Healthcare data sucks - that song turned my Friday to Friyay!!! Gave me the much needed boost to get through…
Neal Patterson’s Final CHC Speech – November 16, 2016

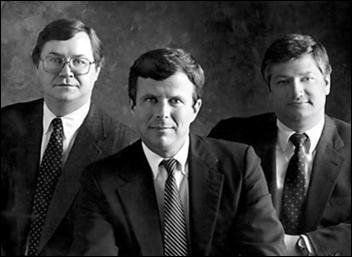

Cerner Chairman, CEO, and co-founder Neal Patterson made a surprise appearance – one that would would turn out to be his last — at the Cerner Health Conference on November 16, 2016. Patterson had been diagnosed with cancer in January 2016. He died less than eight months after his CHC talk on July 9, 2017 of cancer complications. He was 67 years old. His wife Jeanne – who was Cerner’s seventh employee and who suggested the company’s name – died of longstanding metastatic breast cancer less than two months later at 59.
I recently received a recording of Patterson’s remarks and am running them on this second anniversary of his death.
This time last year, I gave this talk on this stage. At that time, I knew something was going on. I think it was New Year’s Eve when I got the call about the biopsy that said I had cancer. For me standing here, the previous talk [by David Feinberg, MD, then CEO of Geisinger Health System] was incredibly relevant to me as the patient.
I think about caring and the inherent trust you have with your provider. You are at their mercy. You’re there because you trust their competency, but the caring is not always there. You can tell when people are in a hurry or when they are behind schedule.
Dr. Feinberg is the leader of possibly one of the most important parts of healthcare in the next decade. A lot of other things are going to happen in the next decade. Data is going to be there. We are going to be right at the center of it. What we do collectively is going to change fundamental platforms. Cognitive computing — or whatever the term ends up being — systems are going to make good physicians, good nurses, and good technicians better. But most importantly, they will change the experience that we have as patients.
I have quite a few stories that I could tell about my cancer treatment experience. It wasn’t exactly that I was bored, but I did pretty much spend eight months in a rabbit hole, going through a series of treatments that had brutal effects. You have a lot of time to be a patient inside the facility getting the treatments, and then you have quite a bit of time to reflect on the consequences of those treatments.
I have figured out that God has a sense of humor because he put me at a place where the provider was going through an EMR conversion. [note: Patterson didn’t name the institution, but it was almost certainly MD Anderson, which was undergoing a conversion to Epic at the time]. I know he did it on purpose. Only one or two of us really deserve to go through one, and I have done mine, OK? [laughs, clearly joking about Epic CEO Judy Faulkner] It wasn’t a Cerner conversion, but I’m sure anything I say has also happened in a Cerner environment. Here’s a couple of stories from that.
This was a high-quality, high-prestige organization. It was one you would pick from the list if you had cancer. I went for my chemo treatment one day and they sent me to the big transfusion room. I hated that room because it was always going to take a lot longer.
I had been in the waiting room for four hours waiting to get assigned a room to get a transfusion. Few who know me well would believe this statement, but I had patience, because there was a lot of complexity and a lot of stuff floating around. But after four hours, I went through the door that I wasn’t supposed to go through, into the triage room.
They said, “We can’t get you a room because we haven’t got this lab test done yet. Your doctor didn’t order it.” I said, “I am most certain that he did.” They said they hadn’t received the results.
I said, “Here’s what I’m going to do. I going to stand here until you get the results. The only way I’ll leave is if you send me to a stat lab, which will get the results in 10 minutes, and I’ll be back with those results. This doesn’t need to happen.”
Sure enough, they got somebody in the laboratory who promised they would stay on the line until they got the result. Then I got a room assigned and started the process of transfusions that can last four hours.
I forgot to tell you. Many of you have heard me speak before. I was always a terrible speaker, but one of the negative outcomes of my treatments was my speech. My assistant Elaine whispers in my ear, “Talk slow. Try to finish the words.” I don’t know If I’m talking slowly or finishing anything.
Anyway, I got to my room. A lady who was there I first arrived was still there. I asked her how she was doing. She said it had been a terrible day. I asked how long she had been there. She said seven hours. [Patterson stopped speaking for several seconds to compose himself after an emotional reaction]. There’s no caring in that.
The message for us, and what I think is the reason that God sent me here, is that most of that was probably due to the system conversion and changing procedures. We in the room need to anticipate those things to minimize the impacts, because they are big impacts.
Let me do one more quick story. I could tell that the cancer center was quite proud of their laboratory. They have a big lab. I was impressed, but the big lab waiting room was just cram-packed full. Always full. I went back to get my test and they were doing positive ID, running your patient ID, and confirming that the test order is in the lab system. It was taking 10 minutes for this handshake to work.
I knew which third-party system was on the other side. While I was waiting through my 10-minute turnaround, I asked the tech, “How long does it usually take? It should only take like 10 seconds, but it has been taking 10 minutes.” I picked up the phone while I was waiting, since I was stuck anyway, and I called. I got it fixed pretty fast. I don’t think anybody in the whole place even knew they had the problem. They had enough problems they were chasing and they weren’t chasing that one. I fixed that one overnight, so I was proud of that.
There are two stages of being a patient. I took it as a project. Once I got the diagnosis, there was a problem and I was going to solve it. You have to make a series of decisions, such as where to get treatment. Then you get your strategy of how you’re going to approach it. Finally, you get a plan and go execute it. I was familiar and comfortable with that part.
With the kind of stuff I had, you don’t have “a doctor.” You have four major doctors.
- You have the doctor who will cut a bunch of stuff out. I was in surgery for 15 hours, so they were working on something pretty hard.
- Then you have the surgeon who tries to make you look something like you looked before. He’s a pretty important factor to you. He’s trying to put you back together.
- Then you have the radiation oncologist, who is going to basically fry you by putting you in the oven and cooking you every day. I had proton-beam radiation, although I never did understand whether it’s actually better.
- Then you end up with your medical oncologist, who is a really important doc, too.
That’s a team, but it is very hard to be part of that team. I would score my team pretty high on the team list, but it wasn’t hard to find things where they did not work together as a team. They are busy as all get-out and you are in one space at a time.
You’ve built the team and the plan and you’re going to go execute the plan. But there’s that other side, where you are actually having it done to you. That’s where you can feel the caring.
What’s really cool about healthcare is that the people you encounter are almost always caring. It’s usually the way systems are designed, leadership, or other factors such as workload that create the distractions that reduce that feeling of caring on our side.
With that, there are a couple of elephants in the room. One is, what is my plan?
This is a great diet. I lost 70 pounds. Thirty of that I enjoyed taking off, maybe even 40 of it, but the last 30 pounds was basically strength. I’m kind of in shock now. I look like I’ve come out of a prisoner-of-war camp. You lose a lot of strength.
At this stage, I’m at the end of the treatments. I received very good news. The surgeon who was going to do the voodoo stuff said to me at the beginning, “I’m going to cure you.” The first thing I asked him when I woke up was, “Did you cure me?”
He got an A. That team got an A. But I think all of you know that with a disease like this, it’s five years before you feel good about what the next checkup is going to find.
With all the treatments I had, I have issues. If I’m out eating with somebody, they’ll say, “Neal has a few issues we’ll have to accommodate here.” But I’m in a mode of getting stronger and getting better daily, which is a great place to be.
I will be back at Cerner in basically my capacity probably in January. But the reality is that I’m going to make some changes. Before we had the last board meeting, I had my assistant look at my time over the last three years. I spent almost a full day in the air flying each week, that is, in the airplane and off the ground. That doesn’t count the time getting and from to the airport. So one of the things I’m going to have to adjust is that I’m not going to be everywhere I have been. You’re going to see me less at your site, and the converse is that Cerner will see me more.
My last comment is about our industry. We’ve been through the digitization phase of healthcare, and most of it was automating processes. Many times, the automation of processes could have been done better. Too many times, we were automating the old process.
What we are going to do as a company is to double the productivity of physicians. The EMR is central to their work and it will increase their productivity. We’re going to do the same thing with nurses and many technologists.
But one thing that I’m saying here today that I wouldn’t have said a year ago is that we’re going to make being a patient a different experience, too. It’s just not the freaking portal, if you don’t mind my language. The patient portal was a nice step, but for the patient to be part of the team, it has to be part of the team. The portal cannot just be a source of information. We’re going to be part of a team, we’re going to make us part of the team, and then we’re going to make it easier to care for us.
Thank you for being here. Thanks for the opportunity. What I have gotten to do over the last 35-40 years has been a privilege. There’s an awful lot left to be done and we are going to go do it. Thank you very much.


This was very touching and inspiring. Thank you for sharing. Many of us think of Neal Patterson as a cut-throat billionaire health care tycoon, but this is a very one-dimensional view. He really did make the world a better place. No matter if you are a diehard Epic person or a Meditech fanatic, you must step back an appreciate this man. The intense rivalry among EHR venders made Epic, All Scripts, Meditech and the others to push their limits to give providers the tools save lives, make patients healthier, and standardize processes. The health care industry would not been the same if it weren’t for Neal and his life’s work. His legacy reaches beyond Cerner. It’s deep within the clients, competitors, and his many protégés.
R.I.P. Mr. Patterson.