Giving a patient medications in the ER, having them pop positive on a test, and then withholding further medications because…
Monday Morning Update 8/27/12
From Siemens Surfer Dude: “Re: Mark Zielazinski, CIO of Alameda County Medical Center. An e-mail was distributed to ACMC staff last week saying he’s leaving with no details. They’re in the middle of an Invision to Soarian implementation scheduled for go-live on CPOE this fall.” Verified. Mark says he’s moving on to Marin General Hospital to rejoin his old El Camino Hospital boss Lee Domanico, who is now CEO at MGH. They’re building a replacement hospital and Mark will have some related additional responsibilities beyond IT, telecomm, HIM, and biomed. As far as ACMC goes, Mark says the Siemens / NextGen rollout is going fine and ACMC is getting its ARRA money. Both organizations will make announcements about his new job sometime this week.
We would expect that an EHR technology developer could satisfy § 170.523(k)(1)(iii) by disclosing: 1) the type(s) of additional cost; and 2) to what the cost is attributed. In reference to the first example above, an EHR technology might state that “an additional ongoing fee may apply to implement XYZ online patient service.” In situations where the same types of cost apply to different services, listing each as part of one sentence would be acceptable, such as “a one-time fee is required to establish interfaces for reporting to immunization registries, cancer registries, and public health agencies.
From Frank Poggio: “Re: MU Stage 2 zinger. Buried back on Page 405 is a real ditty, Price Transparency. Looks like in spite of all the flaming comments ONC received from vendors on the draft of this idea, they are moving ahead with it. ONC backed off requiring vendors to publish a specific price list, but now mandates that they list out all component, install, training, interface, third party and other costs. At this rate, I predict in Stage 3 they will ask for the numbers. Also, in the new certification rules, ONC estimates that it will cost vendors $195 million. If you take the 816 vendors certified under Stage 1 and then reduce the $195 million by ONC’s $60 million annual budget, that means each vendor will spend $165,000 to revise and certify their software for Stage 2. Who will eventually pay, and would that money be better spent elsewhere?”
From Sagacity: “Re: MU Stage 2. For the pleasure of your readers, the bookmarked and cross-linked versions of the Stage 2 and Certification Criteria rules. Save to the same folder with the original names and the cross-linking will work.” Thanks for that.
From Luminosity: “Re: authors. You should get more people to write instead of just giving space to a few guest authors.” Everybody is welcome to submit Readers Write articles as long as they meet my requirements for length, quality, and non-promotional topics. Being invited as an ongoing contributor to HIStalk is another matter – I’m not desperate for content, so I would expect folks to be way better than average. Regulars like Ed Marx, Dr. Rick, and others have an interesting and credible perspective, state it well, are entertaining as well as informative, and are diligent enough to keep it up month after month. Writing is like teaching – everybody thinks they could do it perfectly because really talented folks make it look easy. Anyone who thinks they have the right stuff and can send me a sample article along with ideas for their ongoing series and we’ll see where it goes. That’s the limiting factor on whose articles you’ll see here, not my unwillingness to give someone else a platform.
Welcome to new HIStalk Platinum Sponsor Sandlot Solutions. The Fort Worth, TX company, which is uniquely jointly owned by Santa Rosa Consulting and North Texas Specialty Physicians (NTSP), offers a platform that turns data into information. NTSP is a pioneer ACO (one of only 32, also named one of eight ACOs to watch including its use of Sandlot Solutions by Information Week) with 2.5 million patients. They know how to connect providers with critical information. Sandlot Solutions offers a next generation HIE and analytics system that uses low-cost cloud computing to connect physicians across all care settings and practice locations to improve care and reduce costs. The underlying products include Connect (HIE and master patient index); Dimensions (data warehouse); Metrix (analytics); and Care Manager (caregiver workflow driven by near real-time clinical and claims data). If you’re in the market for HIE software, check their no-nonsense evaluation checklist. The company’s leadership team has some familiar names, including that of our own “From the Investor’s Chair” Ben Rooks as an advisor. Thanks to Sandlot Solutions for supporting my work.
Now that I’ve talked about Sandlot Solutions, let’s have a short demo (which I found by cruising YouTube).
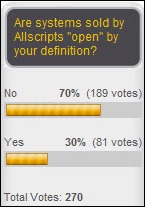
Allscripts says its systems are open, but 70% of poll respondents say really aren’t, at least by their definition of the term (the thoughtful comments are worth reading). New poll to your right: is your reaction to the announcement of the Meaningful Use Stage 2 rules positive, negative, or indifferent? Once you’ve voted, click on the Comments link in the survey box (or click here) and explain your opinion.
From that last poll, a comment by Limber Lob was particularly thoughtful given his obvious knowledge of several vendor EMR products:
Whether Allscripts is "open" centers on the definition of the term "open." "Open" conjures up notions of "open source" or at least multiple read/write APIs for a system, but it also reminds us of the important related concept of "extensible systems." An extensible software system is one that can be "extended" by someone other than the original developer AND in the programming language in which the system was written. It isn’t widely realized that three of the four successful long-lived integrated EHRs (with single patient database) are extensible by this definition. The VA VistA’s programming Standards & Conventions (SACs) allowed the extension of VistA over the years by VA sites nationwide, with — for example — the Puget Sound VA developing VistA’s Provider Order Entry (POE) system, and the Topeka VA writing VistA’s Bar Code Medication Administration (BCMA) module. VistA’s extensibility under the VA’s Decentralized Hospital Computer Program (DHCP) of the 1980s and 1990s is a principal reason why VistA now has more than 100 major sub-systems and an estimated 125,000 function points. Cerner’s EHR can be extended using Cerner Command Language (CCL), which is a proprietary "scripting language" in which as much as a quarter of the Cerner EHR’s logic is written. Many Cerner sites employ multiple CCL programmers, and books on CCL are available from Amazon. And perhaps surprising to many, Epic’s EHR is also extensible by Epic customers, as Epic makes source code and documentation available so that customer organizations can develop name-spaced code and data structures that extend Epic’s functionality in a manner similar to Epic’s customizations of their system for their clients. Epic encourages customers to use the other mechanisms for enhancing the functionality of the Epic EHR, but they also support what they term "free range programmers" in their customers’ organizations. Meditech, the fourth of the long-lived integrated EHR systems, has a closed code base. Finally, Allscripts’ supports extension of their Sunrise environment using a package called ObjectsPlus that has a reputation for being hard to use, and requires highly skilled and expensive programmers — which makes it an impractical proposition for many Sunrise customers.
I must have received half a dozen breathless “Breaking News” e-mails at work Friday screaming that HHS had delayed ICD-10 implementation until 2014. I’m not sure why this news was earth-shattering given that HHS itself proposed the extension in early April. Were the rags expecting some other outcome, or did they just forget that this is old news?
Here’s a new book on healthcare business intelligence. The folks involved sent me a Kindle copy, but I haven’t had time for more than a quick skim so far. Amazon has the Look Inside! feature turned on, so you can peruse the table of contents and quite a few sample pages. The author is Laura B. Madsen, who works for BI vendor Lancet Software.
In England, Lewisham Healthcare NHS Trust chooses Cerner Millennium for electronic patient records, its first UK win since it jointly bid to Royal Berkshire along with UPMC in 2009. InterSystems and Cambio were the other finalists and iSoft is the incumbent.
Also in England, Buckinghamshire Healthcare NHS Trust admits that a software problem prevented the parents of some children from receiving their follow-up vaccination notices. The trust took over the vaccination program a year ago, but some parents were sent multiple reminder letters while others received none. A trust spokesperson said other customers of the unnamed software may also have been affected.
In another item from England, the county of Herefordshire, trying to determine why only 3% of its residents received an invitation to be checked for serious disease vs. the 20% target set by the government, find that a software problem may be responsible. A doctor tells them that the screening software only works with the Google Chrome browser, while the county-side medical system is not compatible with Chrome, forcing doctors to print out their entries and then re-enter them manually on two dedicated computers.
The Meaningful Use Stage 2 Webinar offered by NeHC and ONC on Friday filled up quickly. They’ve added sessions for Tuesday and Thursday at 12 noon Eastern, or you can view Friday’s recorded session or download the slides.
Researchers working with data from hospitalized HIV patient create a predictive model to estimate the chances of readmission within 30 days and death, using only EMR information from the first two days of their admission.
Keynote speakers at New York eHealth Collaborative’s October 15-16 conference at Pier Sixty in New York City: David Brailer, chairman of Health Evolution Partners, and Stephen Dubner, author of Freakonomics. Several dozen other speakers will grace the lectern. Receiving career achievement awards in health IT at the event’s gala will be Jeff Immelt of GE and Sam Palmisano of IBM. General registration is $395, licensed healthcare professionals and government employees get a $195 rate, and students get in for $100. The gala runs an extra $750. Rooms at the Hilton New York Fashion District are $319. HIStalk sponsors who are sponsoring this event include Optum, Emdeon, NextGen, and Nuance.
Tom Carson, founder and former president CEO of MD-IT until January of this year, is named CEO of Axion Health, which sells employee and occupational health software.
ZirMed names Kenneth Willman (WellPoint) as VP of payer solutions and strategy.
The University of Toledo Medical Center announced last week that it had temporarily suspended its live donor program and suspended two nurses after unspecified human error forced surgeons to abort a planned transplant while both patients (a male donor and his sister, who was the intended recipient) were in the OR. The university provided more information Saturday: the human error was that a nurse put the donor’s kidney in the trash, ruining it.
Doctors in Ontario complain in a town hall meeting about changes in their fee codes, intended to reduce costs by $340 million but making it impossible for physicians to bill for certain services. An interventional cardiologist says doctors are now paid only $2.50 for reviewing an ECG, with the rationale being that computers are doing all the work, leading her to say, “I’d like to think I’m better than a computer. I feel disrespected and disillusioned.”
Vince takes a short HIS-tory break to memorialize industry long-timer Dick Schopp, who died earlier this month.









ONC systematically ignored detailed feedback from many vendors on the cost to modify (I won’t say upgrade because that implies better) their systems.
165,000.00 per system? That barely buys you one capable programmer with benefits and everyone knows it. And, there is way more work in there than one programmer would be able to do on their own in a year.
What about QA, Documentation, User Centered Design, all the Interfaces, the release packaging, etc.?
This is a bold and intentional misrepresentation and it should be pointed out.
They are off by a factor of 10 or more and the feedback they received consistently pointed that out.
Frank,
Who will pay? The answer is obvious. The patients and taxpayers, but not the shareholders, unless they are patients.
With the government mandate, these devices are going to be purchased regardless of the costs. Which vendor will sell the most?
The one that actually produces devices that improve efficiency of care, improves outcomes, and reduces costs.
So far, all vendors’ devices get an F in those three categories.
Computer interpretation of EKGs: “An interventional cardiologist says doctors are now paid only $2.50 for reviewing an ECG, with the rationale being that computers are doing all the work, leading her to say, “I’d like to think I’m better than a computer”
In the United States, the FDA has not revetted the accuracy of the computer reads of EKGs for many years.
I as a nurse, depend on these reads, but, it is well known that most of these auto-read systems think atrial fibrillation is sinus rhythm (and vice versa) and are meaningfully useless (and dangerous) with supraventricular tachycardias and with rhythms involving pacemakers.
Many patients get the wrong treatments because of erroneous computer generated EKG interpretations.
To say your poll about the Open question for Allscripts is open-ended would be the understatement of the year. The ability to hook into the Allscripts platform (or many others for that matter) has been in place for years, that is nothing new. And the ObjectsPlus code set, or any from Cerner or Epic, are necessary to keep some level of control in the hands of the vendor, otherwise you are opening Pandora’s box. And when you buy software, part of the expense is developers to help you use it better, no matter what the language.
How about polling what health systems are going to do to help NORMALIZE their data? When Allscripts-Eclipsys merged, it was going to be a sexy sell to say they were able to bridge Sunrise and Enterprise data together. Guess what, a lot harder than it looks.
Why? Because data normalization DOES NOT exist in most health systems. RxNorm vs. Multum for medications. Med Allergies that have different definitions between inpatient/outpatient settings. These interpretations and cross-mappings take time and are not sexy to talk about. Why do most hospitals struggle at med reconciliation? Same reason. My Tylenol is not your Tylenol.
“Open” communication between disparate systems is n its infancy and an ACO/ICO/Value-Based system is going to require a level of normalcy we have not seen yet. At least Allscripts is seeing the forest through the trees in this department, regardless of what “Open” actually means.
Independent – data normalization has existed in most all clinical laboratories since the early 1900’s. The clinical laboratory has generated for decades the largest volume of healthcare data. The problem is that many of the other vertical silos in the “healthcare system” have not followed suit.
This is a role that the CIO could help solve from a leadership perspective…
Best,
Don
On costs to change EHRs to comply with ONC’s world view…
Typical government approach – exaggerate the benefits while misrepresenting the costs.
Keith,
I basically agree with you as to who ultimately will pay. But the feds actually believe the providers will pay first. Here’s why. Back in 2009 when the Obama administration first proposed the idea of an MU program with bonuses and test criteria and a bureaucracy to support it they said “if we spend $30 billion on EMRs we will save $800 billion in healthcare costs”. That’s a 26 to 1 payback. In my 35+ years working in profit and not-for-profit business I have never seen a 26 to 1 ROI anywhere.
So round about next year, after the election, when the feds have to come face to face with 14 trillion dollar deficit, and healthcare making up 17% of it, I fully expect to hear this from Congress: “Hey providers, we gave you $30 billion and now we’ve come to collect the ROI you promised” (Remember AHA/HIMSS and AMA supported ARRA!). Guess what will happen next? OUCH!
Yes Frank,
There was a gaping hole in the concept that HIT would be the financial foundation for covering the costs of PPACA. I see your point.
HIT has failed to deliver on outcomes and cost reduction. There have been years of experience in innumerable hospitals. All I see are higher profits for the non profits, higher salaries for the corner suites, and some truly horrific deaths and care screw-ups
that one would not have expected to have occurred with the proclaimed safety of HIT.
Funny that neither side in the big erection have pointed out that HIT has not delivered and will likely not deliver the goods expected for paying for PPACA.
HIT/EHR “ROI”??? Bwaaahahaha!
Only systems that provided ROI were the hospital billing and finance systems in the 60’s.
This MU mambo jombo is one big govt bubble.
Where would Obamas buddies Jeff Immelt and Glen Tilman be without it huh?
Everyone’s drinking kool aid.
I have only seen ROI when there is extensive Clinical Transformation adapting a new workflow around a new tool in the clinicians hands. Why is it that when so many EMRs are installed, there isn’t any clinical change like there is when a health system buys anything else that goes into a clinician’s hands? It makes no sense why an EMR has to be squeezed into the old paper process of doing things.
It’s a tool, but if you don’t use it the right way, it’s no better than what it was without it. Common sense applies that automating more of your bottlenecks would create better outcomes…but it’s just not occurring in most EMR implementations.
Typical Government, your government bias is showing. Yes, I know you weren’t trying to hide it.
But I must ask, why not uniformly apply standards to organizations both public and private? From what I’ve seen, the exaggeration of benefits and misrepresentation of costs is common in all organizations that retain a marketing department.
PezMan says:
Why is it that when so many EMRs are installed, there isn’t any clinical change like there is when a health system buys anything else that goes into a clinician’s hands?
Can you give some examples of the “anything else” and the clinical changes that occur?