Couldnt help thinking of this https://www.youtube.com/watch?v=QBV7HRGM7ns&t=174s
News 1/3/14
President Obama announces that he will nominate Leon Rodriguez, director of the Office for Civil Rights of HHS that enforces HIPAA, for Director of Citizenship and Immigration Services in the Department of Homeland Security.
Reader Comments

Photo: Brian Snyder/Reuters
From DZA MD: “Re: Baystate Medical Center. Cerner PowerChart crippled with record inpatient census and Nor’easter in full effect. Unable to process timely discharges before brunt of storm arrives.” Unverified. As I write this Thursday evening, Massachusetts is about to get nailed by a winter storm that will bring up to 30 inches of snow in places with wind chill as low as 20 degrees below zero and even colder Friday night.
From Dirk Benedict: “Re NextGen lawsuit. Mountainview Medical Center in Montana sues NextGen, saying it didn’t install its $441,000 EHR system as promised.” The six-bed hospital contends that NextGen was to install a system “which would permit MVMC to demonstrate ‘meaningful use’ of such electronic health records through all stages of applicable federal regulations” and was to complete implementation by October 1, 2013. According to NextGen’s website, NextGen Inpatient Clinicals EHR 2.6 is 2014 Edition certified as a modular EHR, so it’s difficult to determine what the exact issue(s) might be. NextGen provided us with this statement:
We cannot comment on the pending litigation, other than to say that we firmly believe the allegations made by Mountainview Medical Center are without merit and we will defend against them vigorously. We confidently stand behind the quality and performance of our products and offerings.
From Intractable Vermonting: “Re: Vermont health insurance exchange. The cost overruns have been tremendous and the politicians responsible pass it off as ‘changing project scope costs money.’ 99 percent of all IT leaders in the US would be fired if they managed a project in this fashion. Also, security is the last thing that is built into the technology before it goes live and I am sure there were shortcuts taken with all these exchanges. The hackers know that most sites require Social Security number to register.” The Vermont Health Connect insurance exchange website is the most expensive IT project ever undertaken in the state, running up a tab of $172 million, of which the federal government contributed $48.7 million. One big contractor was the ever-present CGI, which managed to turn its $42 million contract into $84 million worth of billables while missing key deadlines that kept the site from being ready on October 1. CGI was smart: the state says the delays cost $26 million, but CGI’s contract says it can be penalized a maximum of $5 million.
HIStalk Announcements and Requests
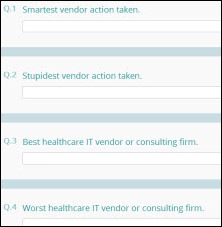
It’s time for the HISsies nominations. What’s your choice for “Stupidest Vendor Action Taken,” “Most Overused Buzzword,” “Industry Figure With Whom You’d Most Like to Have a Few Beers,” and “HIStalk Healthcare IT Industry Figure of the Year?” Enter your nominations, from which the most-nominated choices will go on the final ballot in a week or so. That means no complaining if your choice isn’t on the ballot and you didn’t nominate them.
HIStalkapalooza registration will open up the week of January 13. Read HIStalk religiously for the link to the signup notice in the next couple of weeks. We fill up really fast every year. Above is a photographic hint of the venue for those wondering. The primary sponsor has a couple of co-sponsors whose support will allow the event to be even bigger and better. If your company is interested in getting exposure as a HIStalkapalooza co-sponsor, let me know and I’ll connect you since they are willing to take on two more.
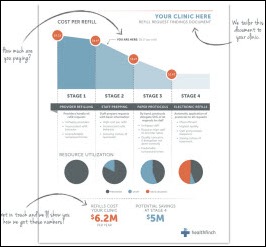
Welcome to new HIStalk Platinum Sponsor healthfinch (they tell me it’s supposed to be all lower case). The company offers RefillWizard, which improves doctor efficiency as a “Team-Based Decision Support System” that improves patient safety while reducing refill turnaround time by up to 95 percent. They begin by preparing a customized savings document like the one above and making recommendations to optimize the refill process. They have found that 62 percent of refills can be selectively and safely delegated to clinical staff, reducing the staff time to 34 seconds (some PCPs spend 1-2 hours per day just managing refills.) RefillWizard, which just won the Allscripts Open App Challenge, works either with paper protocols or integrated with the EMR. HIStalk readers probably know DrLyle (Lyle Berkowitz, MD), the company’s chairman and chief medical officer. Thanks to healthfinch for supporting HIStalk.
I found this healthfinch RefillWizard overview on Vimeo.
Upcoming Webinars (Times are Eastern)
January 7 (Tuesday), 1:00 p.m. Clinical Analytics for Population Health Management. Sponsored by HIStalk. Presenter: Core Sharma, principal analyst, Chilmark Research. As providers move from fee-for-service to value-based payment models, they must not only comply with ever-proliferating quality metrics, but also transition from a cost-plus business model to one of cost containment.
January 9 (Thursday), 2:00 p.m. Beyond the Summits. Sponsored by HIStalk. Presenters: Ed Marx, SVP/CIO, Texas Health Resources, and Elizabeth Ransom, MD, FACS, EVP/clinical leader North Zone, Texas Health Resources. Everyday healthcare executives share leadership and teamwork principles they learned from climbing some of the world’s highest peaks over the last four years.
January 16 (Thursday), 1:00 p.m. Advanced Efforts to Identify and Eliminate Waste from Healthcare. Sponsored by Health Catalyst. Presenter: David Burton, MD, executive chairman, Health Catalyst. Based on a breakthrough analyses using several large healthcare data sets as representative samples, Dr. Burton and team will present insights designed to help executives struggling to identify, quantify and extract waste from their systems
Acquisitions, Funding, Business, and Stock
Healthcare Data Solutions acquires StratCenter, a provider of healthcare provider data.
Stryker Corporation will acquire surgical sponge counting technology vendor Patient Safety Technologies, Inc. for $2.20 per share. The company’s market cap is $85 million.
Sales
In the UK, King’s Mill Hospital signs a five-year, $5.9 million EHR contract with Specialist Computer Centres and McKesson.
Medical billing company Medorizon Partners selects InstaMed’s patient payment plan technology.
The Defense Logistics Agency awards TeraRecon a maximum $30 million fixed-price contract for the procurement of radiology systems and services.
Central Georgia Health System will implement Infor’s healthcare business automation applications.
People
CareTech Solutions hires Daniel Lincoln (Palace Sports & Entertainment) as corporate controller.
CMS announces the retirement of COO Michelle Snyder, who supervised development of HealthCare.gov. The agency says Snyder had originally planned to retire in 2012 but stayed on at the request of CMS chief Marilyn Tavenner.
CareView Communications, which offers patient flow and safety solutions, promotes Steven G. Johnson from president to CEO, taking over for Samuel A. Greco, who is retiring for health reasons. Careview also names Sandra K. McRee (McRree Consulting) COO and appoints Jason T. Thompson to the board, replacing his father, Tommy G. Thompson.
Direct Consulting Associates promotes Frank Myeroff to president.
Announcements and Implementations
Baptist Memorial Health Care (TN) goes live on Epic this week at four minor medical centers and at its Baptist Medical Group clinics. Four Memphis-area hospitals are scheduled for a March 11 go-live.
Government and Politics
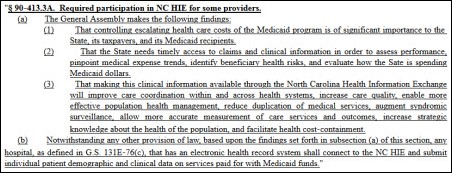
A new North Carolina law requires hospitals with EHRs to connect to the state’s HIE and submit data on services paid for with Medicaid funds.
The Department of Defense issues an RFP to keep AHLTA and CHCS running through the end of 2018 after plans for a joint DoD-VA EMR were scrapped last year when costs were estimated at $28 billion. The value of the new contract is estimated at $250 million to $1 billion. DoD is looking at a commercial replacement for contractor-developed AHLTA, whose estimated cost to taxpayers was up to $5 billion.
Innovation and Research
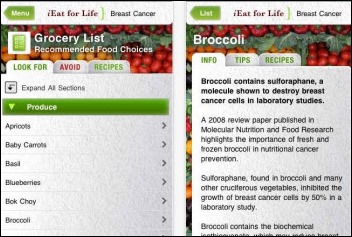
A study of 295 smartphone apps that claim to prevent, detect, or manage cancer finds no published studies that prove their usefulness, effectiveness, or safety.
Technology
The FDA extends the Kinsa Smart Thermometer the first-ever 510(k) clearance for a smartphone-connected thermometer.
The US Patent and Trademark Office issues CommVault Systems a patent for efficient data management improvements, such as docking limited-feature data management modules to a full-featured data management system.
Other
Riverside Health System (VA) announces that a now-terminated LPN inappropriately accessed the records of 919 patients over a four-year period.
Cerner completes the purchase of the 237-acre tract for its planned $4.3 billion office development in south Kansas City.
A new study contradicts the Affordable Care Act assumption that putting uninsured Americans on Medicaid will reduce ED visits, instead finding that ED visits in Oregon increased by 40 percent as the newly insured sought ED for issues that could have been handled in physician offices. The primary author, an MIT economist, concludes that, “As I tell my economics students, when something is free, people use more of it.”
The Department of Justice joins the whistleblower lawsuit of two Charlotte, NC contract ED physicians who claim for-profit hospital chain Health Management Associates offered them kickbacks to order unnecessary tests and increase admissions. The doctors say HMA’s Pro-Med software was programmed to automatically order batteries of tests on ED patients based on their complaints before they were seen by a physician. They say HMA required EDs to admit 50 percent of Medicare patients whether they needed it or not, quoting a 2009 email from an HMA executive to ED managers that said, “Big declines in over 65 admissions – you know what to do!”
A Huffington Post reprinted piece by writer and medical resident Brian Secemsky, MD doesn’t have much good to say about the EMR used by the underserved clinic where he works:
After several months of receiving emails full of buzzwords such as improved care coordination and effective closed-loop med administration from the powers that be, I couldn’t help but drink the Kool-Aid and join the anticipated excitement of integrating an innovative source of technology into an over-booked and often overwhelming practice. Where my mind was brimming with images of easy-to-use tabs, high-yield keywords and a system where clinic documentation could effectively reflect patient encounters using minimal time and effort, I was instead bombarded with yet another early ’90s-style template full of odd-sized buttons and novel concepts that were the far from intuitive. The spiked punch quickly wore off the minute I first fumbled through this bulky piece of technology, and I was back to spending hours each night typing away, well after seeing the last of my patients.
Weird News Andy likes this unlikely innovation and even suggests the above graphic for advertising. A car mechanic in Argentina falls asleep after watching a YouTube video about a machine that extracts corks from wine bottles, then wakes up inspired to invent a device that uses an inflated plastic bag rather than forceps to extract babies stuck in the birth canal. Against all odds, WHO has endorsed his invention and a US device maker has licensed it.
A bizarre article concludes that the government is planning to execute US citizens. It concludes that ICD-9 code E978 (legal execution) is part of a secret plan to create an “International One World Government,” claiming that, “Even more disturbing, is finding out American citizens have been subject to the ICP Medial code for many years. Thus, giving the United Nations our private information through coding.” The article proposes a solution even more dramatic than ICD-10 foot-dragging: the US should pull out of the United Nations.
Sponsor Updates
- Sunquest releases new versions of Sunquest Laboratory and Sunquest Molecular.
- The Boston Globe profiles Sumit Nagpa, CEO of Alere Accountable Care Solutions.
- Jason Fortin, senior advisor for Impact Advisors, discusses the impact of Meaningful Use in 2013.
- EDCO Health Information Solutions posts a Point of Care Scanning Process video.
EPtalk by Dr. Jayne
I received a lot of feedback about this week’s Curbside Consult. I’ll be posting more responses to the original reader email in the next Curbside Consult, but wanted to share some quick responses in the interim.
One reader asked for more detail about how we’ve tied the physician bonuses to EHR use. I can’t claim credit for the approach since we copied it from another organization, but it has worked well. It only applies to employed physicians using the group’s EHR platform. We have a couple of practices that we have acquired that are on other systems and are not yet converted, so they are exempt for now.
Physician bonus amounts are determined by three factors: patient satisfaction, clinical quality scorecard results, and productivity. A sliding scale is used for each element. For example you might receive 100 percent of your patient satisfaction and productivity bonuses but only 80 percent of your quality bonus.
The EHR plays into that in two ways. Since we’ve been fully adopted on EHR for many years, all of our quality reporting is now derived from EHR data (no more manual chart reviews). If providers are not documenting in the EHR, their scores will be low. We initially did a hybrid approach with both manual chart review and EHR reporting while physicians were adopting, but that has been phased out. Our staffing for compliance reviews has dropped significantly. They used to take three full work days per physician and now they take two to three hours per physician.
The major way that EHR applies to the bonus, however, is simple. All visits must be documented in the EHR and must meet our minimum data standards. These aren’t a lot different than the paper chart. The visit has to be complete within 24 hours of the patient visit and has to include certain critical data elements that essentially align with CMS coding requirements. For example, documentation has to have a chief complaint, history of present illness, review of systems, review of pertinent patient history, physical exam, and an assessment and plan.
We expected this to be present in the paper world and now it’s actually easier since the data is shared across the multispecialty group rather than living in separate paper charts by location. Providers can review histories with one click rather than having to dig for histories that may have been mentioned in various progress notes. Our physicians were not particularly good at keeping the paper problem list and past / family / social history face sheets up to date on paper.
For some practices that were challenging implementations, we actually had to physically visit the practice and make sure they didn’t have shadow charts. One site didn’t have charts, but had “jackets” for each patient. We didn’t just fail them outright but gave them three months to remediate, then audited them again. Over the last few years that the EHR requirements have been attached to the bonus structure, we’ve been fair about doing pre-audits so people know where they stand, then allowing enough time for them to remediate before their final audit.
The reader also asked about the “standards” that I mentioned our physicians have to meet to stay employed. Some are pretty simple – no OSHA or CLIA violations, favorable scores on coding and compliance audits, and getting along with their partners and staff. Some are more rigorous. We have high standards for clinical quality, and physicians are graded on blood pressure control, appropriate use of drugs for coronary artery disease, cholesterol control, influenza vaccination, cancer screening (colorectal, breast, prostate), diabetes management, and a couple of others. Physicians who can’t keep their scores in the desired range are remediated (as are their office staff – many of the metrics can be improved by leveraging staff and using standing orders including vaccination and screenings).
Finally, physicians are expected to be productive – specifically, to be above the 75th percentile based on MGMA data. That’s a lot to ask, but the group makes it clear when physicians join and it’s actually spelled out in the contract. Our compensation parallels this – our physicians consistently earn salaries in the top 20 percent based on MGMA data. If they choose to work less than full time, the productivity expectations are scaled accordingly. Our retention rate has been very good. Most of the providers who leave within five years of joining have a family reason. For example, they may only work with us for a year or two while they wait for their spouse to receive a residency or fellowship appointment that requires relocation.
In addition to their bonuses, our providers also received a hefty chunk of their Meaningful Use payments as a cash bonus. This differs from most organizations I’ve talked to that tend to keep the MU payments at the corporate level. I think the way we shared them is especially surprising given the fact that our providers don’t pay anything for EHR software, training, or maintenance. The only EHR-related charge that the practices incur is for hardware, which averages $8,000 – $10,000 per provider every three to four years.
Another reader asked how we handle the EHR records with a physician who chooses to leave the organization (or is let go) yet wants to keep his or her patients and office location. It’s actually pretty easy. We have a subsidized EHR offering (under the Stark exception) so we already have local private physicians on our EHR database with independent practice data. We simply copy the charts of active patients (those seen by the provider within the last three years) into a new practice in the EHR. Only clinical data is copied, no financial data and no accounts receivable.
If the provider is on staff at one of our hospitals, he or she may be eligible for a subsidy. Otherwise they pay fair market rate and we host it similar to a SaaS model offering. Although the providers can still share data with the employed practice, they have to do it through our private HIE rather than sharing a direct chart within the multispecialty practice. Providers are charged $0.50 per chart for the copy. That’s a holdover from our old contract when we had paper charts and they paid that much for the paper charts. I have no idea where that number came from — it’s been in place for at least 15 years.
If they choose not to stay on our platform, we have a third-party consultant perform an extract based on the new vendor’s specifications. It’s the same very skilled consultant we use when we acquire practices and bring the data into our system. Once the drive goes into the Pelican case and enters the physical transport protocol, though, it’s out of our hands.
I’ve seen two physicians treated poorly by their new vendors. One took several months to move the extracted data onto the new EHR. Another simply turned the data into PDFs and parked it in the new EHR’s scanning system, which is pretty sad considering the level of discrete data we can provide. Providers can also buy a system directly from our vendor and we’ll do the extract in that situation as well.
I’ve shared a lot of fairly specific information this week, so I hope it doesn’t come back at me. Stay tuned for the next Curbside Consult. I’ll be sharing my thoughts on infrastructure and interoperability as well as what happens when you try to drive a Ferrari in a corn field.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis, Lorre
More news: HIStalk Practice, HIStalk Connect.















A bizarre article? On a Web site called Freedomoutpost.com? Were you expecting a thoughtful, erudite review of healthcare reform? Thanks for the laugh and the insight into what at least one of the mole people is doing with his time.
#eptalk
@dr.jayne Contrary to what you state, you failed to provide much specific information, and what you provided gives me a sense that with all of the elaborate scheming by your hospital, your outcomes should be far better than those of any other hospital.
Have patient outcomes improved, or are the random metrics merely being met, and what are the unintended consequences of your elaborate and erudite scheme to incent your doctors?
@Brian Secemsky, MD
Who doesn’t have much good to say about the EMR used by the underserved clinic where he works:
Paradoxically, that underserved clinic has become further underserved by going digital. The buzz words are the same ones appearing in the Sebelius HIT promos. These same buzz words infiltrate most HIT promo and roll out speeches and press releases, to justify the $ millions going in to the vendors’ ans consultants’ coffers.
Do you think I am cynical?