Giving a patient medications in the ER, having them pop positive on a test, and then withholding further medications because…
Monday Morning Update 7/2/12
From Hellcare: “Re: ACA. Interesting reader responses. You have collected many devoted readers and contributors with varied backgrounds, experience levels, and opinions over the past few years. What about an open forum week, in addition to your regular articles, where we discuss, ‘What is wrong with the healthcare system and how do we repair it?’ Who knows, maybe we’ll do better than Congress! I don’t think that it even needs to be a dissection of the ACA, but maybe opinions from more than just C-level management that have to give the answers they have to give to save their jobs. If Ell Jeffe is right, then there is much to discuss and even better, more to learn.” I’m game. To keep it positive instead of everybody just complaining, tell me what you’d change and why. Also, operate under the assumption that we aren’t going to simply throw out today’s healthcare system, so your changes should be realistic. Anyone want to start us off?
From Pliny: “Re: mobile apps. The FDA says they are subject to its oversight if they process user input with a formula or algorithm, output a treatment recommendation, or perform a calculation that results in an index or score. That would cover any mobile app that connects to an ARRA-certified product, would it not?” Good question. I interpret it as meaning the logic is running from the mobile device itself, which wouldn’t be the case with most clinical system front ends that are just displaying data and capturing input, no different than a Citrix session. Anybody else want to chime in?
From The PACS Designer:”Re: Apple’s 7-inch iPad? With the launch of Google’s $199, 7-inch tablet called Nexus, can Apple be next with a 7-inch iPad? Earlier this year, such rumors were swirling about a mini iPad that would make a better fit in lab jacket pockets, so we may see it in 2013 at a price of around $300.”

From DrLyle: “Re: AMDIS meeting. About 300 attendees, mainly CMIOs and similar, about 50% more than last year. Some great discussions from both academics and applied informaticians, with topics such as problem list management, ACOs and population health, EMR usability, analytics, and role of the CMIO.” Presentations from the AMDIS 21st PCC Symposium are here. Above is a DrLyle photo from the meeting last week in California.
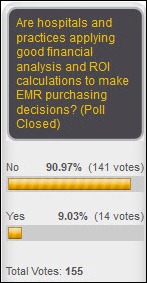
A surprising 91% of readers say hospitals and practices aren’t using sound financial principles when they decide to buy their clinical systems. New poll to your right: what’s your professional and personal reaction to the Supreme Court’s decision that Obamacare (as both parties now call it) will stand as law?
From the above poll results, here’s my challenge to CIOs of hospital that are spending $100 million or more on an inpatient clinical system. Readers are skeptical that your employer did its due diligence on return on investment. Explain to them why they are right or wrong (e-mail me a paragraph or two – I will leave you anonymous unless you indicate otherwise.) How did your organization justify the expense and what’s being measured to prove that the decision was a good one? Or if you made your investment and went live more than a year or two ago, how do the benefits you’re seeing (both financial and non-financial) compare to what you expected?
I haven’t followed the PPACA drama all that closely, but here are the healthcare IT ramifications I would expect judging from what I’ve heard here and there.
- The majority of people and companies who paid little attention to PPACA under the assumption that some or all of it would be found unconstitutional will have to scramble to catch up. Few expected it to survive unscathed, so they wasted the first couple of years after it became law in March 2010 when they could have been figuring out what it means to them.
- More people will have access to insurance, so hospitals theoretically won’t see as much self-pay and bad debt. However, they will need even more people and systems to handle all of those insurance transactions.
- A fly in the ointment, however, is that employers may decide that the penalty for not providing insurance is cheaper than actually buying it with their significant employee subsidies, so they may just drop coverage entirely and force employees into the open market via health insurance exchanges. Employees may make the same choice, especially in PPACA’s early years, when penalties for not carrying medical insurance are minimal (just a few hundred dollars per year). Real-time eligibility checking and a plan to collect patient responsibility upfront will be required for provider survival.
- States have made poor progress in developing health insurance exchanges, so they probably won’t be ready any time soon.
- Medicaid rolls will swell massively under the plan, so providers will need to watch their reimbursement rates and payor mix carefully, especially since states are already teetering financially and now have another headache to deal with.
- With 30 million newly insured citizens and a shortage of primary care providers, the pressure will be on to improve PCP efficiency (even if just to restore the time EMR usage has stolen).
- Platforms that provide the ability to schedule PCP visits against their open schedules will be in demand to even out supply and demand based on provider and location.
- Given the likelihood that PCPs will still be overloaded, I would expect more care to be delivered by extenders and telemedicine, which will change the expectation of the systems in use.
- The demand for provider information will be insatiable. The same federal government and insurance companies that require endless petabytes of questionably useful information will now want even more of it once the promise of cost reductions isn’t realized. They are even more in charge of providers now than they were previously.
- Medical device vendors can’t be happy since PPACA requires them to start paying an annual 2.3% tax on gross revenues starting in January.
- PPACA’s impact on cost will probably be to increase it. In that regard, the biggest problem has still not been addressed since the special interests would have killed the bill otherwise – the healthcare system, regardless of who’s paying, is bloated, inefficient, and run by those special interests (including the biggest special interest of all, politicians.)
Investor reaction to the Supreme Court’s decision: shares of hospital chains and healthcare IT vendors are mostly up, insurance company shares are down. Allscripts was up 8% on the week, while Quality Systems, McKesson, and Cerner jumped around 4%, a little better than the S&P 500. Athenahealth was up, but only by 1%. Cerner’s market cap is up to $14 billion, with Neal Patterson holding $462 million worth.
Not getting your HIStalk e-mail updates? Here are two solutions: (a) sign up for them if you haven’t already (duh), and (b) add mlsend.com to your so-called whitelist of e-mails allowed to get through your spam filter (your e-mail administrator will probably need to do this). I changed the e-mail service a few weeks back, so if you aren’t getting the e-mails all of a sudden, go with option B and tell your e-mail person that mlsend.com e-mails aren’t spam.
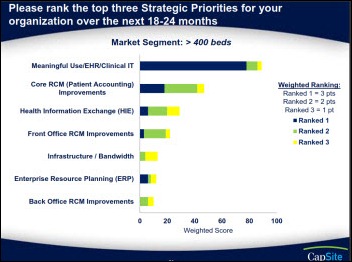
CapSite releases its Revenue Cycle Management study, which finds that 21% of hospitals plan to replace their RCM solution in the next to years and 53% say they will upgrade what they have. Interestingly, the larger the hospital, the more likely they are to replace or upgrade their RCM. The most-desired bolt-on solution is patient insurance eligibility verification, although 400+ bed hospitals are more interested in kiosks and the most-planned purchase of all is coding solutions. I was also interested in a relatively minor stat from the extensive report – in 400+ bed hospitals that responded, the #1 registration/ADT vendor (as a proxy to overall system penetration in my mind) was Epic, followed by Siemens, Cerner, and GE. I also liked the strategic priority question above.
The non-profit Patient-Centered Outcomes Research Institute (PCORI) is hosting the National Workshop to Advance the Use of Electronic Data in Patient-Centered Outcomes Research this week in Palo Alto, CA. Assuming it’s a bit late to plan attendance in person since they just sent me the announcement, they’ll have a live webcast (July 2-3). Speakers include folks from PCORI, Stanford, UCSD, NIH, FDA, and other big organizations. I hadn’t heard of most of the speakers, but those whose names I recognize are Doug Fridsma (ONC) and Paul Tang (PAMF).
Medical image management vendor UltraLinq offers Cardiac Accreditation Accuracy, software that allows users to track their QA documentation and statistics through integration with its exam data.
The PACS Designer is updating his list of iPhone apps, so if you’ve run across any that are interesting, post a comment to tell him about them.
CTG announces four new contracts for outsourcing, business process re-engineering, IT medical management, and HIE implementation support.
A jury returns a $15 million verdict against Springhill Memorial Hospital (AL) for a 2008 incident in which a 45-year-old non-ventilated patient died after bypass surgery due to an overdose of the anesthesia drug propofol that was administered by a nurse working her first shift in the cardiac recovery unit. The nurse was found to have no documentation of training appropriate to her assignment, had no experience in working with cardiac recovery patients or propofol, and failed to call for help when the patient lapsed into an immediate coma. Afterward, the nurse changed her documentation of the patient’s vital signs and ventilator settings, then erased the IV pump’s memory and destroyed the propofol container.
Vince’s HIS-tory this week covers HMS, tracking down co-founder John Doss for a first-person account.
Wall-mounted entertainment consoles are being removed from South Australia hospital patient rooms after at least four patients are harmed by units falling off the wall. Plans to install 3,500 of the units were cancelled.
Strange: a journal article chronicles the case of a 24-year-old software engineer from India who experienced an intense headache every time he tried to watch pornography, forcing him to change his plans. The authors didn’t figure out what caused the headaches, but they successfully treated the patient by advising him to pre-medicate himself with ibuprofen and acetaminophen.




“•With 30 million newly insured citizens and a shortage of primary care providers, the pressure will be on to improve PCP efficiency (even if just to restore the time EMR usage has stolen).”
I am pleased to see that you recognize that EMR usage reduces cost effectiveness of doctors’ time. Considering the impediments posed by meaningfully unusable EMR systems, it is unlikely that PCP efficency will improve.
Make use of the leap second and take joy in the fact that the earth is spinning more slowly.
Re: Transforming Health Care
Doctors are not receiving any incentives to provide the right care at the right time for the individual patient. Most doctors know how to practice economically without rationing care. The current and proposed incentives are perverse. Both independent doctors and contracted doctors in ACOs or hospital networks are pressured to over order, or ration, depending on the venue. $ billions could be saved if the doctors were to receive a cut in the savings by each, on average, if they reduced the global expenditures from their orders by ordering right for the patient. There is so much unnecessary surgery being done that could be delayed or avoided, polypharmacy cases with medicine caused diseases, and now huge inefficiencies caused by EMRs and CPOE systems that run up the bill. Bottom line: pay doctors to provide cost effective care by having them share in the savings of $ billions accomplished by their efficiency.
Carol Thomas, MD – thank you for a great intro on a huge problem and possible repair. If providers are being pressured to over order or rations services of care; yet, i they were given the ability to practice medicine as they trained to do, then we might find a huge chunk of savings. The problems seems to lie with the ACO or hospital network. Are they willing to change their way of thinking? Can they and still stay in business and finally, will they? I’ve worked with enoug providers to know that they don’t want or appreciate anyone telling them how to practice medicine; but, they haev to stand together.
@Hellcare – ACO’s were actually introduced to allow for shared savings, contrary to the rant that you find so enlightening…
@Mr. Histalk – things are slightly more complex in several areas that you mention:
– if employers decide to stop providing health insurance for their employees, in addition to the penalties, they must also take into account the loss of tax benefits they would continue to get if they provide insurance.
– It is unlikely that you will see 32 million of the uninsured (the official estimate) suddenly get health insurance overnight; that process will probably take a few years
– If the states are not ready with their exchanges by 2014, the federal government will run it for them.
Regarding apps, users of the Versus Real-time Locating System (RTLS) can download our free app to display location information on their iPhone or iPad.
http://itunes.apple.com/us/app/versus-evm/id414955095?mt=8
Jeanne,
Thanks for the tip on Versus EVM, I’ll add for the next TPD’s List update.
TPD!