I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…
News 6/25/21
Top News
Shares in Doximity, which set an IPO share price of $26 versus the expected range of $20 to 23, close at $53.00 on their first day of trading on the New York Stock Exchange, valuing the physician network vendor at $7 billion.
Reader Comments
From Muumuu Summer: “Re: Epic. Are you hearing that they seem to be losing more employees than usual? It seems like they are bringing back a previous break-the-glass strategy by having senior people cover open positions until they can be filled, which can leave clients without a permanent person for months.” Epic clients are welcome to report their experience.
From Watcher of the Data: “Re: Avaneer and blockchain. You are dead right about this. The most amusing part of this is that blockchain won’t ‘solve’ the interoperability problem – it can become useful only once the problem has been solved.”
From Percolator: “Re: Epic’s sepsis model. Cerner has a free one that gets little use, and the company has had trouble selling models for other conditions. Every condition needs to be mapped to hospital work flow – who do you alert and how, and what is the recipient supposed to do? These models add little incremental value because (a) doctors are already very good at detecting sepsis and starting antibiotics, and (b) 90% of sepsis is community acquired before the patient is admitted. ‘Watch this patient more closely’ is not worth much, especially if doctors and nurses already suspect sepsis.” Thanks. I’ve removed identifying information since I wasn’t sure this comment was intended for public display.
From Ossify: “Re: Epic’s sepsis model. Why should anyone care what the algorithm does as long as it works?” You wouldn’t want to harm someone, either by overtreating or undertreating, because a software model was trained on a bunch of data and “learned” from facts that are clearly irrelevant or not universally applicable. Example: Epic developed a patient no-show model awhile back that incorporated the patient’s religion and body mass index in predicting whether they would show up for appointments, and researchers found that removing those features didn’t reduce the model’s predictive powers but eliminated some inequity issues. Did Epic really think those factors were relevant, or was their data science knowledge insufficient? Then there’s the “what do we do with this” issue – should appointments be double-booked in case those patients really do skip their appointments (and what happens if they don’t?) or perhaps could the information be less invasively and more constructively used to send reminders or to understand that particular patient’s possible issues with venue location, transportation, or available hours that could be resolved by suggesting a different location? AI is amazing for being able to detect data patterns that humans haven’t, but if pitched to replace or even enhance expert judgment, it’s the customer’s job to make sure that the algorithms work in their particular situation. I’m not sure the average health system has the expertise to make those evaluations, so that’s why outside review is a reasonable recommendation.
From Bagna Cauda: “Re: mental health apps. Which ones are best?” I’m skeptical that any of them accomplish much given the lack of peer-reviewed studies on their outcomes. FDA seems to lack interest in holding their developers accountable even when they are clearly being pitched for use in medical or psychological situations. It doesn’t help that psychological counseling itself may have outcomes that are hard to prove. Lastly, the nature of these behavioral health app companies is that they are pandering to investors who demand fast growth Silicon Valley style, which means their customers will have minimal human involvement and instead will interact with scalable, cookie cutter technology that offers the opposite of the human interaction that many people crave. It also seems that some vendors expect users to stop paying once the limited value of the app becomes clear, so they refocus on selling to employers and insurers (healthcare excels at separating the people who consume a service from those who pay for it).
Webinars
June 30 (Wednesday) 1 ET. “From quantity to quality: The new frontier for clinical data.” Sponsor: Intelligent Medical Objects. Presenters: Dale Sanders, chief strategy officer, IMO; John Lee, MD, CMIO, Allegheny Health Network. EHRs generate more healthcare data than ever, but that data is of low quality for secondary uses such as population health, precision medicine, and pandemic management, and its collection burdens clinicians as data entry clerks. The presenters will review ways to reduce clinician EHR burden; describe the importance of standardized, harmonious data; suggest why quality measures strategy needs to be changed; and make the case that clinical data collection as a whole should be re-evaluated.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock

Providence-owned Tegria acquires healthcare AI vendor KenSci.
Subscription-based opioid use disorder virtual care vendor Bicycle Health raises $27 million in a Series A funding round.
National emergency medical services provider Priority Ambulance acquires software vendor Randseco, which offers the StatCall digital patient logistics solution that supports information exchange among ambulances, hospitals, payers, and non-medical transportation services.
CitiusTech acquires Pittsburgh-based payment technology consulting firm SDLC Partners.
Sales
- The University of Texas Health Science Center at Houston engages ReMedi Health Solutions to offer personalization training for 2,000 clinicians in 18 specialties as it implements Epic. The company also provided an AI-powered virtual assistant for workflow help and tipsheets.
People

Healthcare IT Leaders hires Patrick Dougherty (Allscripts) as CTO.

Pallav Sharda, MBBS, MBA, MMI (Google) joins employer bundled health services platform vendor Carrum Health as chief product officer.


Well Health hires John Knotwell, MBA (Get Bridge) as chief revenue officer and Marissa Morrison (Foursquare) as VP of people.

Sheeza Hussain (Hillrom) joins remote patient monitoring technology vendor Bifourmis as chief commercial officer.

RCM services vendor Kemberton names Deanna Gray (Millennia) as SVP of customer success.

Peter Arduini (Integra LifeSciences) is named president and CEO of GE Healthcare, effective January 3, 2022.

Virtual-first urgent care and primary care clinic HealthTap promotes co-founder and COO Sean Mehra, MBA to CEO.
Announcements and Implementations
Healthcare Triangle releases DataEZ, a cloud-based analytics service that that can manage large quantities of data, including real-world data from remote monitoring, digital health services, and clinical trials.
Medical imaging software vendor Novarad announces GA of a software-only version of its CryptoChart image sharing product that uses a QR code to access the cloud-based information.
Rehabilitation therapy platform vendor WebPT recaps its recent accomplishments – 20,000 clinic customers and a 40% market share, release of its Digital Patient Intake tool, key leadership appointments, and launch of an integrated virtual visit solution.
WellSky-owned CarePort announces a care coordination solution for ambulatory providers, which will allow them to connect patients to home- and community-based organizations directly from their EHR and to maintain two-way communication during the referral process.
3M will establish a Digital Science Community in Dublin, Ireland, employing 100 people to do R&D work for its HIS division.
MGMA and WhiteSpace Health release MGMA DataDiscovery, a physician practice performance analytics tool for medical groups.
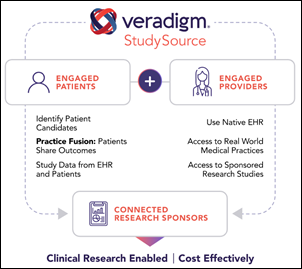
Allscripts-owned Veradigm and pharma contract research organization PRA Health Sciences develop an EHR-based clinical research network that uses Veradigm’s StudySource platform.
Texas Children’s Pavilion for Women launches PeriWatch Vigilance in Malawi, with the fetal monitoring system being provided at no charge by PeriGen.
Omny Health develops a de-identified EHR data repository for dermatologic pharma research, offering the data of 7.5 million patients that was collected from 1,000 dermatology providers. The company announced GA of its anonymized data research platform in early May. Co-founder and CEO Mitesh Rao, MD, MS was Stanford Health Care’s chief patient safety officer through 2017 and remains an emergency medicine professor at the Stanford University School of Medicine.
Other
England’s NHS publishes a draft data strategy that outlines NHSX’s use of data to give patients better access and control, to allow systems to share records, and to support research. It calls for the NHS app to allow patients to review test results, medication lists, procedures, and care plans and to be able to manage appointments, refill prescriptions and contact health and care staff. NHS also responded to concerns about its data-sharing plans by committing to publish a health data transparency statement by 2022.
Epic spokesperson Barbara Hernandez responds to the study in which Michigan Medicine researchers found that its sepsis alerting tool performed poorly, leading the authors to urge health systems to review the inner workings and past performance of such algorithms before using them in patient care. Epic’s points:
- Customers have access to the full model, its formulas, and its accuracy measurements, all of which are published on Epic’s UserWeb.
- The authors used a hypothetical approach that did not consider the analysis and tuning that is required before real-world deployment.
- The tool has helped clinicians provide life-saving interventions to thousands of patients that might have been missed otherwise.
- Michigan Medicine provided a positive review of the system in a UGM presentation in describing how pediatric patients are screened within two minutes of developing symptoms.
Meanwhile, one of the authors of the Epic Sepsis Model article that was published in JAMA Internal Medicine – nephrologist, assistant professor, and machine learning lab director Karandeep Singh, MD, MMSc of University of Michigan Medical School – provides further information via Twitter:
- The authors ruled out configuration and mapping errors that often create low data AUCs (area under the curve). Epic’s AUCs were much higher in its own sensitivity analysis.
- Singh notes that AUC is driven by two factors – the method of calculation (which was not a factor in their study) and the outcomes being considered (which was significantly different). Epic defines sepsis as presence of an ICD-10 code whose usage varies so much among hospitals that nearly nobody trusts it, including CDC and CMS, which don’t rely on the code to track sepsis or measure sepsis outcomes, respectively. The authors used the criteria that UM sepsis committee developed for quality measures tracking, which is a composite of the CDC and CMS definitions.
- Singh raises the possibility that Epic’s model may infer sepsis from the ordering of sepsis-related medications, with the model’s data “leakage” making it look better than it really is.
- Epic’s model identified only a tiny percentage of patients that clinicians would have otherwise missed.
- Singh concludes that UM is using the model as part of a broader sepsis intervention that includes frequent nursing checks, but will be revisiting the model’s usage.
- Singh’s recommendations to Epic, which he presented to its data science team in April, include releasing its models publicly for independent review as Cerner has done, increasing the transparency of the model’s coefficients and modeling code, and making it easier for Epic customers to run competing open models instead of limiting them to those offered by the company as “a walled-garden app store.”
Vanderbilt University Medical Center informatics professor and department chair Kevin Johnson, MD, MS posts “Living Through Going Live,” a video recap of VUMC’s 2017 go-live on Epic.
Sponsor Updates

- Newfire Global Partners offers its team members an interoffice exchange program, such as employees from its Ukraine office working and culture-exploring on Croatia.
- Users rate Halo Health the top clinical communication and collaboration platform in G2’s latest “Clinical Communication and Collaboration Grid Report.”
- Health Data Movers publishes a new client story, “Data Conversion for Oncology EHR to Epic.”
- InterSystems announces the latest release of its Iris data platform, which includes adaptive analytics capabilities and additional SQL extensions for analytics to improve the process of implementing an enterprise data fabric architecture.
- Jvion will present at the Home Care 100 Leadership Conference June 27-30 in Marco Island, FL.
- Ellkay joins the Active Archive Alliance.
- CHIME President and CEO Russ Branzell, MBA interviews National Coordinator Micky Tripathi, PhD, MPP at the summer forum.
- Nordic and the American Medical Association publish a white paper titled “2021 E/M Transition: How Organizations Are Moving Forward Successfully.”
- Mental health patients at Citizens Memorial Hospital have chosen virtual care via Meditech.
- Everest Group recognizes NTT Data as a Leader in its SAP Services PEAK Matrix Report.
Blog Posts
- Defining the Opportunity Window for Managing Blood Glucose Levels in Hospitalized COVID-19 Patients – And How to Meet It (Glytec)
- Turning Data Into Actionable Insight: How AI is Making a Difference (Healthcare Triangle)
- Observations of High-pressure and Rapid Shallow Breathing in Mechanically Ventilated COVID-19 Patients: An Interim Assessment (Capsule)
- How SOC 2 Type II Compliance Can Improve the Patient Experience (Loyal)
- Five Ways Activity-Based Costing Can Maximize Earnings (Health Catalyst)
- International considerations for digital health passes (Intelligent Medical Objects)
- The Evolution of Healthcare Delivery Models (Avtex)
- SIIM 2021 | Visage’s Top Five (Visage)
- Why Patient Engagement is Failing Us – And What You Should Do (Lumeon)
- 3 paths payers can take to actualize value from the CMS interoperability rules (Lyniate)
- How to Ensure a Healthy Relationship with Your Epic Community Connect Partner (Impact Advisors)
- Post-COVID Rural Healthcare Outlook with Alan Morgan, CEO of NRHA (Part 1) (Medhost)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.




As former CIO I am wondering if all of the billions (trillions?) spent on EMRs, etc have really improved care/outcomes. Based on the very simple measure of life expectancy I would so no (https://www.cdc.gov/nchs/data/hus/2019/004-508.pdf). I am sure that billing and documentation has improved and the industry has amassed warehouses full of data for interesting studies. I know that I will be critiqued for use life expectancy as the single measure but it is easily available and is a fundamental outcome. This should be embarrassing for a country that already had the highest cost and low life expectancy compared to other advanced economies (https://www.commonwealthfund.org/publications/issue-briefs/2020/jan/us-health-care-global-perspective-2019)
I think it cuts both ways. The #1 and #2 drivers of life expectancy in the US recently are COVID and opioids. I think EMRs have been a net positive in helping tackle both. That said, the ability to improve either COVID or the opiod epidemic also rests heavily on public policy. So I don’t know that it’s worth looking at life expectancy through the lens of EMR adoption.
Cost on the other hand…if anything EMRs are helping to drive the consolidation (and thus monopolization) of the healthcare market. EMRs give you the ability to do better operational consolidation, and better data that you can use to negotiate rates of your services. Both of these put upward pressure on costs. See: Sutter and their ability to drive up L&D costs. Is care better because of EMRs? Maybe? But the patients are certainly paying for every bit of it.
I said “costs”, but I should have said “prices”
Re: Epic defines sepsis as presence of an ICD-10 code whose usage varies so much among hospitals that nearly nobody trusts it, including CDC and CMS,
Therein lies the ‘big hole’ in applying AI in healthcare (or any other industry). It’s the old GIGO axiom. EMRs capture a ton of data but to much of that data is ‘gunk’. It’s primary reason for being coded and captured was/is administrative/financial, clinical research was never it’s original intent. Medical researchers were some of the biggest supporters of the ACA HiTech act thinking with the installation of EMRs across the country they could access a ocean of data and improve care and reduce costs. What they and the feds didn’t realize (or ignored) was that a good deal of the data is useless for valid medical research.
Unfortunately our medical data ocean is full of trash and cleaning it up and stratifying it will cost at least another $30 billion. Until then many of these AI tools will be nothing but academic math exercises.
OK, I get that. But the thing is, you need to look at this as stepwise improvement.
We got everyone using EMRs and ICD-10 codes. There is basic agreement on these foundation pieces. I think you’ll see, next, pressure to improve the data quality. That could take many forms and may very well take a lot of time. But every step forward brings the goal closer.
I read a lot of computer security articles. Know what the most common pattern to the exploits is? They start out as impractical hacks, then gradually they start getting easier to access. Here is the sequence:
1). An exploit is announced. It is incredibly difficult to use and most commonly, requires another successful hack to precede it’s use. Everyone is blasé about the new exploit because it’s so difficult to utilize;
2). A variation of the original exploit is announced. People start to take notice because this new variation, while still difficult to access, no longer has any prerequisites. Patching priorities are increased;
3). Multiple exploit variations are published. Some are actually incredibly easy to access! Meanwhile, “in-the-wild” attacks using the new variations start to appear. Patching is now urgent!
Finally, $30 billion? Let’s face it. Spread over the entire nation, this is actually not a lot of money. Especially considering how much healthcare already costs. Spread it out over 10 years and it’s just $3 billion a year. I’ll bet you could get people to pay this, to get standardized, high quality ICD-10 data.
You might even get healthcare savings sufficient to cover the costs.
We’ll be sure to add this to the long list of things people think we should be embarrassed as a country for.
I agree that mortality probably isn’t the best measure of EMR benefit. I also agree that having EMRs, e-prescribing, electronic transmission of lab results and vaccine receipt, and an ability to do a quick pívot to telehealth have all been very important in dealing with the pandemic.
I’m less convinced that quality of care has improved in general and don’t believe that documentation is improved (except for being legible). However, it’s hard to figure out because there are so many confounding factors that were introduced at about the same time. The meaningful use reporting requirements that have now morphed into MACRA have distracted from clinical care rather than genuinely improving anything. The same is true of a whole host of requirements for documentation and tracking of data imposed by CMS, Joint Commission, and others. And the CPT charting requirements are still cumbersome, unnecessary, and add nothing to the care of the patient.
Despite the hype associated with the “learning health system”, much of the data in the EMR is incomplete or inaccurate. This will become even worse with greater propagation of errors through more and more health records with the push for interoperability. As but one example, a family member still has benign prostatic hypertrophy (BPH) on his problem list and the first sentence of “identifying information” even though he had a prostatectomy more than 8 years ago and has told multiple physicians since then that they should correct this information.
Overall EMRs have probably had more benefits than negatives but it could have been and could be so much better if the focus was actually on delivering care and less of the regulatory and payment related impediments.
OK, so I see 2 errors here. I mean, it’s reasonable to expect some things from from EMRs, but I’m not sure that large benefits in metrics like life expectancy is reasonable.
What are the errors?
1). “Medicine is different.” Really? Why? Every other industrial sector has computerized, and massively so. It’s true that biology is complex, but this is a difference in degree and not in kind;
2). “We can continue providing healthcare with profit motives, patchwork systems, byzantine insurance polices, and no expense control (except for de-facto rationing of the under-insured).” No further comment required;
3). “Let’s ignore the primacy of Public Health in lifespans.” Nothing else matches large-scale Public Health measures, in increasing quality of life and lifespan. Nothing. Certainly not the EMR movement. Not infection prevention & control. Not chronic disease management. Not cutting-edge pharmaceuticals.
OK, that was 3 things, so sue me!
#3 is the key point. Only about 10% of life expectancy change comes from medical care. EHRs can be reasonably expected to only impact that 10%. And individual algorithms impact specific causes of mortality which represent a sub-fraction of that 10%. It’s not surprising that it doesn’t show up in a broad-brush measure like life expectancy!
Is it just me or was Bicycle Health’s page’s message a little to lighthearted for the serious nature that their business deals with?
Quote- Did Epic really think those factors were relevant, or was their data science knowledge insufficient?
WHAT Epic data science knowledge? They have any? Maybe in the clinicals, but in someething like this its non-existant, this was probably a customer request.