I believe it is this: https://www.investopedia.com/terms/w/warrant.asp So an option, but one provided by the original company.
Monday Morning Update 10/17/11
From Epic4All: “Re: Epic. It’s the de facto EHR for hospitals in Seattle with two more area community hospitals implementing it – Overlake and Valley General Medical. This is on top of the largest system Swedish Medical Center (and associated hospitals), UW, and Group Health already live.” Unverified. Your statement will probably elicit scathing comments from the same handful of high-strung readers who howl that any mention of Epic is pandering favorably to the company, conveniently missing the point that they are outselling everyone (not to mention that I run quite a few negative comments about Epic as well.) I’d bet money that anyone who gets that worked up at the mention of Epic either (a) works for a struggling competitor, or (b) applied to work for Epic and got turned down (or both). I suppose I could write endlessly about Invision or STAR, but who would find that relevant or interesting?
From Soliloquy: “Re: Epic. Heard that one of the Adventist facilities on the West Coast is stopping its ambulatory implementation and will put out an official announcement next week. Someone also told me that Ventura County is walking away from Epic at their two public hospitals.” Unverified.
From Another Take: “Re: Fasttrack’s comments on Cerner Health Conference. This consultant writeup is favorable, but seems to be without bias. I found it an interesting juxtaposition.” Most interesting to me was that Neal Patterson compared Cerner to Apple, which seems a stretch given the implementation challenges and user-visible complexity of Millennium, Cerner’s unwavering focus on investors instead of innovation, and emphasis on enterprises instead of individual users. I’d say Cerner is a lot more like Microsoft, Oracle, or IBM in that regard, but Neal’s obviously looking to ride some Apple coattails (or perhaps is badly hiding some Steve envy). That doesn’t detract from what Cerner has accomplished, but drawing a self-comparison of a conservative enterprise software vendor to the consumer-focused and innovative Apple is always going to cause some eyes to roll.
Thanks to HIStalk reader Jared, who sent me an iTunes gift certificate with a note of thanks for HIStalk. He wasn’t looking for a plug, but I’ll give him one anyway since it was a nice surprise – he’s the founder of Splint, which is building EMR client iPhone apps for nurses (of which he is one.)
Armed with a bulging iTunes balance courtesy of Jared, I decided to see if I could find an interesting iPad app or two for HIStalk readers. The result: Splashtop Remote Desktop, one of the coolest things I’ve seen lately (especially for $1.99). Load the app on your iPad or iPhone, install the free streamer app on the PC you want to control, and you’re done – the app finds your PC and you can instantly start controlling it just like you were sitting in front of it. Not only is the video fast and smooth, the PC’s sound even plays over the iPad’s speakers (!!) I sat outside on the deck with a snack and fired up Word, ran my Iolo System Mechanic registry backup, closed down my invoicing program that I’d forgotten was open, and streamed some Flash video that normally doesn’t work on iPad. It looked exactly like the video above. You can run your desktop apps from anywhere, send files to yourself that you forgot to take along, run Office apps or Outlook without having anything installed on your iPad or iPhone, and maybe even do work-related IT geeky stuff like remote into servers, launch non-Web enabled apps, and do inside-the-firewall stuff from anywhere (by using remote desktop). That’s pretty amazing if you ask me.
I must be getting cranky since I keeping coming up with new grammatical pet peeves, but here’s an HIT-specific one: calling an enterprise-wide implementation of Cerner, Epic, VistA, Meditech an EHR (“The hospital is installing Epic’s EHR.”) I really dislike the non-specific term EHR in general since it describes the end result (stored patient information) and not the applications that create or view that information (CPOE, medical device interfaces, imaging systems, etc.), but it’s really a stretch to use the term EHR to include patient-irrelevant applications such as revenue cycle, supply chain, and workforce management that are often part of the same enterprise-wide implementation. The Feds got everybody throwing around the term EHR to make the same old EMRs of yesteryear sound more appealing, but the tried and true terms made more sense because they were specific: PM/EMR, clinical systems, order entry, etc.
Listening: new from reader-recommended Mayer Hawthorne, a young white nerd from Michigan who shockingly sounds exactly like a 1970s Motown / Philadelphia soul act with high vocals, horns, strings, and funky bass (Stylistics, Cornelius Brothers & Sister Rose, Billy Paul). Here he is on my new fave music show, Live from Daryl’s House. Super catchy, fresh, and retro. He does a great job on Private Eyes with Daryl Hall on the video. This is another chance for those folks stuck in a post-college musical rut (AC/DC in drive time, anyone?) to listen to something recorded in this millennium — think of it as a gateway drug to music that your parents didn’t listen to.
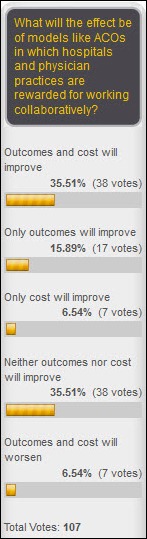
Readers aren’t quite sure how ACOs will affect quality and cost, with the number of those who predict both will improve being exactly offset by those who say both will get worse. New poll to your right: should HITECH compensate providers for using EHRs they bought before the program started? (I didn’t forget that I don’t like the term EHRs, but I used it since we’re talking HITECH here.)
Thanks to the following sponsors (new and renewing) that supported HIStalk, HIStalk Practice, and HIStalk Mobile in September. Click a logo for more information.
My Time Capsule editorial this week, stretching its legs after being filed away since 2006: Don’t Look Now, Your Loop is Open. An excerpt: “We bought the technology least likely to be used, that addresses errors least likely to be harmful, that doesn’t help the user who needs it most, and deployed it in patient care areas where serious errors are least likely to occur.”
RIS/PACS vendor Candelis gets FDA 510(k) clearance for its cloud-based diagnostic image routing and sharing tools.
A SIS-sponsored survey finds that 43% of anesthesia providers either use or will implement an anesthesia information management system, with 28% planning to evaluate systems in the next year.
Ohio State University Medical Center was scheduled to go live on its $102 million Epic system early this past Saturday morning.
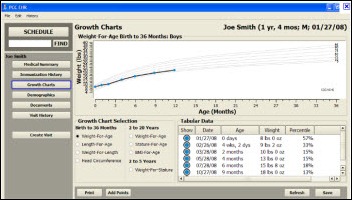
Physician’s Computer Company earns ONC-ATCB certification for its pediatrics-specific PCC-EHR v6.0.
Virginia Tech researchers develop software that limits smart phone access to data to specifically defined locations, then wipes it clean when the phone leaves that area. It can also limit smart phone functionality by location, such as shutting down cameras and e-mail when phones are in a hospital operating room.
Awarepoint and Meditech collaborate to develop an ED offering that allows locating patients and tracking critical milestones in real time from the Meditech system. Monongahela Valley Hospital (PA) is its first user.
Florida’s doctor-shopping database finally Monday morning. It’s not perfect, however: pharmacies can wait up to seven days to update it with prescription records, its use is optional for doctors and pharmacies, and most of its potential users don’t know it’s coming online. I was talking to a rural GP who uses an interesting approach to weed out his many drug-seeking patients: he gives them a quick urine screen every time they visit. If they show use of marijuana, cocaine, or other illegal drugs, he shows them the door immediately. He also sends them packing if they have excessive levels of their prescribed drug (indicating abuse) or zero levels (indicating that they’re selling the drug instead of using it). Not surprisingly, the vast majority of his abusing patients are on Medicaid.
Kansas City-based hospital chain HMC/CAH files for Chapter 11 bankruptcy protection, with its biggest creditor being software vendor CPSI at $1.2 million owed.
Bill Wallace, a retired SVP of IT of BCBS Kansas, is named CEO of Kansas Health Information Exchange Inc., the organization’s first employee.
A personal injury law firm’s press release says it settled a wrongful death lawsuit against Northwestern Memorial Hospital (IL) for $5 million, where a 55-year-old physician patient died after a nurse gave him insulin despite a doctor’s order saying it should not be administered. The law firm deposed a nurse who said she had contacted hospital administrators several times to complain about high workload and inadequate staffing. The law firm manages to squeeze in a jab against the medical profession, saying “it is both tragic and ironic that this type of obvious error would happen to a physician in this age of physicians protesting malpractice claims.”









Since Epic has been the lead story for a few of your posts, let it be known that Epic is the vendor to Northwestern Memorial Hospital, the subject of your last news item: “55-year-old physician patient died after a nurse gave him insulin despite a doctor’s order saying it should not be administered”.
Should this not be considered an adverse event associated with user unfriendly EMRs? Should not such deaths be eliminated by EHRs and CPOE? Just surmising.
EMRs will never be user-friendly enough to make up for someone who is careless. We do not have enough data to blame the error on Epic. More likely, in my opinion, is a careless or overworked nurse who didn’t read the error carefully enough.
I agree with you, Suzy. Bravo! A true systems error! Doc still gets sued, and likely nurse too. Pity really,we have immature EMR’s, which is in all honesty where we are at, so far as comparatively trying to map human thinking and replicating that with an EMR, and as a result the silo-ed options available in EMR’s drastically reduce the complete order intent. Even the best EMR out there is still immature! We are still comparing them on one scale of immaturity! Some less some more, but all immature!! An analogy would be comparing the clinical history taken by a physician from a patient by direct interview. Traditionally, in an era seemingly gone by, this would be written or transcribed in a great deal of detail, drawing on the vast array of explanatory words the English language has to offer, and the result telling a fairly detailed story of the sequence of events leading to the hospitalization. But, in stark and tragic contrast today, the best of EMR technology has thrown ‘templated’ histories at us as a solution to time inefficiencies.
That solution loses a tremendous amount of important detail some of which can have life-threatening consequences if not acted on.
So, something in the EMR led to that patients death , that could have been prevented had he had a paper chart. WAIT, did I hear that right? If only he had a PAPER CHART, he may have lived!! So try telling this to the senators and legislators that enacted the ARRA/HITECH ‘fix-it-al’l. OF course we are not going back, but we have to do a better job, and we do need to hold the EMR accountable, and legislators need to perhaps evaluate their timelines. The push for compliance is still a PUSH. Generally a push leads to a fall. We need the authority to slow down implementations and to insist government quit pushing when safety is an issue.
This concern seemingly has fallen on deaf ears and a number of us have understood that the result of such errors, likely to increase, are litigation trophies waiting to be swooped up by the legal profession, much of which is well represented in congress, and so one profession seemingly benefits tremendously from this immaturity, and it AIN’T us!!
We really need legal reform.
Neil –
I’m not sure where to begin with the rambling and semi-comprehensible entry, but as a former provider, I think you’re foolish if you think EMRs somehow introduce a risk that didn’t exist with paper charts. In my experience, paper is just as likely (or even much more likely) to be misinterpreted by a caregiver. As in all things, I don’t think blaming the tools is as good as finding out why someone was careless.
Somehow a press release from a law firm turned into another troll fest. Epic is not “the vendor” at Northwestern Memorial Hospital, they may be at a physician group affiliated with NMH, not sure about the details, but the hospital itself uses other vendors.
What is even more ridiculous, is that there is no indication that the order not to give insulin was even electronic – it might very well have been a peace of paper that got lost in the chart.
True, Duh, very likely human ‘carelessness’ involved, but we are implementing ‘tools’ to prevent that. My statement stands: our tools are still immature and need to do a better job….this one got through!
(And just so we don’t make this site become like YouTube with ‘hate’ comments, Duh’s comments on my ‘ramblings’ are taken in the spirit of collaboration, for one common good….the safety of the patient! Thanks!)
Some good reading on this topic for y’all, if you want (may help you understand where my concerns/’ramblings’ lie as an actively practicing provider embedded in the EHR implementation:
‘Medical Malpractice Liability in the Age of Electronic Health Records’, NEJM 363;21: 2060 – 2067
‘Hidden Malpractice dangers in EMR’s’, Response to above article by Steven I.Kern, Esq. former New Jersey Deputy Attorney General assigned to the State Board of Medical Examiners
‘Meaningful Use of Information Technology: A Local Perspective’, Annals of Internal Medicine. 2011;154: 690-692
I do not know if there is an organization that only tests EHR products and there patient safety profile, similar for instance to ISMP for medications? Anyone?
The interview at NMH solves the mystery. The argument that the order may have been on paper is a belly laugher.
http://www.healthcare-informatics.com/ME2/dirmod.asp?sid=&nm=&type=Publishing&mod=Publications%3A%3AArticle&mid=8F3A7027421841978F18BE895F87F791&tier=4&id=0FD7A5E3CF5A42E994CC76661C7EA69D
Dale Sanders is vice president and CIO of the Chicago-based
Northwestern Medical Faculty Foundation at Northwestern University,
affiliated with 897-bed Northwestern Memorial Hospital. He recently
spoke with Healthcare Informatics Senior Editor Daphne Lawrence.
DL: Who do you have?
DS: We have Epic on the ambulatory side and Cerner on the inpatient
side.
re the unverified note about Jack Evans leaving Dell – Jack now shows his current role as SVP of Enterprise Services at ettain group on his LinkedIn account…..
Gina…great post, especially as I read on:
http://www.healthcare-informatics.com/ME2/dirmod.asp?sid=&nm=&type=Publishing&mod=Publications%3A%3AArticle&mid=8F3A7027421841978F18BE895F87F791&tier=4&id=0FD7A5E3CF5A42E994CC76661C7EA69D
DS: Most of the care that we think is affected by personalized
medicine we think will be on the outpatient side. Eventually we will figure out a way to display this content back through the Cerner user interface as well.
DL: Are you working with anyone on this or is it all in-house?
DS: We did this all internally with our own staff.
DL: And Epic works with you on it, right?
DS: I’ll be honest with you. Epic is not very supportive of it, and I’m not that happy with Epic’s overall support for open application programming interfaces and open services. I’ve brought this up to Judy and her team — you’ve got to open the API, you’ve got to become more services oriented and you have to make it easier to blend non-Epic content in the user interface. They’re slow to support that model as compared more open architectures like eClinical Works.
DL: So why are you using Epic?
DS: Epic is embedded here and has been for 10 years. We’re going to offer eClinical works for the private physicians as part of the Stark laws umbrella. If you open the API, you’ve got zillions of programmers that can write cool applications against that, and it makes your product more attractive, not less attractive.