Anything related to defense will need to go to Genesis.
Monday Morning Update 4/27/20
Top News
Epic CEO Judy Faulkner discusses possible post-coronavirus healthcare changes in a Business Insider interview:
- Some hospitals and medical practices will file bankruptcy, as she notes that Epic customers have reported revenue declines of up to 55%.
- Mergers, acquisitions, and layoffs are likely, especially as small providers are purchased by large health systems that have greater financial reserves.
- Video visits and at-home monitoring are here to stay.
- Public health surveillance and the associated standardized data requirements will be a focus.
Meanwhile, Epic offers customers COVID-related applications with no charge for licenses, implementation, and support during the pandemic:
- Bugsy Infection Control for infection tracing.
- MyChart Bedside for communicating with isolated patients.
- Remote Monitoring.
- Secure Chat.
- Transfer Center.
- Willow Inventory for tracking PPE.
- Rover for handheld nurse charting.
- Nurse Triage.
- MyChart, with no per-patient cost for new sign-ups.
HIStalk Announcements and Requests
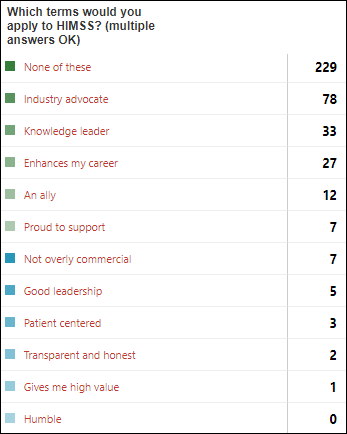
Poll respondents didn’t express a lot of positive thoughts about HIMSS, with transparency, value, and humility being the attributes they chose least often. I’m guessing that much of the ill will was caused by vendors and registrants who lost money from HIMSS20 refund decisions, but I also speculate that significant dissatisfaction and resentment has existed for years but has been masked by high HIMSS conference attendance numbers, which may have not been accompanied by any particular love or respect for HIMSS as an organization versus as an unavoidable vendor that runs the industry’s de facto gathering. Some respondents provided their own negative terms instead of choosing from the positive ones I listed. I doubt that any of us could come up with easy fixes, even if HIMSS were to agree that its past missteps require correction.
New poll to your right or here: Which types of virtual visit have you had since mid-March?
Listening: new from Delanila, moody, sultry alt pop fronted by composer Danielle Eva Schwob with the topical title of “It’s Been A While Since I Went Outside.” She filmed the official video (“visual poem”) herself in a COVID-emptied Manhattan. Her entire catalog under this name is just four singles, but all are magnificent and immediately addictive. I’m also enjoying the new, posthumously released single from Chicago rapper Juice WRLD, whose lyrics in “Righteous” (“taking medicine to fix all the damage”) foretold his drug overdose death in December 2019 at 21 years of age at Midway International Airport, when he downed of handfuls of pills to hide them from federal agents who were searching the private jet on which he was traveling (successfully, as it turned out) for the drugs and guns that were on board. Lastly, if you’re looking for a song that will burrow into your brain like toxoplasmosis, try “The Other Girl,” which sounds like Taylor Swift but is actually country pop singer Kelsea Ballerini with singer-songwriter Halsey (the latter’s first musical posting in 2012 was a parody of a Swift song, so there you go).
Webinars
April 28 (Tuesday) 1 ET: “COVID-19: Managing an evolving patient population with health information systems.” Sponsor: Intelligent Medical Objects. Presenters: Julie Glasgow, MD, clinical terminologist, IMO; Reeti Chauhan, senior product manager, IMO. IMO recently released new novel coronavirus descriptors to help clinicians accurately record diagnoses and also created free IMO Precision COVID-19 Sets to help identify and analyze patients with potential or documented infection. The presenters will discuss these new tools and describe how to use them optimally.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Vocera announces Q1 results: revenue up 15%, adjusted EPS –$0.14 vs. –$0.17, beating Wall Street expectations for both.
Amazon surveys its sellers about their health plans, creating speculation that it will offer health coverage.
Sales
- Tift Regional Medical Center (GA) goes live on LiveProcess Emergency Manager to power its virtual command center.
- Commonwealth of Massachusetts will offer free virtual visits to uninsured state residents who have COVID-19 symptoms or have been identified through contract tracing, powered by virtual care provider Doctor On Demand.
People

Eric Rose, MD (Intelligent Medical Objects) joins the VA’s Office of Health Informatics as chief terminologist.

New Jersey Innovation Institute hires Jennifer D’Angelo (Bergen New Bridge Medical Center) as VP/GM of healthcare.
Announcements and Implementations

In Australia, Queensland Health cancels its laboratory information system replacement contract with Sunquest after two years and having spent $24 million of the $43 million original contract award. It will instead upgrade its Auslab system that Sunquest was intended to replace.

Cerner offers health systems and researchers free access to the de-identified data of COVID-19 patients for developing epidemiological studies, clinical trials, and medical treatments.

Waystar launches an analytics and business intelligence module ahead of schedule to support the coronavirus-driven decisions healthcare organizations are making.
COVID-19
Researchers study the 14 available coronavirus antibody tests on which the hopes of reopening the US economy rest. Only three of the 14 tests — many of which are manufactured in China — delivered consistently reliable results, and none were perfect. All but one test sometimes gave false positive results (which could lead someone to think they are immune when they are not), the tests performed better when the patient had been infected for longer periods, and none of the tests have been approved or studied by the FDA. Meanwhile, an urgent care center near me is pitching COVID-19 testing for $40 cash plus the cost of the video visit, the latter of which is covered my many insurance plans for coronavirus screening. The unstated important point of all this is that (a) we have zero evidence that even correctly resulted seropositivity means that someone is immune, and (b) even if they are immune, we don’t know for how long. We could kill people by sending them back to work or causing them to throw coronavirus caution to the winds by assuming that past exposure indicates immunity. What we don’t know about this virus is nearly everything, except that it spreads and kills people with ruthless efficiency.
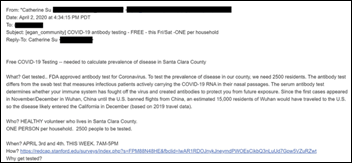
A Stanford seroprevalence study – which was was already being widely questioned for recruiting self-selected users via Facebook and going straight to a press release with no peer review — takes another hit when BuzzFeed News finds that the physician wife of the lead author recruited participants via a wealthy school’s listserv, skewing the demographics of participants. The preprint article estimated that up to 81,000 people are infected in Santa Clara County versus the officially reported 956, which would indicate a much lower death rate than previously believed. Another author is maverick Stanford researcher John Ioannidis, MD, DSc, of which an expert concludes may be “so attached to being the iconoclast that defies conventional wisdom that he’s unintentionally doing horrible science.” He and another of the paper’s authors had previously questioned in a Wall Street Journal op-ed piece and in several Fox News appearances whether the threat of COVID-19 is overblown.
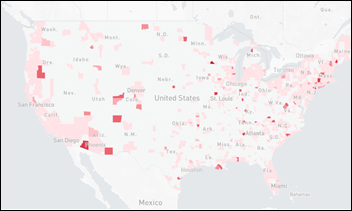
Facebook is offering users a coronavirus symptom survey that was created by Carnegie Mellon University, with results from 1 million users per week being sent directly to CMU for predicting disease spread and county-by-county impact. The first set of results will be published Monday. The map above indicates percentage of people with symptoms in each county (the redder, the worse), but I noticed that the symptom map allows showing percentage of people with symptoms by hospital referral region, which is useful in hospital planning (Rapid City, SD is about to get hammered).
US nursing homes have seen more than 10,000 deaths related to COVID-19, and nine of them that experienced coronavirus outbreaks that triggered “immediate jeopardy” federal citations were found to have significant problems meeting basic health standards – lack of PPE, failure to enforce physical distancing of residents, inadequate staffing, and failing to recognize and react to coronavirus symptoms. Routine federal inspection of nursing homes was stopped on March 20. They complain that federal help has been non-existent as hospitals received all the focus. More than half of reported COVID-19 deaths in some states were nursing home residents.
The Economist warns that governments are borrowing money at a level not seen since the end of World War II despite a dramatic drop in taxes collected, piling up coronavirus-related debt from issuing stimulus money and relief checks for people and businesses. The authors conclude that such spending is sensible in trying to forestall further economic slump — especially in the lower-risk US as the world’s reserve currency and with low interest rates — but working down the 1945 debt all over the world required high taxes on capital, the benefit of inflation, and a baby boom that was accompanied by higher levels of education. The authors also expect that the public — especially senior citizens who vote against politicians who attempt to limit entitlement spending — will demand higher levels of healthcare spending.
Former CMS Acting Administrator and United States of Care founder Andy Slavitt lists his takeaways after talking nearly non-stop to to scientists from all over the world:
- Making effective, breathable, and even fashionable masks available at low or no charge to the entire US population could protect us (at worst) or eradicate the virus (at best) due to the power of exponential math of the infection rate. Masks, rather than a vaccine or therapy, may be the silver bullet.
- We will solve the shortages of tests, ventilators, and hospital beds.
- Individual immune response rather than the strain of the virus may drive COVID-19 outcomes.
- Creating an effective vaccine by 2021, proving that it is safe, and then manufacturing and distributing it to the entire globe involves many challenges.
- Even in the absence of a vaccine, COVID-19 could be managed as a chronic disease.
- A vaccine may only be partially effective or may offer partial inoculation, in which case it could still be used in healthcare workers and high risk people.
- We need to produce so much PPE that a glut is created, taking profiteers out of the picture.
VA officials reverse their previous insistence that it is providing adequate PPE even as employees stated otherwise. VA Executive in Charge Richard Stone, MD says FEMA ordered the VA’s vendors to redirect its shipment of 5 million masks to FEMA for restocking the emergency stockpile, forcing the VA to limit employees who work directly with COVID-19 patients to one mask per day, while other employees who delivered food and medications to COVID wards received only one mask per week, with orders to staple the straps if they broke. The VA says that 1,900 of its own employees are sick with COVID-19 compared to the 6,300 infected veterans it has treated. The VA did not have enough tests for its employees until recent weeks, but its absenteeism rate is still tracking below the normal average at 4% as poorly equipped employees keep showing up for work.
White House officials are discussing plans to replace HHS Secretary Alex Azar, sources say, following widespread criticism of the federal government’s early response to the pandemic and misstatements to the White House about Azar’s reported demotion of HHS vaccine expert Rick Bright, PhD.
Other
Something triggered a memory of XG Health Solutions, the Geisinger analytics and consulting spinoff that was splashily introduced in 2015 without much buzz since, The company apparently closed its doors last summer (shutting down instead of selling out for even a “better than nothing” price is a key indicator of spectacular failure). I attended their HIMSS15 launch and concluded:
From the hallway conversations I heard and my own opinions, here are the positives: Geisinger has developed a lot of expertise and content that’s less ivory tower than most big academic medical centers, they put some thought into involving the patient in the use of their apps, and the SaaS-based subscription means new best practices can be put into place quickly. Negatives: the company has significant venture capital ownership (they aren’t Geisinger, in other words), you might suspect that Geisinger applied soft pressure to the newly named EHR vendor partners to get on board with uncertain future commitments, and so far they’re a company that hasn’t done much to dent the market other than to do Geisinger stuff and make announcements. Success in commercializing hospital software is elusive, and while Version 1.0 is easy, it’s Version 2.0 that gets ugly with upgrades, design decisions, and testing. The first non-Geisinger betas will be important.
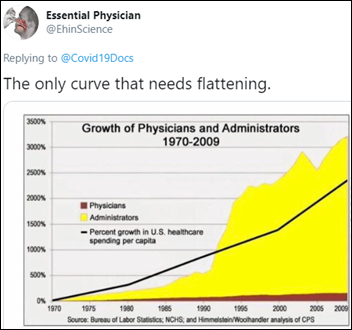
Best tweet of the weekend, although “other” would have been a lot more sarcastically effective and epidemiologically accurate than “only.”
Sponsor Updates
- Impact Advisors publishes a white paper titled “The Future of EHR Implementation Post-COVID.”
- Experian Health’s MyHealthDirect scheduling solution is now available in the Epic App Orchard.
- Health Catalyst makes COVID-19 insights derived from its Touchstone platform of 80 million de-identified patient records available to customers, hospitals, public health authorities, governments, and biopharma working on treatments.
- NextGate publishes a new white paper, “Why Patient Identity Management Tools are Critical for COVID-19 Surveillance.”
- KLAS includes Nordic solutions in its latest report, “COVID-19 Technology and Services Solutions Guide.”
- Clinical Computer Systems, developer of the Obix Perinatal Data System, releases the latest edition of its Critical Care Obstetrics Podcast, “Team Skills Simulation Training.”
- PerfectServe congratulates customer Prisma Health on FDA approval of its VESper ventilator expansion device.
- Experity will host a virtual job fair May 2 from 9am-noon CT.
- Patient engagement vendor Relatient joins the Epic App Orchard.
- ROI Healthcare Solutions announces comprehensive EDI optimization offerings for Info users.
- Summit Healthcare publishes the “Galway Clinic Success Story: Solving Complex Interoperability Needs with the Latest in Integration Technology.”
- In Europe, Synteract leverages the TriNetX platform and COVID-19 Rapid Response Network to find and enroll patients for coronavirus clinical trials.
Blog Posts
- Why health IT matters: Not on the front lines of COVID-19, but not on the sidelines either (Spok)
- Maximizing Annual Wellness Visits with Telehealth in COVID-19 (Lightbeam Health Solutions)
- Quickly Find and Share COVID-19 Resources Across Your Healthcare Coalition or Health System (LiveProcess)
- Financial Strategies for the Post COVID-19 Recovery (Loyale Healthcare)
- Amid crisis, hospitals provide communities with mental and emotional support (Meditech)
- The Biggest Barriers to Healthcare Interoperability (Health Catalyst)
- Charles Corfield’s COVID-19 Weekly Assessment (NVoq)
- Three ways automation can help weather the storm of uncompensated care (Experian Health)
- How Healthcare Providers Can Deliver the Best Online Payment Experience During Challenging Times (PatientBond)
- Why E-Notifications Matter More Than Ever (PatientPing)
- Beyond HIPAA-Compliant Texting: Top Healthcare Communications Solutions (PatientKeeper)
- Week 2 WFHighlights & Pointers: Heart-Warming Stories & Success as a WFH Parent (Pivot Point Consulting)
- Virtual Visits vs. Zoom – The Era of Telehealth (QliqSoft)
- Digital Tools Prove Essential to the Revenue Cycle During COVID-19, Will be Key to Recovering After (Relatient)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.





If MDs want to improve the ratio of physicians to administrators, maybe they should pressure their colleagues to open more US medical schools.
Among the things that have changed with the emergence of covid-19 is the number of Epic generated press releases. Have there been more this year than all of previously recorded time?
Epic being seen doing good, may be good for Epic and the world.
The sad truth of PR is that you need to embellish. Once you start to embellish, it does not take much to go down the slippery slope and lose credibility. Time will tell.
“What we don’t know about this virus is nearly everything, except that it spreads and kills people with ruthless efficiency.”
With a death rate that is trending to be between .25 and .5 percent when this is all said and done, I’m not sure how this rings true.
Could not agree more on XG. Was involved in an xG Epic implementation with Catholic Health Services on Long Island. They spent 100’s of thousands on a bunch of Clinical decision support protocols that could not be used out of the box because of different configuration philosophies. Needed to redo all of them to adapt to local build.
Judy is stretching the truth while describing the use of CareCompanion at Cleveland Clinic. 1001 patients using CareCompanion will qualify for thousands of patients. But according the the folks leading the initiative at CCF, actual utilization is sub 30%.
I see 2 people disliked the comment. Is it a shortcoming of the platform or did you genuinely dislike the post? Scenarios:
A) I am an Epic lover and I don’t like this company being bashed. So I am disliking the post/author.
B) I don’t like falsehood. So I am disliking Judy stretching the truth.
C) I think sub 30% adoption is great and the post demeans that achievement. So I am disliking the post/author.
D) I work at the hospital (Cleveland) and know that we have over 80% utilization. So I am disliking the post/author.
Red’s my favorite color
Thanks for an honest answer. Do you happen to know if the claim (<30%) made is correct or not?
Media squelching is a term for repressing positions on social media that differ from the party line, by the partisan leadership of those platforms. Let me stipulate: COVID-19 is dangerous and we need to take steps. We also have to be sane about the steps we do take.
What is interesting is how the virus went from a nothing burger in early Feb to nearly shutting down the world in less than a month, and the irrational actions of a lot of the population because they are scared (TP hoarding etc). Based solely on “modeling” that hugely missed the mark by 1600% (that is original 1.7 million US deaths now projected to be <100K, a change in less than 6 weeks), and we shut down our economy on that error.
And not knowing all the key ways it spreads or just how fatal it is if contracted. Because we don't have the denominators, which are key to knowing any of the rates. Exacerbated because the only people approved for COVID testing have to have symptoms, so no total population stats are known. New data is coming in on the head counts of those with antibodies who never reported sick, which provides hope this isn't as bad as we are led to believe and that the death rate is greatly lower across the population than modeled.
And the urgency is bolstered by CDC's original instructions on coding U07.1 as being the underlying cause for any death when present (or suspected if no testing done) with co-morbitidities and end stage conditions. NY is getting excoriated because they forced nursing homes to take hospital discharges of patients with COVID, which resulted in double digit deaths in those locations, because they are filled with the at risk elderly. And it also adds to the death count numbers that probably would not have occurred. These types of factors inflate the actual COVID death rate, but even then, it is coming in quite low (most stats now are showing actual death percentage under 2% and most don't even achieve 1% of everyone who gets it.)
Then we have those with other agendas latching onto this as a way of control. I won't go there except to point to the draconian and petty things – such as filling skate parks in CA with sand so teens can't skate.
So when the views of the leadership of the major social media platforms aligns with one point of view on this topic, we get media squelching of anything that does not align. This is a very dangerous thing to let happen.
I do not know the accuracy of reports by Dr. Ioannidis as I don't have his data. But will say that it aligns with other investigator's reports I've seen. This only means there are two sides to this – and reality is somewhere in the middle. My fear is that we are wrecking not only our economy but will eventually collapse our healthcare infrastructure because of this lengthy operational shutdown – as said above in this HIStalk edition. Both sides should be heard – but on platforms that let challenges and pushback to the findings (of either side) be aired.
I hope Mr. H will let this post. And I am open to hear from anyone who sees it differently.
I’m not sure what your point is here other than you feel like your view isn’t getting heard on social media platforms.
With regards to the model accuracy I see the situation as similar to the Y2K bug from 20 years ago. It was a huge sensation in popular media, and everyone was all hyped up about it. Every major software company spent time developing and pushing out patches to their code to make it “Y2K compliant.” And then Jan 1 2000 happened, and … noting. It was a non-event. People were quick to complain about the hype, but it’s not that Y2K was never a risk, but rather it was avoided because people took steps to prevent it.
It’s the same with COVID. It’s not that the models in Feb were mountains made of molehills, it’s that we as a society took drastic steps to prevent those models from being reality. Emotionally, it’s easy to look back and say “maybe the steps didn’t need to be as drastic as they were” but analytically we know that it’s because the steps were so drastic that this thing was contained so well.