Neither of those sound like good news for Oracle Health. After the lofty proclamations of the last couple years. still…
News 11/17/10
From HIPAA Police: “Re: spelling. You would think a group sending a mass e-mail pitching its market research services would spell HIPAA correctly.” You would indeed.
From Limber Lob: “Re: getting physicians to standardize processes. Princeton economist Uwe Reinhardt says that trying to get physicians to work together is like trying to get eagles to fly in formation.” I like that analogy a lot.
From Capone’s Vault: “Re: Motion Computing Mobile Clinical Assistant C5V. This is slick. The pressure will be on the iPad to match the healthcare-friendly features of this.” It’s a full tablet with a docking station, optional barcode scanner, camera, Gorilla glass breakage resistance, and hot-swap batteries. It weighs three pounds, can be disinfected, and can withstand drops (big thumbs down to the iPad in that regard). Sounds great, just a little bit expensive at the mid-$2,000 range, but IT-friendly. Motion was bad about not getting enough nurse input on their previous models, so I’ll withhold judgment until I heard from nurses who have used a C5V at the bedside.
From Randy: “Re: Connected for Health review. I am enrolled in a Health Systems Management class at Morehead State University. This book is required reading.” I’m glad to hear that – I bet its great for that. Another reader is using it in an informatics course for public health students they’re teaching. For those who don’t know, Morehead State is in eastern Kentucky. I went to a seminar at St. Claire Regional Medical Center once, which is how I knew. Thanks for the report.
From Duke Nukem: “Re: NEJM article saying doctors should beat hospitals to the punch in forming their own ACOs to protect their own interests. Harrumph – you mean the same way they protect themselves by walling off nurse practitioners and claiming medical expertise is required to deliver acupuncture? A hundred years ago, they were barely better trained than barbers and butchers.”
Microsoft says its genomic sequencing project with Seattle Children’s Hospital consumed $18,000 worth of cloud-based supercomputing resources compared to the $3 million it would have cost using traditional local hardware. It used the Windows Azure cloud computing platform.
Wake Forest University Baptist Medical Center is going Epic, I’m told.
Nuesoft’s IT and product groups throw down a pretty good Lady Gaga video spoof. It sounds a lot like her and many other singers today, i.e. heavy on the Auto-Tune, which I really dislike — think Cher’s Believe from 1998, which sounds kind of Peter Framptony like somebody’s singing into a keyboard (meaning you don’t really have to be able to carry a tune to be a “singer” with computer-perfect pitch – it just came a few years too late for Milli Vanilli, but in plenty of time for the cast of Glee). But I digress – it’s a pretty good video.
A former Fallon Clinic (MA) doctor brags on the clinic’s EMR, but complains that his access to it was terminated when he left to join another clinic. His point: he can’t treat patients as effectively who have chosen to move with him since “their” information is being held captive by Fallon Clinic, who says they’ll mail him a CD in a few weeks. I think it’s a bit presumptuous to assume that his former employer will continue to let him use their systems and I assume the CD they’re sending will have the information about his patients in some standard format he can review. Beyond that, that’s why there are HIEs (other than to get federal money).
The OncoEMR oncology EMR by Altos Solutions becomes the first oncology-specific EMR to receive ONC-ATCB certification as a complete EHR, the company says.
Patient Privacy Rights releases an informed consent white paper and the results of a new patient privacy poll. The rags are picking up the poll result as big news since it finds that 90% of Americans want to be able to decide who can see and use their health information, but I should add a cautionary counterpoint that the questions were loaded with what the ever-witty Inga always calls bias of the “Do you like babies and puppies?” variety. For example: it asked lay people whether providers should be able to “share or sell your sensitive health information without your consent” and “Who should make the decision on whether corporations and researchers can see and use the information in your health records without your permission?” I don’t know how far that skewed the percentages that ended up in the 90s, but I’d say quite a bit. Still, I don’t doubt the conclusions, just the methodology. I’d also guess that quite a lot of Americans would divulge just about anything for cash (like those Brits and their passwords a couple of years ago), so maybe that’s the backup plan for those profiting from their data – just buy it from them and mark it up.
Stanford Hospital runs a pilot project in which cath and angiography patients are given iPads preloaded with movies, books, games, and Internet access to entertain themselves before and after their procedures. The hospital likes the idea because TV installation was going to be a pain.
Inga did her usual bang-up job with the latest installment in her ongoing Vendor Executive Series on HIStalk Practice. She asked 14 top executives to comment on a recent survey that found that about half of physicians in private practice expect their EMR vendor to help them qualify for Meaningful Use money. It’s always fun to compare and contrast their answers.
McKesson CEO John Hammergren comes in at #10 in the list of the highest-paid CEOs of publicly traded companies, bringing home $24.5 million in total compensation for the year ending September 30. The company declined to comment.
Vocera acquires two Tennessee hospital communications companies: Clinical Health Communications and Integrated Voice Solutions. Guille Cruze, founder of White Stone Group that spun off Clinical Health Communications, will run both organizations as a Vocera VP in charge of handoff communications products like the ones offered by those two vendors. I interviewed him back in January 2008. The companies have 30 employees and 150 hospital customers between them.
Bill Gates says robots will be the next big technology. Maybe he’s right: check out the Actroid-F from Japan, which the developing company will market to provide social services such as those delivered by hospitals. I creeped myself out when I realized that I was thinking that she’s pretty cute. I bet I’m not the first.
Healthcare is the #3 enterprise user of iPads, trailing only financial services and the tech sector.
Maybe the iPad will rank higher in healthcare in Australia, where Victorian Premier John Brumby promises that every state hospital doctor will be given an iPad if his party is re-elected. He says $12 million will cover it, but he seems vague about exactly what’s going to be running on those devices that will give doctors “easy access to time-critical clinical information,” not to mention who’s going to support them.
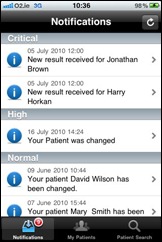
In the UK, Portsmouth Hospitals NHS Trust wins a patient safety award for co-developing a PDA vital signs capture application.
Odd lawsuit: a prisoner serving 10 years for running over and killing a teenager on a bicycle while going 83 in a 45 mph zone is suing the dead teen’s parents, who he claims were negligent in allowing the dead teen to ride his bike without a helmet. He wants compensation for his “great mental and emotional pain and suffering.”
HERtalk by Inga
UPMC says it will add 815 new full-time jobs, including up to 80 in IT. This announcement came following the release of UPMC’s first quarter financials, in which operating revenues grew by $77 million to $2.1 billion and profit increased $28 million to $93 million from July through October. The health system is on track to spend about $500 million on capital improvements this year, including about $100 million on its EMR implementation.
Former Sentillion and Microsoft executive Rick Dean moves to Humedica as VP of provider sales.
KLAS introduces an RSNA Resource Center that features several radiology-focused KLAS reports, including the Medical Imaging Buyers Guide. It’s free for providers and thousands of dollars for the rest of us.
Florida Hospital DeLand, which is part of Adventist Health System, goes live on Cerner CPOE.
Memorial Hospital (IL) selects Summit Healthcare as its integration partner as it migrates to Meditech 6.0.
Saint Luke’s Health System (MO) will implement the SeeMyRadiology.com platform to share medical images across the enterprise.
I’m guessing that Mr. H is the new BFF of Louise L. Liang. MD. In case you missed it, Mr. H wrote a terrific review of her book, Connected for Health, recommending that that basically anyone with an even remote interest in IT and healthcare read the book. The masses took the message to heart and from about 8:00 this morning until 3:15 this afternoon, the book has climbed from #2,223 on Amazon’s bestseller list to #218. It also moved from #90 to #8 on the Medicine bestseller list and from #4 to #1 in the Public Health category. Heck, Dr. Liang should buy Mr. H a Christmas ham. Speaking of Christmas, I’m putting the book on my list.
Preliminary data from HIMSS Analytics suggests that 22% of hospitals are capable of achieving 10 or more of the required core measurements for Stage 1 Meaningful Use; 40% have the capability to meet five or more of the menu items. HIMSS Analytics says it will provide quarterly updates on hospitals’ progress beginning January 2011.
Apple’s AppsStore rankings for the Top 10 EMR and Operational apps can be found here. Bedside by IMS MAXIMS tops the EMR and Operational apps list and ranks 150th in the overall medical category.
A spokesperson for Advocate Health Care says patients experienced little or no interruption in care despite an 11-hour computer crash that affected 10 Chicago-area hospitals. The health system’s Cerner system went down about 5:00 a.m. Saturday, requiring employees to take patient orders on papers and access records using backup computer systems.
Sponsor Updates
- Chandler Regional Medical Center (AZ) will implement the GetWellNetwork interactive patient care solution and integrate it with its Meditech 6.0 system.
- API Healthcare names Lisa LaBau COO. She was previously with Cerner and Dynamic Healthcare Technology.
- Precyse Solutions appoints William F. Bria II, MD, CMIO for Shriners Hospital for Children in Tampa, to its advisory council.
- Allscripts wins the 2010 Excellence Award as the fastest growing company by the North Carolina Technology Association.
- Baptist Health Care (FL/AL) executes an agreement with NextGen to deploy its EHR and PM solutions for its employed physicians. Baptist will also offer system access for community physicians who choose to purchase the solution.
- CareTech Solutions added three new healthcare clients to its Web products and services division last month, including San Juan Regional Medical Center (NM), Southern New Hampshire Medical Center (NH), and Wheaton Franciscan Healthcare (WI). The company also announces Version 4.0 of its CareWorks content management system for hospitals.
- CapSite will present at the 22nd Annual Piper Jaffray Health Care Conference, to be held November 30 – December 30 in New York.
- ICA earns a spot of The Nashville Post’s Fast 50 Award for being one of Middle Tennessee’s fastest growing companies.
- At its annual user conference last week, Nuance recognized 25 healthcare organizations for saving one million dollars or more on medical transcription costs as a result of implementing Nuance’s eScription platform. Eight other organizations were also recognized for their gains in medical transcriptionist productivity.
- McKesson partners with the Emergency Nurses Association to offer the ED Benchmarks Collaborative, a Web-based subscription service that helps EDs identify trends and compare their performance with that of other facilities.
- Ingenix CTO Art Glasgow will speak Thursday at a congressional luncheon on the state of HIE initiatives at the Institute for eHealth Policy in Washington, DC. It will be broadcast online for those who can’t make it to DC.








If you’ll take a slightly used copy, Inga, I’ll send you mine once I finish…with a fresh Christmas bow, of course! (Knowing Mr. H’s snarky temperment and broad industry insight, I figured such a glowing review meant I needed to hit Amazon post haste last night.)
Re: getting physicians to standardize processes. Princeton economist Uwe Reinhardt says that trying to get physicians to work together is like trying to get eagles to fly in formation.”
First, serious clinical medicine is not a collection of “processes” such as on an assembly line. Trying to “standardize processes” in medicine is not appropriate to the domain.
There are other areas where that type of thinking has resulted in disaster. As in The Trouble With Robo-Lending“, WSJ, Nov. 13, 2010:
Amir Bhidé wisely notes that “high-touch gave way to high-tech. Statistical models that took no heed of specific circumstances replaced the bankers’ on-the-spot judgments” [with “standardized processes”] and that “Robo-lending and the securitization it facilitates lead to the misallocation of capital and economic instability.”
“Robo-medicine” that takes no heed of the specific circumstances of patients will fare equally poorly.
Finally, Reinhardt has significant conflicts of interest that could motivate him to support “standardization of medical processes.” Reinhardt, a Princeton economic professor who often writes about health care for the New York Times’ Economix blog, earns more than $500,000 a year working for a number of health care companies. He also holds more than $5 million worth of related stock. You can read more about that at this link.
Not that this proves his opinions are wrong, but I take them with a large grain of NaCl.
Re: Physicians walling off nurse practitioners and a hundred years ago, being barely better trained than barbers and butchers.”
Also in the WSJ today is this letter:
Richard E. Tarrant asserts that there is no need for primary-care doctors as that care can now be provided by mid-level providers (Letters, Nov. 10). I saw an ad in my local paper in which nurse practitioners said that they have 400 hours of clinical experience prior to entering practice.
A conservative estimate of 4,800 hours would approximate the clinical experience of a medical student. As a family practice resident 30-plus years ago, I gained at least 10,000-plus hours of clinical experience before practice. Today’s resident in primary care would have somewhat less, but they would still have in excess of 9,000 clinical hours.
Would you prefer a primary-care provider with 400 hours of clinical experience or one with 14,800 hours of clinical experience?
Claude L. Kinzer, M.D.
Huntsville, Ala.
I think that’s self explanatory. Having supervised PA’s in the past, they’re great if you need sutures or some minor illness treated, but woe unto a person who has a really serious problem, either overt or covert.
Training and experience matters.
Re: “I’m guessing that Mr. H is the new BFF of Louise L. Liang. MD”. Watch out Oprah! “Freedom” wasn’t that good anyway. When is the next book review? What are your top 10 favorite healthcare related movies? Your public needs to know!
Re: Fallon Clinic medical records article above
This situation actually brings up an interesting scenario that some physicians may find unpalatable. Traditionally, physicians have thought of medical records as belonging to MDs and patients, not hospitals. In an employed situation, it’s easy to see where that data belongs to the employer. However, some vendors and hospitals are now partnering to extend their ambulatory EHR to non-employed, affiliated physicians at a discount. I know Epic, for example, has been big on this. It raises the question of who owns the data? Affiliated docs surely would feel that it’s their data and their clinic, but if the hospital is providing the EHR from its central location, they are managing the data and it would appear that it really is the hospital’s data, not the doc’s. Not sure a lot of affiliated physicians have thought this through when choosing to accept an EHR provided by a hospital.
Re the Fallon doc: this is but another case for allowing patients/consumers direct access to and ability to take with them, their complete medical record/PHI. It is time for us, patients, consumers, citizens, whatever you want to call it us, to take direct ownership. As Dr Halamka wrote recently, the Electronic Medical Home’s time has come.
I always thought the effect on Believe was a vocoder, but you are correct it was indeed was Auto Tune.
Re: Top 10 EMR/Operational Apps list
The Top 10 list is actually part of an analysis of Apple’s Top 1000 apps in its Medical Category, which we included in our latest medical apps research report.
So to be clear: MobiHealthNews analyzed the 1000 apps and determined which ones were EMR or operational, not Apple.
ok… it’s the weird news that left a bad taste in my mouth today… did you take the poll on the linked website? apparently people are actually siding with this murederous slug…. yah, sure, the kid should have been wearing a helmet BUT he shouldn’t have been killed by some scumbag driving double the speed limit on the wrong side of the road! What is wrong with America!
Re: the Fallon Clinic
I don’t see how the EHR per se is the problem here. If the clinic would have been on paper, the departing doc would have been unable to take the paper charts with him. At least this way, he will get something on a CD.
As to affiliated docs having EHRs from the hospital via the Stark exemption, the data belongs to the entity which signs the EHR contract with the EHR vendor. In this case the clinic, not the hospital. The data does not belong to those who “manage” the servers, either the vendor or the hospital, although both are well positioned to “create problems” for clinics who want their data back.
Ultimately, of course the data belongs to the patient, but having several thousand patients authorize data transfer to a new clinic or a new EHR, one by one, is not a very practical solution.
Re: new BFF of Louise L. Liang. MD
Mr H has been a solid contributor of music review and I can thus take only a short leap of faith on this book recommendation. EMR implementations are all around us and good lessons learned are valuable in any catagory. I’m looking forward to the read to help me with my HIE work.
Re: Motion Computing Mobile Clinical Assistant C5V
No talk of battery life, but lots of talk about swappable battery.
Last iteration was 2-3 hours (in real life usage). If people cannot remember to plug in cows, you expect them to manage multiple batteries per device?
Something that lasts an entire shift on one battery would still really need 2 per RN/MD so one could charge when the next shift comes on.
RE: MIMD
It is hard to say that standardized processes in health care can’t improve outcomes. We have plenty of room for improvement and many poor providers that could use guidance.
Interesting that no mention is made of the sales incentives put in place for mortgage mills. The sales guys (“bankers”) were creative on applications to make their prospects eligible and for them to get their bonus.
rxpete Says:
It is hard to say that standardized processes in health care can’t improve outcomes
Allow me to make the simple observation that if it is hard to say, we shouldn’t be saying it, at least until we have robust evidence it is true and does not pose significant downsides.
“McKesson CEO John Hammergren comes in at #10 in the list of the highest-paid CEOs of publicly traded companies, bringing home $24.5 million in total compensation for the year ending September 30. The company declined to comment.”
Meanwhile, back in the trenches…
The punishments will continue until he reaches #1.
…sigh…