Giving a patient medications in the ER, having them pop positive on a test, and then withholding further medications because…
News 9/21/22
Top News

A Washington federal judge clears the way for UnitedHealth Group to acquire Change Healthcare, rejecting a Department of Justice lawsuit that attempted to block the deal. DOJ had argued that the acquisition would give UnitedHealth’s insurance business access to the claims data of competing payers, which would increase healthcare costs.
The acquisition price is $7.8 billion versus the $13 billion that was reported when the acquisition was first announced in January 2021.
The approval requires Change Healthcare to divest its ClaimsXten claims payment and editing software business to TPG Capital for $2.2 billion.
UnitedHealth will merge Change with its Optum Insight analytics and consulting business.
Reader Comments
From Bonedigger: “Re: executive coaching. What advice do you have to make that a career?” My advice would be to choose something else, at least based on my experience with a few health IT folks who tried the executive coaching biz and failed quickly. Senior-level people may overestimate the value of their experience in unrelated work such as consulting, teaching, and coaching, but many organizations prey on their vanity by selling them coaching education and certifications. They still have to find customers (which is the hardest part, like in all businesses), develop the right chemistry, and do good enough work to be retained. The fact that few of them hired coaches for themselves isn’t much of an endorsement.
HIStalk Announcements and Requests
A memory of a long-ago health IT executive sent me back to Vince Ciotii’s remarkable HIS-tory series, which turned into several hours of “where are they now” Google searches of the folks he mentions in it. I interviewed Vince for the last time in September 2019 and asked him what his epitaph would say, and he replied that the series was his proudest work in 50 years as a health IT executive. Vince’s own final chapter was written upon his death in September 2021.
Webinars
September 22 (Thursday) 1 ET. “ICD-10-CM 2023 Updates and Regulatory Readiness.” Sponsor: Intelligent Medical Objects. Presenters: June Bronnert, MSHI, RHIA, marketing director, IMO; Julie Glasgow, MD, marketing manager, IMO. The yearly update to ICD-10-CM is almost here. Prepare your organization for a smooth transition, and avoid any negative impacts to your bottom line, with an in-depth look at the upcoming changes. Listen to IMO’s top coding professionals and thought leaders discuss the 2023 ICD-10-CM coding changes. This webinar will review additions, deletions, and other revisions to the ICD-10-CM code set and how to make sure you get properly reimbursed.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock

Search firm investor Starfish Partners acquires Direct Recruiters, which specializes in staffing solutions for a variety of industries including healthcare IT and life sciences.
Online prescription startup Peak stops offering its ketamine-based psychedelic therapy for drug-resistant depression and anxiety to new patients, and will cease operations at the end of November.

Enterprise imaging company Intelerad Medical Systems acquires image exchange vendor Life Image for an undisclosed sum. Intelerad now boasts one of the largest image exchange networks, having acquired competitor Ambra Health last year.
PillPack founders TJ Parker and Elliott Cohen announce that they are leaving Amazon, which acquired the online pharmacy in 2018 for $753 million with little impact since.

McKesson will acquire Rx Savings Solutions, which offers an app that recommends cost-saving prescription changes to members, for up to $875 million in cash. Founder and CEO Michael Rea, PharmD started the company in 2009 after working as a pharmacist for Walgreens and OptumRx.
Transcarent launches a medication price transparency program to give self-insured employers more control over their prescription benefits.
The 28-year-old founder of digital shopping cart vendor Bold – who quit the CEO job in January 2022 days after a fundraising round that valued the company at $11 billion – will become founder and CEO of Love, a Kickstarter-like crowdsourcing and clinical studies platform for homeopathic products. The company will sell digital tokens, which allows investors to vote on which studies to fund. Ryan Breslow – who avoids meat, gluten, caffeine, alcohol, supplements, and after-dark lights and electronic screens – says, “I think my superpower is that I’ve never done health before.”
Sales
- Albany Med Health System (NY) will implement Epic in 2024.
- Children’s Healthcare of Atlanta selects real-time location systems software from Vizzia Technologies.
- The VA renews its VistA-integrated dialysis EHR contract with DSS in a five-year, $27 million deal.
People
Orb Health names Lisa Simon, CPA (Monongalia Health System) CEO; Gordon Jaye, MS (Aspirion) SVP of transformation and patient engagement; and Eric Van Portfliet (Firstsource) CTO.

William Cavanaugh, MBA (Lyniate) joins Concord Technologies as president.

DMEscripts hires John Brady (Anthem) as CEO.


Global Healthcare Exchange promotes Tina Murphy to president and CEO. She replaces Bruce Johnson, MBA, who will become executive board chair.
Announcements and Implementations
Johns Hopkins Medicine’s Office of Telemedicine announces that it has conducted 1.5 million telemedicine visits with 420,000 patients since March 2020. The office plans to expand emote patient monitoring capabilities to include ambulatory and complex care and the availability of virtual consults between Johns Hopkins facilities.

West Cecil Health Center (MD) implements Bluestream Health’s virtual care platform-as-a-service.
Verato launches a Universal Identity platform that consists of Verato Patient Journey and Verato Provider Data Management.
Epic implementations in Denmark and Finland are “still troubled” years after go-live, according to authors of an article in the International Journal of Medical Informatics who say that usability has not been optimized, clinical time to perform tasks has increased, and clinician dissatisfaction is at 32%. The authors noted these issues, which are common in large implementations:
- Project participants failed to pay attention to the extent of user changes that were involved and issues raised in Denmark’s first go-live were not addressed before the second.
- Grand expectations are needed to generate project enthusiasm, but may gloss over real-life concerns when realities intrude.
- Tax-supported Nordic healthcare does not require billing insurers, but Epic’s US-centric clicks and worfklows that support it could not be configured away. Translation of user interfaces from English to Danish and Finish also caused problems, especially with search functions.
- Both countries spent years configuring Epic for their requirements, with Danish regions focusing mostly on standardization and the Finnish region on local preferences. The authors say that “neither approach has resulted in a well-liked system.”
- The EHR rollouts, which increase documentation requirements, created clinician stress. The plan to lay off medical secretaries to save money and then transfer their documentation work to physicians was a key issue.
- The authors recommend following up promptly with users who report problems, assume that a return to productivity will take at least 3-12 months and likely longer in these countries, and be cautious about changing work processes that clinicians oppose.
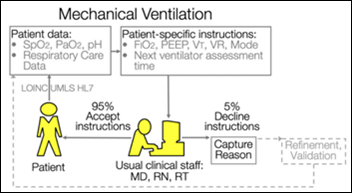
A large group of expert authors proposes to reduce deviations in best-practices patient care by using EActions, which are validated expert systems that are designed to manage a specific clinical task or condition by considering existing patient information to the point that no clinician review is required. The authors distinguish between using such closed-loop technology to make evidence-based treatment decisions – which is possible once a diagnosis has been made – instead of for generating a diagnosis, for which AI is not sufficiently mature. Rules-based treatment for acute respiratory distress syndrome is replicable because if-then rules can adjust ventilator settings and order labs just as clinicians would do, while treating heart failure is not replicable (and thus not suitable as an EAction) because the logic is more complex than simply matching if-then rules to existing data points. The authors predict that implementation of EActions will reduce clinician burden and EHR data noise, allowing comparative effectiveness clinical research questions to be addressed by learning healthcare systems as a by-product of delivering evidence-based care.
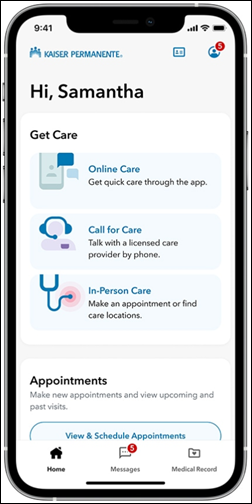
Fast Company names Kaiser Permanente as its 2022 Design Company of the Year for its app redesign, which KP says was associated with an 80% increase in online appointment booking, a doubling of website visits, an increase of digital experience satisfaction from 86% to 92%, and an 84% digital registration rate of members. KP says it is piloting a feature in which the app will offer location-based notification of available services to campus visitors.
NIH awards a $2.7 million grant to Eko to develop a machine learning algorithm to detect pulmonary hypertension using its smart stethoscopes
Government and Politics
Anonymous US Army recruiters complain that the DoD’s Cerner system, which was supposed to speed up the time required to get new recruits processed and in uniform, has instead lengthened the timelines to the point that parents are complaining and recruits are changing their minds about enlisting. The recruiters say new policies and capabilities force them to wait to receive medical records relating to Cerner-flagged histories from providers, which can take weeks. Army officials say that the problem isn’t Cerner, it’s that recruits are often taking antidepressants and ADHD drugs and thus require a heath review that may get them disqualified for service. Anonymous online commenters complain that it was easier in the good old days because recruits could simply lie or plead ignorance about their medical histories.
A lead story in the New York Times says that the lack of public health data limits US response to outbreaks, observing that state and local health departments remain stuck in a world of fax machines, manual data entry, and phone calls. CDC’s attempts to quantify the spread of the Omicron variant of COVID-19 required it to ask Kaiser Permanente to analyze its own patient data. The lack of data has limited the government’s ability to make decisions about boosters and to understand breakthrough cases. The federal government is requiring hospitals to show progress toward automating CDC case reports as triggered by EHR diagnoses, but only 15% hospitals have accomplished that.
Other

A South Dakota paper profiles Sanford Health’s plans for its recently announced $350 million Virtual Care Center and the impact it will have on local and regional patients, as well as nearby health systems: “We would like to be a partner in that,” says Horizon Healthcare CIO Scott Weatherill … We’re definitely drinking the Kool Aid on this, and we fall back on telemedicine readily to continue to provide care, keep our clinics open, and offer additional services to our patients.”
Cooper University Health Care’s MD Anderson affiliate will get a new $2 billion building that will add 100 beds to its Camden, NJ campus.
A Surescripts analysis finds that prescription pick-up rates increased by 3.2% when prescribers used the company’s Real-Time Prescription Benefit, which also saved an average of $38 per prescription.

Paging Dr. Weird News Andy: a man in India is hospitalized for three weeks as doctors remove a 7.5-inch deodorant can from his colon, whose presence he declined to explain.
Sponsor Updates
- Oracle Cerner publishes a new business brief, “How a Real-Time Health System Addresses Challenges.”
- Agfa HealthCare embarks on an upgrade enterprise imaging project with UC Christus Health Network in Chile.
- IDC MarketScape includes Agfa HealthCare in the Leaders Category in its “European Enterprise Medical Imaging 2022 Vendor Assessment.”
- AGS Health publishes a new case study, “CAC Implementation improves hospital revenue by $1.03MM.”
- Arrive Health names Nikki Heider marketing manager.
- Therapy Brands renews its partnership agreement with OptimizeRx, which gives users of its e-prescribing platform access to diagnosis support, affordability, access, and adherence resources.
- Baker Tilly releases a new Healthy Outcomes Podcast, “Trends, issues, and updates in the senior service industry.”
- Biofourmis will present at the Academy of Physicians in Clinical Research Annual Meeting October 7 in Fort Lauderdale, FL.
- Black Book Market Research publishes its latest “State of Global Healthcare Technology” report, which reveals adoption trends, market dynamics, and top-rated vendors across 55 countries.
- Divurgent announces a refocused mission, vision, and advisory services.
Blog Posts
- Build vs. buy in healthcare IT: The battle for buy-in (Arcadia)
- Climbing the Executive Ladder – One Class at a Time (Ascom)
- CHQR Badges – What are They and Why They’re Important to Community Health Centers (Azara Healthcare)
- What is Whole Person Care? (Bamboo Health)
- 7 ways to optimize expenditures associated with surgical procedures (Bravado Health)
- Bringing “Top Flight” Communications to the Academic Medical Center (CareMesh)
- Looking forward to new innovations in the healthcare industry (Oracle Cerner)
- Overcoming Healthcare IT Staffing Challenges (HealthTech Resources)
- What Conditions Qualify for Chronic Care Management? (ChartSpan)
- Measuring Digital Identity and IAM Maturity to Advance Digital Initiatives in Healthcare (CHIME)
- We’ve Unveiled Our Brand-new Brand (Clearsense)
- Healthcare Apps Promise Powerful Outcomes – If Patients Use Them (CoverMyMeds)
- Evolving the Training Paradigm – A Breakout Session at the Arch Collaborative Learning Summit 2022 (Divurgent)
- Keeping an Eye on Patients in Transition (EClinicalWorks)
- Research Needs Robust Data: The CDC Utilizes the PINC AI Healthcare Database (Premier)
Sponsor Spotlight
ChartSpan recently released new clinical claims data on the effectiveness of Chronic Care Management programs. If you are looking for a partner in high-quality value-based care programs that actually deliver results, contact us today.
(Sponsor Spotlight is free for HIStalk Platinum sponsors).
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.






I initially read “Nordic” as relating to the Nordic Consulting group based in Madison. It turns out that in this context it is about Nordic countries in the frigid bits of Europe. Oops.
The new Kaiser App is fantastic from both a patient point of view, and an EMR vendor. Today I saw my PCP. I checked in online last night when prompted by at text from Kaiser, and when I arrived today I had a text with a code; once I replied with the code, I was ‘on the board’ in their waiting area. You could choose text or QR code check-in. Text doesn’t require you to go to the kiosk, so I chose that. I sent a text to my PCP on the portal yesterday, and it notified me that she was out of the office until today and might not respond quickly, then gave me alternate choices, ie., reach the covering provider or call the Advice Nurse line. I love, love, love that feature!
This seems laughable and a bit ridiculous that Army recruiters are blaming an EMR system is keeping them from recruiting effectively or timely.
I wonder if the Nordic Epic customers could be happy with any commercial offering. Force fitting an application and new workflows often leads to unhappy users. These countries have unique workflows (perfectly valid for them to have of course) …, so fitting an EHR designed for other locales and all the associated moving parts is likely an unreasonable goal without being willing to change themselves. Users have every right to be unhappy when the new solution just slows many systems and procedures down.
I pondered at the time these countries bought into Epic — was this ever going to work out? The money and expansion opportunities was apparently too great to pass up.
The history and track record of US firms successfully installing clinical apps in EU countries is fraught with failure. Almost every major vendor over the last 40 years hit the problems you note. Your reasons are right on, I experienced it first hand some 20 years ago. In some cases it has lead to the demise of the firm. The only real solution is an almost total re-write of the system to match the varied work flows. A very, very costly and risky undertaking..
“I think my superpower is that I’ve never done health before.”
And starting a homeopathic, crowd-sourced clinical trials business?
Cool.
“Grand expectations are needed to generate project enthusiasm, but may gloss over real-life concerns when realities intrude.”
Ohhh, I relate to this. The use of “the Vision Thing” is needed at every level of a major project. Therefore it is routinely and widely sold that way.
Typically though, the go-Live version you get is actually rather vanilla. It may do a couple of nice things, but it rarely lives up to the grand vision you sold early on. If you are persistent and lucky, gradually you can start building the really nice stuff.
The other matter is that it takes the users some time to learn how to leverage a new system. Even a very rich, capable system? The users need time to find and get comfortable with the functions that work best for them. Normal corporate training doesn’t quite get the users to that point either–they get too much training content in too little time.
Real understanding, comfort, and smooth workflows take time.