellations involve larger organizations that routinely have at least one or two people on video due to travel constraints.
Childcare issues could be at play due to school closures, but one of the only bright spots of the pandemic was getting to virtually meet the families and pets of my co-workers.
In last week’s Healthcare AI News, Mr. H mentioned the growing concerns that we are on the cusp of seeing AI-related malpractice lawsuits. Frankly, I’m surprised that we’re not already there, given how I see some of my colleagues using AI tools.
Quite a few knowledgeable clinicians, including clinical informaticists and AI researchers, understand the limits of AI. But large numbers of people are overly trusting of the content they see coming out of LLMs.
I’ve seen people cut and paste content containing obvious errors directly from a non-clinical AI tool into the EHR. I’ve also seen people operate wildly outside their scope of practice based on the ability to quickly access information that may or may not be accurate. Unfortunately, these are the situations where people don’t know what they don’t know, and LLMs can be extremely convincing even when they are wrong.
As an example, I recently saw a patient who was accompanied by a physician family member. The family member had a predetermined outcome that they wanted to achieve during the visit. They apparently thought that paying an $80 co-pay entitled them to see a physician who would suspend their professional knowledge and judgment and do the electronic equivalent of whipping out a prescription pad and ordering what they wanted.
I explained the clinical situation, the evidence-based recommendations, what I saw on the patient’s exam, what I had gathered from their history, and why I believed that the requested medication wasn’t appropriate in that scenario. The family member began arguing with me and was showing me his phone with his previous searches on the topic as a way to prove his point. Especially given that his specialty training wasn’t even close to the body system in question, he wasn’t aware that the articles being cited were only tangentially related to the diagnosis.
Fortunately, I’ve spent the last couple of decades working with patients who bring their internet research to the visit. I’m pretty good at educating while arriving at a plan of care that is mutually acceptable. However, I don’t have a lot of experience arguing with a peer who is putting blind trust in the output of a generative AI tool, so it was new territory.
I used my emergency department-mandated de-escalation training, so we managed to make it through the visit once one of the other family members in the room made the physician family member leave. With situations like this on the daily, it’s no wonder that clinicians have lost the joy in medicine. Having to argue with AI-generated errors when a patient’s health is at stake is something that none of us signed up for.
Mr. H also mentioned ECRI’s annual list of technology hazards, and I was gratified to see one of my soapbox issues in the number two position. “Unpreparedness for a ‘Digital Darkness’ Event” is a fancy way to say that an organization isn’t ready for an unplanned downtime. Maybe making it sound more exciting will convince people that they need to do something to get ready.
We should all know that cyberattacks are a “when” situation rather than an “if” these days, and that network or vendor outages are entirely possible. For clinicians who have always been dependent on the tools and safeguards that are built into the EHR, having to work without those can be frightening. It’s one thing to not have calculators or references at your disposal, but not being able to see the overall picture of what’s going on in the intensive care unit at full capacity is something else entirely.
Those of us who practiced in the olden days remember the large paper ICU progress notes that were the size of a poster board, but could fold up to fit in a standard medical chart. With just a glance, we could quickly figure out what was going on with a patient and formulate the best questions to ask during shift change.
The availability of electronic dashboards and monitoring suites has rewired those parts of my brain, but I bet that mental model is still in there somewhere and I could access it in a pinch. We need to remember that soon there will be more clinicians who have never seen that kind of paper documentation than those who have, and adjust our downtime preparations accordingly.
Are you prepared for a digital darkness event? Have you experienced any outages due to snowmageddon? Is your hospital treating staff who have to stay overnight in the facility like a blessing or a burden? Leave a comment or email me.

Email Dr. Jayne.


Healthcare data sucks - that song turned my Friday to Friyay!!! Gave me the much needed boost to get through…