Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…
Monday Morning Update 2/17/25
Top News

A JAMA commentary piece notes that patients don’t trust how health systems will use AI, but then again, they don’t trust health systems in general.
A cited study found a mean health system overall trust score of 5.23 on a 12-point scale. Only 40% of respondents expressed high trust, down from 72% pre-pandemic.
The author, Vanderbilt informatics professor Jessica Ancker, MD, MPH, recommends that health systems clearly disclose AI interactions, specify who can access AI-generated data, and inform patients when AI is used to influence clinical decisions.
She also notes that people tend to be wary of technology they haven’t personally experienced, such as self-driving cars, but usually warm up to it once they see it for themselves.
Reader Comments

From Peds MD: “Re: Epic’s Care Everywhere. Responding to the HIStalk post last fall where Care Everywhere failed to match a critical newborn, Epic relaxed its requirements to make matches if you have the patient’s Care Everywhere number (from the place you are querying) and two other matching demographics. Today we had a patient who had “some kind of heart surgery” as a child in 2001, and it was medically important to know exactly what was done. Because they had moved across the country, I couldn’t match the patient using regular demographics — everything had changed except their name, sex, and date of birth — but when I obtained and entered the Care Everywhere number from the other hospital’s HIM department, the match came back immediately. We are still working with Epic on improving matching, but I think it’s important to recognize progress, as it made a big difference in this patient’s care. Kudos to HIStalk for helping in this.” I posted the reader’s original problem description last year. Thanks for the update and thanks to Epic, which I can say always responds quickly and personally to address issues that readers have reported here.
From Silken: “Re: Epic and SaaS. I’ve seen online commentary about the benefit of Epic moving to SaaS model. What do you and your readers think?” For me, I see the possible customer advantages of running a SaaS versus on-premise and cloud-hosted products. However, technical punditry and wishful thinking aside, you have to assume that Epic is like all companies in being most likely to take whatever path benefits it most. Thoughts:
- Big, Epic-using health systems aren’t visibly demanding a SaaS model, at least when it comes to voting with their dollars, which is the only vote that counts. They have already invested in Epic-driven infrastructure, IT expertise, and long-term budgets. These are sunk costs that shouldn’t influence future decisions, but hospitals are generally risk-averse and don’t relish major disruptions like retraining and workflow changes, especially in the absence of a clear business benefit.
- Even though Epic’s maintenance costs are high, SaaS wouldn’t necessarily be cheaper over time since it’s still up to Epic to set prices.
- Many health systems already operate a de facto SaaS model by hosting Epic for affiliated hospitals and clinics. This may be more cost-effective than Epic offering SaaS directly to an ever-decreasing number of unaffiliated small hospitals and practices.
- SaaS benefits include scalability and faster onboarding of acquisitions, but drawbacks include a reduced ability for customization, forced upgrades on Epic’s schedule, and tighter vendor lock-in.
- The Change Healthcare breach heightened concerns about reliance on a single vendor, possibly making CIOs skeptical that Epic SaaS would be more secure or resilient than their own IT capabilities.
- SaaS would increase health system dependence on Epic, with unknowns about what a post-Judy Epic looks like.
- Oracle Health talks up cloud-native ambitions but lacks market momentum, industry focus, and credibility to provide much of a medium-term threat. Health systems care less about technology compared to business results, proven ROI, and vendor responsiveness and stability. Oracle’s commitment, performance, and retention of internal healthcare expertise remains unproven, and customers have been historically burned by big tech outsiders who barged into (and then out of) healthcare.
- A full Epic rewrite is unlikely unless the reward to Epic clearly outweighs the risk. Few vendors have pulled this off. Meditech did it seemingly effortlessly with Expanse and Cerner (as a publicly traded company) sweated through many bad years until Millennium was fully baked. Otherwise a lot of vendor-touted technology improvement is pig lipstickery, and sometimes that’s all customers care about anyway.
- Epic dominates the market and will eventually run out of deep-pockets health systems to sell to. It doesn’t need to chase new customers by teasing their CTOs into an advanced state of technical arousal.
- Potential drivers for change are Oracle Health rebounding as a serious competitor; a demand for cloud-native AI and analytics; and regulatory pressures around interoperability and cybersecurity (which seem to be lessening by the day).
HIStalk Announcements and Requests
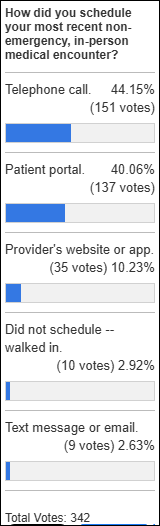
Most poll respondents book their medical appointments by telephone or patient portal. Some say they do it at the check-out desk at the end of their visit, which I’ve seen almost universally with dentists but commonly with doctors, although that experience probably involves routine chronic condition management.
New poll to your right or here: How much of your job performance can be measured using objective metrics?This came to mind while reading an article about how much of a pay cut office employees would take to work fully remotely. The article noted that managers who oppose WFH often oversee employees whose performance isn’t easily quantified by output metrics, which forces them to rely on in-office proxies such as hours worked, enthusiasm, and the perceptions of colleagues and customers. Another question might be that if your job performance isn’t being mostly measured by metrics, then why not? Is your work inherently unquantifiable, or is it that managers haven’t created the right metrics and instead rely on direct observation?
HIStalk sponsors: fill out this form to tell me about your HIMSS25 plans by February 24 and I will include you in my guide, which will look like the one above from last year..

Readers provided microphones and speakers for students in Ms. B’s elementary school classes in Kinston, NC. She reports:
You would not believe how student engagement has changed in our classroom!!! We faithfully use the devices during our math lessons. Students love when they are able to clearly share their thinking, using the microphone, as they give explanations while solving rigorous word problems. Being in the spotlight, they aren’t shy to speak out for all to hear. The Bluetooth speaker sits stationary in the center of the room so all voices are projected throughout. I love the range and how I’m able to walk around freely without even realizing that it’s still on. The students are able to hear me no matter if I’m in the front of the room or in the back of the room.
Sponsored Events and Resources
Instant Access Webinar: “How AI Addresses Resource Constraints Within Identity Data Management.” Sponsor: Rhapsody. Presenters: Lynn Stoltz, MS, director of product management, Rhapsody; Drew Ivan, MS, chief architect, Rhapsody; Michelle Blackmer, chief marketing officer, Rhapsody. Discover how to overcome the toughest challenge in identity data management: resource constraints. The presenters will cover how Rhapsody EMPI with Autopilot solves resource challenges like limitations in time, talent, and budget; Reduces costs and risks associated with inaccurate data; and boosts identity data accuracy through 98% decision-making precision.
Contact Lorre to have your resource listed
Acquisitions, Funding, Business, and Stock
ProPublica examines the history of Zolgensma, a taxpayer- and charity-funded gene therapy for a rare nerve disease in infants whose rights were acquired by a startup. The chief scientist gained partial ownership, the startup went public, and Novartis later bought it for $8.7 billion, netting the scientist $400 million, an investor $315 million, and the CEO $190 million. Novartis then priced the drug at a record $2 million per dose. Medicaid spent $309 million on it over four years, while Novartis made $6.4 billion. The article notes that 10 gene therapy products now cost more than $2 million per dose once Novartis set the price bar so high.
People

WellSpan Health SVP/CIO Hal Baker, MD announces that he will retire in July. He encourages those who might want to succeed him to apply for the York, PA-based job, telling me that “We have a fantastic team, are doing some very cool cutting edge stuff in AI, and I think my 30 years working for a single employer says about as much as one can about how good the opportunity is.”
Announcements and Implementations
Meditech signs its 100th Meditech as a Service client.
Epic integrates organ donation registration capabilities into MyChart in collaboration with the non-profit Donate Life America.
Mayo Clinic will pilot VoiceCare AI’s voice AI agent in three areas for pre-authorization and benefit confirmation.
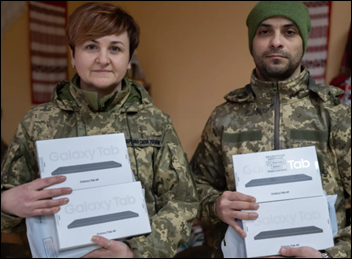
Ukraine’s Ministry of Defence deploys the first batch of 200 tablets to Air Assault Forces medics, who will use them to document frontline care in the military’s self-developed Electronic Primary Medical Records system. The tablets were donated by the Come Back Alive foundation, which supports members of the Armed Forces of Ukraine.
Other

In England, a trade union raises concerns about a hospital’s plan to use license plate recognition software to impose fees and fines. The website of technology provider ParkingEye says that the advantages are to “increase parking revenue, reduce car park abuse, and improve customer satisfaction,” also noting that 30 NHS trusts already use its systems. Complaints abound, mostly about being erroneously told by someone on site that it was free to park or to get validated, having their credit card hit with a huge charge with no response to appeals, and angry excuses of the “I was only a little over the time limit and it wasn’t my fault” variety.
Sponsor Updates
- Health Data Movers hires Andrew O’Hara as a health IT recruiter.
- TruBridge announces its selection as a preferred partner to healthcare services company Cibolo Health.
- Visage Imaging General Manager, North America Brad Levin recaps the first Sharp HealthCare Spatial Computing Health Care Summit in San Diego.
- Contessa Health (TN) works with Netsmart to develop and configure the first application in a suite of tools that is its new population health management platform for palliative care at home.
- Nym publishes a new case study, “Transforming Medical Coding at Inova.”
- Optimum Healthcare IT publishes a new white paper, “Improving Efficiency & Meeting User Demand with ITSM Practices in Healthcare.”
- Praia Health announces it has been granted a second patent for its account and experience orchestration technology.
- QGenda offers a new case study, “North American Partners in Anesthesia Achieves Faster, More Accurate Payroll with QGenda’s Schedule-Driven Time and Attendance Solution.”
- Waystar earns top rankings for its payment solutions in eight categories, according to Black Book Research’s latest analysis of AI-powered RCM software platforms.
- WellSky publishes an EHR checklist for behavioral health facilities.
Blog Posts
- Best Practices for Collaborating with Payers (FinThrive)
- CMS TEAM is coming: Why CIOs must act now on EHR optimization (Nordic)
- Top Physician Communication Frustrations (PerfectServe)
- The Cost of Doing Nothing (Praia Health)
- How Redox and Databricks are transforming prior authorization through interoperability (Redox)
- Powering the Prior Authorization Transformation (Surescripts)
- How a Healthcare Platform Transforms Patient Care & Operations (Symplr)
- How to Align Operations + Technology to Improve Patient Access (Tegria)
- Value-based care requires creativity and technology partnerships (Wolters Kluwer Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Follow on X, Bluesky, and LinkedIn.
Contact us.



Ref: “Care Everywhere number”
It is now too late to pursue further discussions on a national Unique Health Safety Identifier, particularly given the change in administration and new leadership at the Department of Health and Human Services.
It is unfortunate that, despite the dedicated efforts of many highly skilled professionals, the privacy-protecting benefits of a UHSI—along with its ability to streamline accurate patient matching—have been disregarded by short-sighted decision-makers, especially those currently in charge. While algorithms may approximate accurate matching, they cannot achieve the same level of precision as a well-implemented UHSI.
Regarding a Unique Health Safety Identifier, several organizations (e.g., DirectTrust, HL7) have workgroups developing standards/guidelines for a unique voluntary identifier that would achieve almost the same benefits as a federal mandate, probably with much less resistance. It’s not a simple change, as there are all sorts of complexities that need to be considered, but the Direct Trust PEHRLS (Privacy Enhancing Record Locator Service) workgroup could have a trial version by as early as the end of this year or early 2026. In the meantime, we need to work on standardizing matching approaches and how we display possible matches, which is the work we are doing with Epic (and hopefully Oracle/Cerner and others).
I think that it’s hysterical that car parking charges at hospital are a massive issue in the UK. I recall that when I first came to the US Stanford Hospital offered valet parking, I think for free. Of course when you get inside the building in the UK, everything is free. Not the case at Stanford or any other hospital in the US
PS the people who are most angry about hospital parking charges in the UK tend to be the staff who work there, who often get caught up in the fines
SaaS makes sense to me as an option for small practices. As the businesses get larger it gradually makes less sense until it stops making sense entirely. Even in a very large healthcare system? If the application is very niche, with a very limited user base? It might make sense there too.
Epic’s market tends to be larger healthcare systems, I believe. Meditech is strongest with small and medium-sized customers.
Our very large health system on the West Coast is Epic hosted
Sure, and that health system chose that. But why? It’s a complicated decision matrix for sure.
My take is, strategically, you are handing too much pricing power to your vendor. In particular, the vendor can raise their hosting fees. Under these conditions the customer has very limited options.
I’ve had the experience of a vendor strong-arming a price increase upon my company. It was shocking and violated a trust I had in that vendor. It broke a whole system of rules and norms that existed far outside of that particular vendor. That trust never returned in consequence.
Or imagine another scenario: Your hosted application starts performing poorly. You report the issue to the vendor and yet nothing changes. Eventually you learn that the vendor is limiting their infrastructure spend in order to increase profits. What can you do?
Every time you hand a vendor a lever of control, you increase your risk of this type of event happening. I must admit though, that there is no absolute protection against these risks either.
It’s a little unclear from the commentary what SAAS means to people.
Epic is clearly interested in targeting smaller hospitals and smaller ambulatory practices. They have the community connect model as well as Garden plot or whatever they are calling their model aimed at smaller practices. Before that they had some other branding called All Terrain or something equally forgettable.
Its clear Community Connect has enabled giant monopolistic health systems to increase their monopoly. I wish that there was equal focus by Epic on empowering larger independent practices or small standalone inpatient facilities. That would be true innovation IMO.
It’s hard to see exactly what that would look like. The non Epic inpatient is more cost conscious. They are either small, often rural hospitals without the money or for profit chains. The ambulatory crowd is either extremely cost conscious (ECW), very specialized (like ModMed ophthalmology), or looking for a vendor with services (Athena). It’s really not in Epic’s DNA to be any kind of these things.I think of SAAS as really a billing model for software that also involves hosting the software in some shared environment. I don’t think that delivery model has a meaningful impact for the non Epic market. I don’t think it can drive costs meaningfully lower and Epic has purposefully chosen to have more universal content and not offer services.
It’s too bad, because from a traditional HIT perspective, the independent ambulatory and specialty markets are the only interesting game right now. Non Epic hospitals and health systems are the ones competing on straight cost for quality basis, as opposed to having market power and political connections. It’s sort of boring watching all the HIT effort go into having the winners get bigger, and it’s not good for the industry. I wish there was a less focus on what vendor works best to add on to Epic and a little more focus on what technology company is doing something truly different, or even how these private equity firms are running their ambulatory acquisitions. But I understand that’s probably not what the greater HIT population wants to read, even if I think that would be more illuminating personally.
You have the cause and effect mixed up. Health systems are not consolidating because HIT is enabling them…HIT is creating products to support those efforts because that is where the industry is going. That’s not the fault of HIT. Profit-driven consolidation begets profit-driven software to enable that consolidation. The incentives creating this behavior are far upstream of HIT.
It’s true that organizations would be consolidating even if EHRs didn’t exist. I think it’s clear that HIT is enabler of that trend. HIT didn’t start the fire but it adds some gasoline.
To the point I was making, what if Epic poured the development and implementation effort they put into Community Connect into process and automation that made the product accessible to an unaffiliated, 25 bed hospital outside Missoula or an independent chain of 10 primary care+peds+one specialty. They probably would have ended up with a better product experience, about the same amount of money in the end, and they would have slowed the growth in healthcare costs instead of accelerated the rise in prices. I honestly think that the reason they didn’t was because of their culture as well as the culture of healthcare, which is set mostly by people who work in the upper echelons of Epic and Duke and KP and such. To a lesser extent, it’s set on this blog, and by you and I, the long time HIT workers.
I left Epic more than ten years ago, actually a lot more. Part of the reason is that when I joined Epic, there were still many customers converting from paper, and I could see that what they would end up with would be better, especially as Epic improved its product. I want to work somewhere that I can go home at the end of the day and say “the word is slightly better because I went to work today.” When I left Epic, it seemed like most people had EHRs and we were mostly making Epics pockets bigger at the expense of Cerner. And I have no love for Cerner, but I just didn’t see that as being something very useful for society. So I left to work on things that I thought would help outsiders and the little guys in healthcare. It honestly has been probably less lucrative than charging on the Epic train, but I think it’s more helpful. Even if the incentives are upstream of us, we aren’t simple economic agents, we’re humans. We can work for or against the system.
That isn’t meant to be a dig at you or Epic employees really. People at Epic are fixing bugs and improving the product for end users, and that is certainly making other people’s lives easier. It’s not a simple task to debug M code and I don’t want to disparage the people that do it. Its just a commentary on the sad place the industry is in, and an acknowledgment that we are all part of the system, even those companies that claim a moral high ground.
“what if Epic poured the development and implementation effort they put into Community Connect…”
Epic does not pour a whole lot of development effort into Community Connect. It’s not a different product, it does not really have different features either. It’s just a licensing arrangement where Epic customers can extend Hyperspace/Hyperdrive access to affiliated, non-employed users and practices. Does Epic spend some implementation effort on Community Connect? Sure? But only for particularly large projects – otherwise most Epic-using organizations just manage the rollouts themselves.
Epic released Garden Plot a few years ago to enable smaller practices to band together to get access to Epic. Not sure if that is getting any traction, but the option is out there.
I have to quibble with your take. From what I’ve seen, HIT is both a cause of, and an enabler for, consolidation.
Just take a look at environments where for-profit is not really a factor. There is still high demand for HIT systems, with concomitant consolidation trends. The clinicians want it (even as they gripe about the data entry requirements). The patients want it. The regulatory environment drives us towards HIT. The corporate administrators like the idea of HIT.
Who would be an advocate for distribution, best of breed, and dis-aggregation? I’m sure you can find such people but they aren’t in the driver’s seat.