Today's post contains the phoenixes rising from the ashes of the post COVID telehealth era. There's two things that destroy…
News 3/27/24
Top News

Masimo considers spinning off its consumer business, which includes personal health and audio products, while retaining its healthcare and telehealth solutions.
Reader Comments
From Disingenuous: “Re: Judy Faulkner’s giving pledge. It’s shallow since she’s giving her share of Epic to a foundation that will still have majority control, someone who will carry on her legacy and maintain her vision from the grave.” I read that years ago, thinking that the question then becomes who’s on the foundation and how it interacts with a company that has always had one focused leader who is also the majority owner. Epic has always had a board, I hear, although I know nothing about its members and level of control.
From Psych MD: “Re: VA OIG’s report. The report identifies quite a few problems with the patient’s follow-up mental health care, but using root care analysis leads organizations to identify a single failure among several, to recommend corrective actions even when it seems likely that they would not have affected the outcome, and in this case looks to the EHR as a source of blame or a magical fix. I don’t know why root cause analysis has become ascendant over FMEA or other approaches to optimize care and safety.” The full VA OIG report puts a lot of blame for the patient’s death — which was not determined to be a suicide even though the patient had a history of suicidal ideation — on Oracle Health, but these points seem relevant:
- The EHR failed to issue the VA-specified number of staff reminders to schedule new behavioral health appointments for no-shows or cancellations.
- The patient had changed their phone number and didn’t respond to appointment scheduling messages.
- The VA contacted family members, who told them the patient was doing OK and didn’t provide the new telephone number, at which time the patient’s flag for being at high suicide risk was turned off, which prevented ongoing suicide prevention reach-outs.
- The patient died of cardiac arrhythmia after using inhalants, of which they had a documented history but denied current use, two months after their most recent visit.
- This complex case resulted in some EHR changes involving missed appointments, but the patient was not cooperative despite VA employee efforts and no evidence exists that any changes would have improved this patient’s unfortunate outcome.
From AT: “Re: Epic’s succession plan. What’s yours? I’m hoping that you will post an obituary. My career and even my passion for health IT are forever indebted to everything you have provided me and the entire industry.” I appreciate that, but I want no part of limelight, prehumous or posthumous, for doing what I consider an empty-room hobby. You probably won’t even notice my bucket-kicking absence anyway since Jenn can keep the news coming until existing sponsorships expire and the site can go gracefully dark without stiffing anybody (no pun intended).
HIMSS24 Comments Review

Several folks have said it will be hard for HIMSS / Informa to figure out what needs fixing about the annual conference based on the comments that I received. I’ll take the counterpoint in summarizing the list as being mostly minor and personal gripes, with few underlying themes that indicate mass, irreparable dissatisfaction. My thoughts:
- Attendance and exhibitor count are the ultimate benchmark. Those were just fine for HIMSS24. Informa isn’t forced to rescue a conference whose relevance and reach has slipped beyond repair.
- HIMSS20 and the HIMSS23 carpet debacle soured a lot of people on HIMSS, so hopefully Informa’s acquisition cost reflected the value of the tarnished jewel and the company has the vast experience that is needed to improve it. It also means that Hal Wolf has relinquished a lot of power to Informa, which his critics will celebrate.
- HIMSS conference educational presentations and keynotes mostly draw yawns, but HIMSS can improve those now that Informa is managing the exhibit hall logistics.
My suggestions:
- Steal ViVE’s “refreshments and meals included” idea, although that will be hard to scale up to a HIMSS-sized conference due to physical space limits. Requiring highly paid executives to fight for space to sit on dirty carpeted floor to dribble dressing from their $20 salad on themselves instead of networking with fellow attendees is absurd. If money is the problem, sell $50 daily vouchers for access to a private area near the exhibit hall that offers food (including fresher and healthier options) and coffee for most of the day, an expanded model of the now-dead HIMSS Bistro offering that I have always thought worked really well when I paid for a ticket. The other limitation here is that convention centers impose their monopoly powers on F&B to charge astronomical prices, such as $73 for a gallon of Starbucks coffee and $29 for a boxed sandwich or salad in Orlando, all plus a mandatory 21.5% service charge plus tax.
- Dial back the chirpy influencers and HIMSS Media cheerleading unless the target audience is non-decision makers who like that sort of self-aware gushiness.
- Limit the conference to three days and keep the exhibit hall open during all show hours. Nobody enjoys the last-day ghost town, and HIMSS could save money on facilities and let people get back to work by declaring that three days is enough. HIMSS25 will do exactly that, although HIMSS26 sees the return of Tumbleweeds Friday.
- Get better keynote speakers, schedule them early in the week, and announce them before attendance decisions have already been made. Pay one celebrity speaker, if you must, who packs star power while knowing and caring nothing about the work of audience members (hello, Nick Saban), but otherwise get non-vendor insiders on the big stages.
- Take advantage of ViVE’s weak spot of high registration fees by using HIMSS clout to lower them, attracting more provider-siders. That won’t necessarily stem the C-level migration from HIMSS to ViVE, but could correct the inflated vendor-provider ratio and draw in health system directors, managers, and clinicians who have influence on technology decisions but who have limited travel money. I would argue that HIMSS can do fine without CIOs since they rarely emerged from their HIMSS VIP sequestration to hit the show floor anyway.
Webinars
March 27 (Wednesday) 3 ET. “Houston Methodist: Deploying clinical AI at scale for improved outcomes.” Sponsor: Health Data Analytics Institute. Presenters: Khurram Nasir, MD, MPH, chief of cardiovascular disease prevention and wellness, Houston Methodist DeBakey Heart & Vascular Center; Brenda Campbell, RN, senior consultant, HM Health System Innovations; Nassib Chamoun, MS, founder and CEO, HDAI. The presenters will share how an interdisciplinary team collaborated to successfully use predictive models and a novel AI-driven approach to address post-discharge mortality. They will also describe how they expanded use of the platform to reduce clinician time spent digging through the EHR with a one-page risk profile, including codes extracted from notes using generative AI, and targeting their highest risk patients for extra attention. They will speak to how they overcame barriers to bringing AI at scale to support clinicians across the care continuum.
Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Sales
- Nebraska Medicine will implement EVideon’s Vide Health smart room technology within its Innovation Design Unit.
- The Medical University of South Carolina will implement Flatiron Health’s Flatiron Assist oncology clinical decision support software at its cancer center.
- Prisma Health will extend its use of Bamboo Health’s Pings, Spotlights, and Discharge Summaries across its organization and InVio Health Network.
- Samaritan Health Services (OR) will provide virtual urgent care services via Epic MyChart from KeyCare.
- Children’s Hospital Los Angeles offers Nabla’s Copilot AI assistant to its pediatric specialists following completion of a pilot project.
- Community Health Network (IN) will use Ferrum Health’s reference AI architecture to deploy radiology algorithms.
People


CompuGroup Medical will promote Benedikt Brueckle to US CEO in January 2025. He will take over from Derek Pickell, who will retire at the end of this year.

Heather Dunn, MBA (Vanderbilt University Medical Center) joins The SSI Group as president.

Collette Health names Christine Gall, DrPH, MS, BSN (Gall Consulting) chief nursing officer.
Announcements and Implementations

OhioHealth Van Wert Hospital goes live on Epic as part of a system-wide transition that was first announced in early 2021.
Black Book Research announces winners of its awards for highest hospital user satisfaction and clinician satisfaction, as determined by 14,000 respondents.
Malaysia’s health ministry says that it will rejuvenate Selayang Hospital’s Cerner EHR, which was the country’s first paperless system, that has deteriorated to the point that the hospital went back to paper.
Amazon expands its same-day prescription delivery, which is already offered in five cities, to New York City and Los Angeles. The company also notes that it is using AI behind the scenes to prepare prescriptions for pharmacist review to increase efficiency.
A study by The Clinic by Cleveland Clinic finds that its virtual second opinions save the patient or their payer $8,705. Two-thirds of its second opinions recommend a change in diagnosis or treatment, while 85% of patients who had been told that they needed surgery were instead recommended an alternate treatment. The $1,850 program includes a video call with an RN, concierge collection of medical records, and referral to a Cleveland Clinic expert who provides a written second opinion.
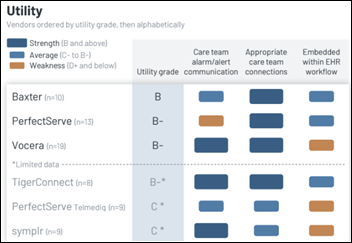
A new KLAS report on clinical communications interoperability concludes that no vendor connects consistently across all use cases — which include communication with outside physicians; integration with staff scheduling; timely alert and alarm routing; integration with EHRs, dietary, and transport systems; and communication of after-hours needs — but deep adopters are starting to unify their communications.
Government and Politics
Senator Mark Warner (D-VA) introduces the “Health Care Cybersecurity Improvement Act of 2024.” If passed, the bill will enable eligible providers to receive advanced and accelerated payments in the wake of a cyberattack, provided they and, if applicable, third-party vendors meet certain cybersecurity standards. Warner launched the Senate Health Care Cybersecurity Working Group last November.
Privacy and Security
Petersen Health Care, one of the country’s largest nursing home operators, files bankruptcy due to a double whammy of cybersecurity incidents — an October 2023 ransomware attack that delayed bills and then the Change Healthcare cyberattack that reduced receivables. The company operates 90 nursing homes in the Midwest and reported $340 million in revenue in 2023.
Other
UK HealthCare’s Chandler Hospital (KY) opens a new ICU floor equipped with remote patient monitoring technologies, including bedside patient engagement software from GetWell and video monitoring from Caregility.

Forbes Hospital (PA), part of the Allegheny Health Network, will equip a 47-bed unit with smart patient room and virtual nursing technology in the coming weeks.
Sponsor Updates
- EClinicalWorks becomes a HRSA-approved EHR vendor for UDS+ submissions.
- Availity and Bamboo Health will exhibit at the State HIT 2024 Connect Summit April 1-4 in Baltimore.
- Divurgent publishes a new success story, “Divurgent Consolidates Over 120 EHR and IS Applications After Hospital Acquisition.”
Blog Posts
- Addressing Epic EHR Support Gaps When Resources are Scarce (CereCore)
- How Happy Are You at Work? (AdvancedMD)
- HIMSS 2024 – Key Takeaways: Let’s Hear from Lenny! (Agfa HealthCare)
- The Win-Back: ApolloMD Learns There’s No Match for AGS Health’s A/R and Coding Services (AGS Health)
- Going on offense: Filling the gaps in healthcare cybersecurity (Altera Digital Health)
- How the zero-copy data lake will advance modern healthcare and data (Arcadia)
- Social Determinants of Health Tools: Context in Communications (Artera)
- Understanding the Change Healthcare Breach and What It Means for Your Healthcare Organization (Clearwater)
- Black Box for the Medical Industry Provides Unprecedented Data (Dimensional Insight)
- Retaining Excellence: Strategies for Keeping Top Talent in the Healthcare Technology Industry (Direct Recruiters)
- Generative AI Integration into the EHR – Welcome to the Healthcare Revolution (EClinicalWorks)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



RE Judy Faulkner’s foundation wishes: Different area, but read up on the Barnes Foundation to see how things work out in the long run with this sort of thing. https://en.wikipedia.org/wiki/Barnes_Foundation
The Barnes Foundation is not a good comparison. Dr. Barnes was an eccentric who wanted his incredible art collection to have extremely limited public exposure in a building that was an antique. Now his collection is available to the public in a beautiful building in downtown Philadelphia. Judy’s intentions are very in line with the board, the staff, and the customer base’s needs.
I read the article, and it reads like a recipe for failure as an art gallery:
– closed from 1925 – 1961, due to court challenges (!);
– located in an obscure town (Merion??);
– after 1961, public access was initiated. To a whole 2 1/2 days a week;
– 1998 sees the beginning of another round of court cases.
There are just a stream of red flags with this story. No wonder the Foundation ran into financial trouble! Between choking off the visitor access and the endless legal wrangling.
Sounds like an object lesson in how NOT to set up an art Foundation & Museum.
I think Disingenuous is confused (or simply not aware of how it has been architected). How control of Epic is handled after Judy’s exit is not related to her pledge to donate 99% of her wealth (via her Roots & Wings foundation).