For the broader community, Neil Pappalardo was an important person within the community well beyond the impact he had on…
News 10/15/14
Top News
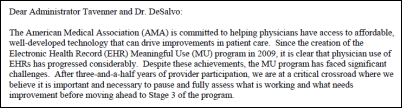
The AMA issues a Meaningful Use blueprint that calls for CMS to:
- Waive penalties for providers that hit a 50 percent threshold.
- Pay incentives for meeting a 75 percent threshold.
- Make three unpopular measures optional: View/Download/Transmit, Transitions of Care, and Secure Messaging (or as an alternative, set thresholds at less than 100 percent).
- Eliminate thresholds and menu vs. core requirements.
- Add Stage 3 measures that are more appropriate for specialists.
- Continue hardship exceptions for anesthesiologists, pathologists, and radiologists given their tiny attestation numbers and their use of systems provided by hospitals that don’t care all that much whether they can attest or not. AMA also wants a hospitalist exemption for those who treat large numbers of observation patients since they don’t qualify as hospital-based EPs in that setting.
- Leave the measures in place that HITPC suggested removing, but allow providers to qualify by meeting any 10 measures.
- Loosen the hardship exception requirements by expanding the definition of “unforeseen circumstances” and exempt hospitalists and physicians who are eligible for Social Security by the end of 2015.
- Revamp EHR certification to cover only interoperability, quality reporting, and privacy and security.
- Eliminate the requirement that only licensed clinicians can enter orders.
- Create standards for electronically passing data between EHRs and registries in a standard format, eliminating the need for middleware.
- Focus Stage 3 standards on coordination of care and new payment models rather than on data collection.
The AMA’s document also calls out C-CDA as causing interoperability problems, saying that ONC mandates its use in Stage 2 even though it has had “very little real world testing, nor was it balloted or approved for standardization by HL7” and therefore is still a draft standard with “wild variation in technology versioning.” It urges that ONC not repeat the same process of jumping on untested standards starting with Stage 3.
Reader Comments
From Media Horse: “Re: Abraham Vergese, MD’s comments about EHRs interfering with patient care. He was the keynote speaker at athenahealth’s user conference a few years ago. It was a good speech about preserving the patient-doctor relationship, but it’s interesting that he spoke for a company that’s in essence a billing company with an attached EHR. I’m not suggesting that he’s a hypocrite, but I’m sure he was paid well.”
From Number Six: “Re: Health Data Warehousing Association conference in Portland, ME last week. I was impressed by the all-volunteer organization’s conference and the low registration fee of under $500 for 2.5 days. It was held in MaineHealth’s really nice conference center and had about 170 attendees. No vendors, just data people giving concrete details of what they’re working on in their institutions. Utah presented how they incorporate PROs into Epic and Altrius had a talk on predictive modeling, which was then covered in a ‘Sharing’ session on Day 2 since it was obvious that their specs could be implemented at other places. I highly recommend the conference HIStalk readers. Next year’s meeting is in Grand Rapids.”
From Always Be Closing (Offices): “Re: CompuGroup Medical. Closing the Boston office and terminated the sales VP and several sales reps.” Unverified, but the report is from a non-anonymous insider.
Webinars
October 21 (Tuesday) 1:00 p.m. ET. Electronic Prescribing Of Controlled Substance Is Here, What Should You Do? Sponsored by Imprivata. Presenters: William T. “Bill” Winsley, MS, RPh, former executive director, Ohio State Board of Pharmacy; Sean Kelly, MD, physician, Beth Israel Deaconess Medical Center; David Ting, founder and CEO, Imprivata. Providers are challenged to use EPCS to raise e-prescribing rates for MU, improve physician productivity, reduce fraud and errors, and meet New York’s March 2015 e-prescribing mandate. Hydrocodone painkillers such as Vicodin have moved to Schedule II, with the higher CS prescribing volume adding another reason to implement e-prescribing. This webinar will describe why organizations should roll out EPCS, presented from the perspectives of pharmacy, compliance, physicians, and technology.
Acquisitions, Funding, Business, and Stock
Lifestyle healthcare technology vendor Alphaeon Corp. acquires Utah-based TouchMD for $22 million. TouchMD’s apps allow plastic surgery and OB-GYN practices to educate patients on their services to “increase consultation closings at the time of service and added procedures beyond the consultation, resulting in increased practice revenue.”
Sales

Beaver Dam Community Hospitals (WI) will deploy eClinicalWorks across its eight locations.
People

Andrew Gelman, JD will step down as SVP of corporate development for PDR Network to run a family business, but says he will keep his hand in healthcare with occasional consulting.
Facebook CEO Mark Zuckerberg and his physician wife donate $25 million to the CDC for Ebola control.

University of Arkansas for Medical Sciences promotes Rhonda Jorden to vice chancellor for IT and CIO.
ONC names Lucia Savage, JD (UnitedHealthcare) as chief privacy officer, replacing Joy Pritts, who resigned in July.
Announcements and Implementations

Mobile Heartbeat will integrate EMR and waveform data from AirStrip’s One platform into its care team smartphone app.
Eskenazi Health (IN) will use technology from Indianapolis-based Diagnotes to alert its brain center coordinators when patients are admitted, discharged, or transferred from hospitals as reported to the state HIE.
Personal health records management app vendor Hello Doctor claims it has “gained access to an API” that gives it “access to 52 percent of clinics and hospitals in the US.” That sounds suspicious since there’s no single API out there that covers multiple vendors, leading me to believe that perhaps they’ve connected to Epic in some manner and are using the “52 percent” statement incorrectly to refer to organizations rather than patients.
Allscripts will offer Shareable Ink’s documentation solution for surgical and clinical documentation for Sunrise.
Government and Politics

Rep. Renee Ellmers, RN (R-NC) issues a statement saying she’s pleased that CMS extended the Meaningful Use hardship exception after admitting that its submissions website wasn’t working correctly, but repeats her request (made via her proposed Flex-IT Act) that CMS reduce its 2015 Meaningful Use Stage 2 reporting period from 365 days to 90 days.
Beth Israel Deaconess Medical CenterCenter John Halamka, MD says the White House should choose someone from DC rather than Silicon Valley in replacing departed US CIO Steven VanRoekel:
I always support the federal government, but bold new ideas get lost in the complexity of procurement, contract management, and getting stakeholders to agree. Navigating the US government is difficult and complicated, and an outsider from Google or Facebook is likely to be eaten alive. Only an insider can navigate the process while offering new ideas and approaches.
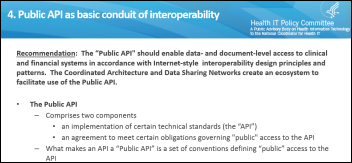
HITPC’s JASON Report Task Force will deliver its conclusions today (Wednesday), proposing that current interoperability approaches should be replaced with an API-driven model starting with Meaningful Use Stage 3. It disagrees with the JASON report’s conclusions that such an approach requires new clinical and financial systems, that the market has failed in its failure to advance interoperability, or that a newly mandated software architecture is required. The task force advocates that ONC create a public interoperability API and encourage its use via the Meaningful Use program.
ONC names 12 providers as health IT fellows.
Executives of California’s health insurance exchange are questioned about its contracting practices as a state senator claims the organization practiced cronyism in awarding dozens of no-bid contracts, some of them to a company whose owner has close ties to Covered California’s executive director.
The chief of staff of New York City’s medical examiner’s office quits following a $10.9 million no-bid, sole-source contract award to a ICRA Sapphire, whose software has cause bodies to be mishandled or lost. The city has been paying for the system using Homeland Security grants, having awarded what one lawyer called a “lifetime contract with constantly increasing costs and poor results” and hiring the India-based company’s rep as the ME office’s CIO. The previous CIO and his girlfriend were arrested for embezzling $9 million in FEMA grants intended for tracking the remains of 9/11 victims. The just-resigned chief of staff had been promoted to the position even after getting caught stealing an airplane’s exit handle from the 9/11 debris to take home as a coffee table souvenir.
Technology
Philips Healthcare begins Netherlands hospital trials of a wearable COPD monitoring sensor that collects information on physical activity, respiratory indicators, and sleep disturbances.
A reader called my attention to Xenex, whose xenon-powered pulsed UV devices (“Germ-Zapping Robots”) can disinfect hospital rooms in a few minutes, a timely topic given Ebola. Two of the company’s executives hold doctorates from the Bloomberg School of Public Health at Johns Hopkins University, while the other two were involved with Rackspace Hosting.
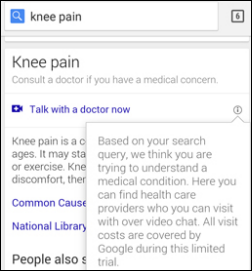
Google is testing a search feature that would allow people who are Googling medical symptoms to click a “talk with a doctor now” link.
Breathometer integrates its $100 Breeze personal breathalyzer with Apple’s HealthKit.
Other

The Brookings Institution presumably publishes intelligently written and authoritative articles on occasion, but this lame piece called “Could Better Electronic Health Records Have Prevented the First American Ebola Case?” isn’t one of them (maybe Farzad was the only person there who knew anything about healthcare IT). Its insight is zero, its valid points are few, and its flaws are many:
- It doesn’t answer the question its sensationalistic headline asks.
- It is based on a preliminary report that an EHR setup decision caused Texas Health Presbyterian Hospital Dallas to discharge the Ebola patient from its ED, which turned out not to be the case according to the hospital.
- It gets the hospital name wrong even though it’s right there on the page to which the article links.
- It wanders all over the place about EHR privacy, cost, and “voluminous files,” then meanders into healthcare policy issues, health IT competition, and a proclamation that an undefined “many”are skeptical about EHR value and the government should therefore fund outcomes research (which is already underway).

Anna McCollister-Slipp, the co-founder of an analytics company and Tricorder Xprize judge who also has Type 1 diabetes says she’s tired of waiting for digital health to flourish, pointing out that:
- Even hospitals that took Meaningful Use money won’t allow patient-sourced data to be imported into their EHRs.
- Most of the health apps were designed for people who are already healthy.
- Her academic medical center does not offer online EHR access, doesn’t allow electronic communication with its physicians, and won’t provide her endocrinologist with the software that would allow him to load her glucose monitoring data to his computer.
- None of her doctors use electronic scheduling, none offer online lab results retrieval, and only one accepts electronic refill requests.
A Pennsylvania legislator questions UPMC (PA) about its ability to send records of Highmark insurance patients to new providers when they lose access to UPMC’s hospitals on January 1. UPMC CIO Steven Shapiro says they can transfer records electronically within 24 hours, but Highmark claims UPMC will be sending faxed documents instead. UPMC uses Cerner among its variety of systems, while Highmark-owned Allegheny Health Network is moving to Epic.
Reuters covers the growing telemedicine market in China, which the government is supporting to overcome the rural-urban medical expertise gap. A report says doctors in China spend 13 hours per week online, with 80 percent of them using mobile phones.
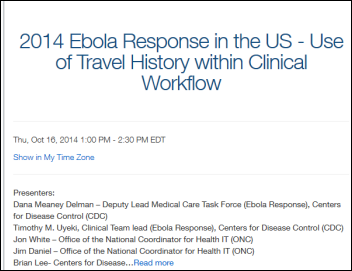
CDC and ONC will present a webinar on Thursday, October 16 at 1:00 – 2:30 p.m. Eastern to encourage providers and EHR vendors to work together to develop Ebola screening tools. CDC’s Ebola team will present its detection algorithms and travel history / medical signs checklists.

NBC medical correspondent Nancy Snyderman, MD admits that some of her crew members broke a voluntary Ebola quarantine in going out for takeout food after returning from Liberia, where the group had been in contact with an Ebola-infected freelancer. New Jersey health officials reacted to her admission by making the quarantine mandatory. She declined to say whether she herself was one of those involved as several locals who spotted her indicated.
Sponsor Updates
- Predixion Software joins the Salesforce Analytics Cloud ecosystem.
- Greenway Health’s SuccessEHS is prevalidated by NCQA to receive 27 points in auto credit toward PCMH 2011 scoring.
- Frost & Sullivan names Validic to its 2014 Best Practices Award for Customer Value Leadership.
- First Databank’s collaborative research paper is selected as a finalist in the Best Paper Competition by the American College of Clinical Pharmacy.
- The Jacksonville Daily News discusses the history of military healthcare IT solutions and calls RelayHealth a “pearl.”
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.



You forgot the ONC this week, going to “lawyer up” with hiring a United Healthcare attorney based in California. I still think they would do better at the FDA as they could work with the device folks and both viewpoints would be given on some of the Health IT systems and apps out there. It’s just technology growing together. At any rate the ONC is following the direction of HHS with getting a lawyer on board as Burwell hired one a couple months ago from Citibank. Of all things this new lawyer is to be the new privacy expert, from an insurance company that is one of the big data sellers out there. I guess everyone is in the “lawyer up” phase of healthcare anymore. I think over all HHS/CMS and now the ONC has too many people being hired from that company who has truckloads of subsidiaries into just about anything you can think of from owning a custodial bank, selling cheap Chinese hearing aids, low income housing, hospice for profit and so on.
The hospital was likely telling the truth from the get-go: the clinical system design did not include ALL the nurse’s notes in the physician workflow. For 30 years, I have seen these types of decisions made by the hospital and the vendor (influence). So as hard as it is to admit it, yeah, the clinical system played a huge role in this patient being discharged on his first visit to the ER.
I like the AMA Blueprint, it’s chock full of reasonable suggestions. One I found humorous, even if reasonable, “Loosen the hardship exception requirements by expanding the definition of “unforeseen circumstances” and exempt hospitalists and physicians who are eligible for Social Security by the end of 2015.”
As long as I’ve been working in health care IT and working with physicians to get them to adopt and engage with EHRs (since 1992), there have always been 5% of them who ‘refuse’ and claim that they will retire before they have to use the damned things. The above suggestion might have come from that stakeholder group. Lots of docs practice long after they could have retired. I think we want a better guarantee they they’ll get out of the way of progress than simply an age limit.
What a great post by Anna McCollister-Slip, but I have to ask why not name the health system? Do we not call out “GM” for its ignition switch failures rather than identify it as “a major US car manufacturer”? We have to start treating these healthcare organizations for what they are – “businesses” that are “competing” for our healthcare dollars. That’s what the “we” want right????
“Google is testing a search feature that would allow people who are Googling medical symptoms to click a “talk with a doctor now” link.” <— What the future of healthcare consumerism will look like.