Yes! Flip flops are essential as the back up for professional footwear. Plus they are easy to put into your…
Monday Morning Update 6/8/20
Top News
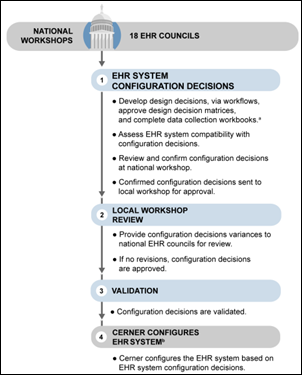
A GAO review finds that the VA has implemented effective configuration decision-making in its Cerner implementation by holding national workshops and creating 18 EHR councils, but needs to improve representation at local workshops.
The report also notes that while the VA and DoD both user Cerner, coordination is needed to allow sharing of information and tasks, such as VA’s requirement to maintain durable orders for life-sustaining treatment across patient encounters that is not supported by the DoD’s Cerner configuration.
Reader Comments
From Quinn Martin: “Re: rebranding. Why so hostile to the marketing folks?” That was Dr. Jayne, but I agree with her conclusion. Rebranding is admirable, but publicly pontificating about it and the process that went into it is not. Companies for some reason feel the need to yammer on in press releases about the naively aspirational big-picture ideas that led them to choose a particular website color or logo style (probably just to stroke the marketing people who dreamed it up) and the whole world just rolls its eyes. Just do it and let your audience react without trying to forcibly steer them to pre-conclude how wonderful it all is. My experience is that even though non-marketing company executives grudgingly go along with the process, they aren’t simultaneously committing to implement corporate change as part of the pig-lipsticking process, so it’s usually fluff anyway. Show, don’t tell.
From Creole Mustard: “Re: HIMSS. Pledges to stand against racial inequality.” I will provide a pro bono communication plan for this effort – publicly report how many people of color are on the HIMSS board and executive team, then ask vendor and provider organizations to do the same. I’ll recycle my advice from above – show, don’t tell.
From Didn’t Attend: “Re: HIMSS. Do you agree with Dr. Jayne’s assessment of HIMSS as greedy because they aren’t giving HIMSS20 refunds?” Not exactly. HIMSS was always about profit, highly paid executives, behaving like a vendor, and profitably commingling providers and vendors in a boat show environment that had little to do with patients or actual health. However, it clearly met a market need, as evidenced by its ever-increasing headcount and revenue. My take: I don’t think HIMSS is financially capable of providing HIMSS20 refunds even if it were inclined to do so, especially given the uncertainty of the conference industry in general, from which HIMSS generates $43 million of its $95 million in revenue. Imagine sitting around the HIMSS conference room table trying to plan HIMSS21 amidst the choking dust that remains from the implosion of HIMSS20. Where HIMSS needs to step up is in transparency and honesty instead of brandishing its force majeure clause in the faces of the members and exhibitors who express concerns – those members are really all it has left at this point. HIMSS20 was scheduled for just three months ago, so maybe they are still crafting strategy and exploring options, but I think the wounds are festering rather than healing. Now is the time to win us all back over. Other cancelled conferences seem to be doing a better job of managing the fallout, and while it’s probably unfair to compare leadership styles, I think former CEO Steve Lieber would have taken positive control of the narrative instead of creating a communications void that its critics are happy to fill.
HIStalk Announcements and Requests
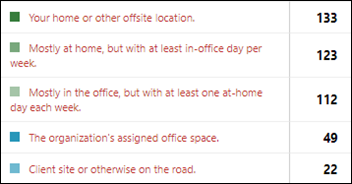
More than 80% of poll respondents prefer to work from home at least one day per week.
New poll to your right or here: Would you trust medical research findings that are based on analyzing the EHR data of hundreds of hospitals?
I celebrated the anniversary of the heroics of D-Day, now 76 years in the rear-view mirror, by reading “A Train Near Madgeburg,” a previously untold story of how Americans (mostly teenagers) of the 743rd Tank Battalion, which was one of three tank battalions that landed in the first wave on Omaha Beach, became the world’s first witnesses to the horrors of the Holocaust in April 1945. They rolled into Germany, and purely by serendipity, found and liberated a train full of 2,500 starving concentration camp prisoners who were minutes away from being exterminated to hide evidence of crimes against humanity to the the tune of millions of deaths. The author, a high school teacher, told the stories of those boys of long ago and those mostly women and children they saved, bringing them together in reunions at his school to provide their first-hand accounts. I was uncomfortable with the similarity of those 1933-1945 events to today’s headlines, but I was moved by the actions of one battle-fatigued, eight-man M5 light tank crew who, deep into Nazi Germany and surrounded by mostly hostile locals, were left alone overnight in their single light tank to guard the train’s occupants, who they assured were “under the protection of the United States Army.” Few books capture both the worst and best aspects of humanity like this one and the lessons it contains are worth careful study.
Webinars
June 10 (Wednesday) 1 ET. “COVID-19: preparing your OR for elective surgeries.” Sponsor: Intelligent Medical Objects. Presenters: Janice Kelly, MS, RN, president, AORN Syntegrity Inc.; David Bocanegra, RN, nurse informaticist, IMO. The presenters will cover the steps and guidelines that are needed for hospitals to resume performing elective surgeries and how healthcare information technology can optimize efficiencies and financial outcomes for the return of the OR.
June 18 (Thursday) 12:30 ET. “Understanding the ONC’s Final Rule: Using FHIR HL7 for Successful EHR Integrations.” Sponsor: Newfire Global Partners. Presenters: Bob Salitsky, healthcare IT expert, Newfire Global Partners; Jaya Plmanabhan, MS, healthcare data scientist. This fast-paced, 30-minute webinar will provide an overview of the Final Rule and describe how technology vendors, payers, and providers can use FHIR HL7 to deliver true interoperability. Attendees will learn how to define the data, technology, and flows needed for their EHR integration projects; how products can retrieve health information while meeting compliance regulations; and the benefit of adopting quickly to the future of data exchange while simplifying future integration efforts.
Acquisitions, Funding, Business, and Stock
NorthShore University HealthSystem completes a precision medicine program in which genetic data is loaded into ActX’s genomic service, then is used within Epic to alert medication ordering clinicians of potential genetics-related side effects, efficacy, or dosing considerations. Long-timers know ActX founder and CEO Andy Ury, MD, whose leadership history includes Physician Micro Systems and Practice Partner. In an unrelated note, whose “let’s just make up words” idea led to the grammatical abomination of “NorthShore” and “HealthSystem?” The CEO blabbered on in 2008 about how the former Evanston Northwestern Healthcare had “outgrown its name,” the “NorthShore” part communicates the all-important “prestige,” and the “brand equation” needed to include “University,” all of which were guaranteed to ensure “ushering in a new era.” I’m guessing the locals just call it “North Shore” anyway are are either indifferent to or annoyed by the impersonal “system” in the name.
Announcements and Implementations

Scripps Mercy Hospital San Diego is using Dexcom’s continuous glucose monitoring system for managing inpatient diabetics, including those with COVID-19 who would otherwise require finger sticks.
COVID-19
The government of Delhi, India files charges against a private hospital that failed to report its COVID-19 test results using the government’s mandatory reporting app. The chief minister also issued a warning to hospitals that he says are turning away COVID-19 patients to free up beds to sell on the black market.
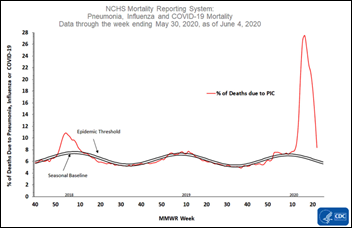
US combined deaths for pneumonia, influenza, and COVID-19 as a percentage of the total continue to taper off sharply, on track to return to pre-COVID levels. Total US coronavirus deaths are at 111,000, with the projection that has been most accurate over time predicting 190,000 deaths by September 1.
CMS acknowledges the wide discrepancy between its just-published data on COVID-19 cases in Virginia nursing homes with data from the state’s Department of Health. CMS reports that one nursing home has had 90 residents die of COVID-19 when in fact it has had zero deaths in zero confirmed cases. CMS also reports only nursing home information, while the state includes assisted living centers in its totals. The industry’s trade group says CDC’s slow approval of new accounts explains the 29 facilities that did not report at all. Virginia has refused to provided totals for specific nursing homes since the state defines corporations as “persons” whose confidential information cannot be published.
Sponsor Updates
- Pivot Point Consulting Managing Partner Rachel Marano joins Vaco’s latest Free Yourself podcast, “Flexing to the Curve in Healthcare IT.”
- PerfectServe recognizes customer St. Elizabeth Healthcare as its 2020 Healthcare Champion.
- The Late Late Show host James Corden will keynote Pure Storage’s Pure//Accelerate Digital event on June 10.
- Santa Rosa Consulting publishes a new case study featuring Berkshire Health Systems.
- Spirion welcomes new board members T.E.N. CEO Marci McCarthy and Fannie Mae Deputy General Counsel Jennifer Mailander.
Blog Posts
- A Real View: Supporting Northwell radiologists and the Javits center field hospital with innovation and infrastructure (Nuance)
- Don’t Miss Out on New MTM Opportunities (OmniSys)
- Rapid Radiology puts the focus on senior care (OpenText)
- Wake of the Floor: Enhancing Patient Engagement as we Emerge from the Shutdown (PCare)
- Newborns Don’t Defer Birth: A Clear Case to Better Equip L&D Clinicians (PeriGen)
- Your Future Revealed: Telehealth with PMD (PMD)
- Disrupt or Be Disrupted: Aligning with Independent Physicians Post-Pandemic (Premier)
- HR & Payroll’s Critical Role in Overcoming COVID-19 (ROI Healthcare Solutions)
- Your Workforce Has Changed, So Must Your Identity Strategy (SailPoint)
- 5 strategies to destressing IT teams in stressful times (StayWell)
- COVID-19 Revenue Recovery: Four Steps to Successful Program Launch (Strata Decision Technology)
- The Cost of an EHR Downtime (Summit Healthcare)
- How to Prepare for the Perfect Storm: Hurricane Season and COVID-19 (Surescripts)
- HonorHealth’s AVP Healthcare Marketing on Growth and Loyalty (SymphonyRM)
- End-of-Life Visitation with Safety and Compassion (Vocera)
- Culture After Crisis: How Clinics Must Evolve to Support Employees in the Coming Months (WebPT)
- A Leading Look at Revenue Integrity (Impact Advisors)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.


HIMSS: No communication or replies after multiple emails and messages left. The people in charge are terrible. No reply or even acknowledging is just down right unprofessional let alone disrespectful. They just want to keep the money without even acknowledging the small companies need for a refund. Just appalling.
I notice that in the email promoting this edition the NorthShore University HealthSystem “precision medicine” program was called “precious medicine” — a rather enjoyable Freudian slip?
I did even better once in mentioning a “marital arts competition.”
Is there a boot camp to prepare for that “marital arts” competition?
I’ve read here and in other publications over the course of the last three months what everyone thinks HIMSS needs to do to repair its relationship with its members both providers, vendors, and individuals. I been in healthcare tech for over 30 years, sat on the HIMSS board, and been a member until 2016 when I came to the decision that HIMSS only cares about three things, money, promoting its own agenda, and removing alternate opinions from the dialogue.
Until its membership and that of the vendor community wakes up and understands that those simple truths about what motivates HIMSS or its current leadership nothing will change. I agree with HIStalk that HIMSS more than likely cannot afford to refund the money it collected without digging deep into the leadership’s compensation and its political machine lobbing capital hill. It is my belief that its time to abandon HIMSS and allow it to either make it as a for-profit organization which is what it really is verse it hiding under the veil of a non-profit, which it hasn’t been for decades.
The educational aspects of HIMSS can be easily replaced by regional groups who can provide localized and national educational content by collaboration and by working with vendors who in lots of instances will pick up the costs. The vendors can form their own association with dues and hold an annual conference that they own, manage, and set the time and place. This would reduce costs all the way around facilitate greater transparency. Those are my thoughts and recommendations. I sate on both sides of the table and its time to rethink the real value of HIMSS.