Well that's a bad look as the Senators contemplate filling in the House gaps in the VA Bill
News 8/24/11
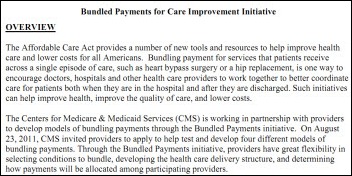
HHS announces its Bundled Payments for Care Improvement initiative, a new CMS program that allows hospitals, physicians, and other clinicians to bill their services as a single package instead of as separate items, giving them incentive to manage care better. Applicants can share in the savings over traditional fee-for-service costs, defining their episode of care as one of four models: hospital stay only, hospital stay plus post-acute care, post-acute care only, or a single all-encompassing bundled payment.
Reader Comments
![]() From BubbasChili: “Re: healthcare reform. I have the answer – legislatively re-categorize insurance companies to non-profit status and require that profits over a given amount be distributed back to consumers. I would also push tort reform, but my first idea is the fix. Just my two cents.” Maybe that requirement should be applied to non-profit hospitals first.
From BubbasChili: “Re: healthcare reform. I have the answer – legislatively re-categorize insurance companies to non-profit status and require that profits over a given amount be distributed back to consumers. I would also push tort reform, but my first idea is the fix. Just my two cents.” Maybe that requirement should be applied to non-profit hospitals first.
![]() From GladItsNotMe: “Re: Lehigh Valley, PA. Has started the evaluation process to replace the old Carecast system. Rumor has it being replaced by that little ol’ vendor out of Madison, WI.” I was too busy at work today to ask Harry Lukens, so I’ll leave this as unverified for now.
From GladItsNotMe: “Re: Lehigh Valley, PA. Has started the evaluation process to replace the old Carecast system. Rumor has it being replaced by that little ol’ vendor out of Madison, WI.” I was too busy at work today to ask Harry Lukens, so I’ll leave this as unverified for now.
![]() From PHEye: “Re: CDC’s Public Health Informatics conference in Atlanta. A speaker complained that HIStalk doesn’t cover public health.” I sometimes touch on public health topics that don’t get much attention otherwise, but those news items aren’t always that interesting to me and probably wouldn’t be to my predominantly hospital-based readers either. And while I appreciate the confidence the unidentified speaker places in a part-time blogger, full-time hospital employee to branch out into an entirely new discipline, I do need to sleep occasionally. I’d be happy to start up a fun, informative public health version of HIStalk as a public service if CDC wants to spend some of its legendary grant money to allow me to quit my day job, but otherwise I don’t have the time to take on new challenges.
From PHEye: “Re: CDC’s Public Health Informatics conference in Atlanta. A speaker complained that HIStalk doesn’t cover public health.” I sometimes touch on public health topics that don’t get much attention otherwise, but those news items aren’t always that interesting to me and probably wouldn’t be to my predominantly hospital-based readers either. And while I appreciate the confidence the unidentified speaker places in a part-time blogger, full-time hospital employee to branch out into an entirely new discipline, I do need to sleep occasionally. I’d be happy to start up a fun, informative public health version of HIStalk as a public service if CDC wants to spend some of its legendary grant money to allow me to quit my day job, but otherwise I don’t have the time to take on new challenges.
![]() From Reporting In: “Re: RelayHealth. Here’s Jim Bodenbender’s e-mail announcing that sales SVP Mike Lang has resigned to work for an EHR vendor. Jeff Gartland replaces him.” I’ll mark this as verified since RelayHealth already updated its management page with Jeff as sales SVP.
From Reporting In: “Re: RelayHealth. Here’s Jim Bodenbender’s e-mail announcing that sales SVP Mike Lang has resigned to work for an EHR vendor. Jeff Gartland replaces him.” I’ll mark this as verified since RelayHealth already updated its management page with Jeff as sales SVP.
![]() From 11YearHITVet: “Re: consulting with less travel. I’m burned out and would like a 50% or less travel schedule. Some of said go into interface work or designing Cerner PowerNotes. Ideas?” I think it depends on how you define “consulting.” Certainly you could do build work remotely, working either for someone else or yourself. Vendors do most of their work of this type offsite given ubiquitous and fast broadband (some of it remotely from Asia, in fact.) But that’s probably not the sexy, high-paying work you’re doing now as the PowerPoint-wielding, suit-wearing expert from afar. If you’re doing general management or operational consulting, it’s really a completely different line of work to do remote technical or functional application support (or to just hire on permanently with a client, for that matter). If you are willing to make that change and have experience, there’s work out there, especially if you know the hot packages like Epic or Cerner. I’ll let readers chime in since I’ve never been a full-time consultant.
From 11YearHITVet: “Re: consulting with less travel. I’m burned out and would like a 50% or less travel schedule. Some of said go into interface work or designing Cerner PowerNotes. Ideas?” I think it depends on how you define “consulting.” Certainly you could do build work remotely, working either for someone else or yourself. Vendors do most of their work of this type offsite given ubiquitous and fast broadband (some of it remotely from Asia, in fact.) But that’s probably not the sexy, high-paying work you’re doing now as the PowerPoint-wielding, suit-wearing expert from afar. If you’re doing general management or operational consulting, it’s really a completely different line of work to do remote technical or functional application support (or to just hire on permanently with a client, for that matter). If you are willing to make that change and have experience, there’s work out there, especially if you know the hot packages like Epic or Cerner. I’ll let readers chime in since I’ve never been a full-time consultant.
Acquisitions, Funding, Business, and Stock
MedAssets gets approval from its board to repurchase up to $25 million of its stock.
Sales
Presbyterian Healthcare Services (NM) signs a multi-year agreement with Health Care DataWorks (HCD) for its Enterprise Data Warehouse Appliance.
Geisinger Health System chooses Altosoft Insight for Pathology for real-time clinical and AP lab reporting.
Montfort Jones Memorial Hospital (MS) selects NextGen’s inpatient clinical and financial systems.
People
CHRISTUS Santa Rosa Health System (TX) hires George Gellert MD for the newly created position of regional medical informatics officer.
Joyce Hunter, CEO of government healthcare IT consulting firm Vulcan Enterprises, joins HavServe, a volunteerism service for developing countries, as CEO. She has volunteered with a number of healthcare IT organizations, including the local HIMSS chapter, HITSP, Maryland’s CRISP HIE, and Cal eConnect.
Announcements and Implementations
Jersey Shore Hospital (PA) and Fulton County Medical Center (PA) team up to implement Meditech EMR. The critical access hospitals expect to save about $300,000 each by sharing hardware at a hosted facility and scheduling training and implementation at the same time.
Anoto Group announces implementations of its digital pen and paper technology, including Shareable Ink’s implementations with Allscripts, Cerner, Epic, McKesson and Meditech. Other new partnerships directly with Anoto or its resellers include NextGen Healthcare, Intelligent Medical Objects, Waiting Room Solutions, Nightingale Informatix, and Bayscribe.
The Community Health Information Collaborative (CHIC) announces plans to consolidate its operations with Minnesota HIE, resulting in a single state-certified entity named HIE-Bridge.
Ministry Health Care (WI) will implement EHR Doctors’ Medibridge.net HIE technology to enable the exchange of patient information and provide patients with access to their health information.
The Electronic Healthcare Network Accreditation Commission (EHNAC) develops an Outsourced Services Accreditation Program for HIE technology service providers. The program will evaluate HIE vendors to verify they meet industry standards of quality for PHI; follow appropriate privacy and security regulations; and meet acceptable standards for technical performance, business processes, and resource management.
The governor of Guam announces the launch of its first HIE, mentioning that Guam Memorial Hospital will get $5 million in federal incentive money and another $21 million is available for doctors who sign up.
Government and Politics
![]() UK health secretary Andrew Lansley calls on developers to create applications that relate to one of five healthcare themes: personalization, improved outcomes, autonomy and accountability, improving public health, and improving long-term care. NHS is running a developer’s contest, but offering no prizes or funding. Consumers are also encouraged to submit their favorite health apps (“maps and apps”) or those they’d like to see developed.
UK health secretary Andrew Lansley calls on developers to create applications that relate to one of five healthcare themes: personalization, improved outcomes, autonomy and accountability, improving public health, and improving long-term care. NHS is running a developer’s contest, but offering no prizes or funding. Consumers are also encouraged to submit their favorite health apps (“maps and apps”) or those they’d like to see developed.
Other
![]() Once again Mr. H was robbed of a spot on this list of the 100 Most Influential People in Healthcare. Representative Paul Ryan tops the list, followed by Vermont Governor Peter Shumlin and President Obama. Donald Berwick, Kathleen Sebelius, and Farzad Mostashardi were included in the top 10, while Judy Faulkner (with an updated head shot) earned the #44 spot.
Once again Mr. H was robbed of a spot on this list of the 100 Most Influential People in Healthcare. Representative Paul Ryan tops the list, followed by Vermont Governor Peter Shumlin and President Obama. Donald Berwick, Kathleen Sebelius, and Farzad Mostashardi were included in the top 10, while Judy Faulkner (with an updated head shot) earned the #44 spot.
A watchdog organization finds that only 15 of the largest 100 HIT firms participated in HIT lobbying efforts between October 1, 2010 and March 31, 2011.
The Department of Homeland Security is soliciting vendors to provide an EHR to store medical data on undocumented residents across 22 immigration detention facilities.
Memorial Hermann Healthcare System (TX) launches Houston’s first HIE. Patients must opt in, with 96% of those that have been asked so far saying yes.
![]() Weird News Andy says he can’t top the quote in this article: “a felony case of stupidity.” A workers’ compensation billing company puts detailed medical information on 300,000 California residents on a server that it thinks is visible only to its employees. Someone Googling discovers that the entire database is wide open on the Internet. The “felony stupidity” comment was in reference to the fact that the company didn’t password-protect the information and didn’t include the “noindex” HTML meta tag that tells search engines to skip indexing that page.
Weird News Andy says he can’t top the quote in this article: “a felony case of stupidity.” A workers’ compensation billing company puts detailed medical information on 300,000 California residents on a server that it thinks is visible only to its employees. Someone Googling discovers that the entire database is wide open on the Internet. The “felony stupidity” comment was in reference to the fact that the company didn’t password-protect the information and didn’t include the “noindex” HTML meta tag that tells search engines to skip indexing that page.
![]() A reader sent over a new JAMIA article called Factors Contributing to an Increase in Duplicate Medication Orders After CPOE Implementation. It looked at the impact of implementing Epic’s CPOE in a 400-bed hospital’s adult and cardiac ICUs (Geisinger, I believe). The number of duplicate med warnings quadrupled, which the study found was caused by (a) multiple providers entering orders at the same time; (b) lack of hand-offs; (c) design problems that caused false alarms; (d) poor data display, where providers entered a new order because they didn’t notice an existing one; and (e) poor local design of order sets that contained pre-built duplicates. Providers both pre- and post-study were neutral about the value of duplicate therapy alerts. The study also found that some potentially duplicate orders weren’t flagged, such as duplicates with differing routes of administration and serial orders where the same therapy was ordered at slightly different times. I didn’t see anything surprising here: duplicate warnings are the ‘stupidest’ of the usual medication screening types (drug, dose, allergy, interaction, drug-lab, drug-disease, etc.) and usually make up at least half of the useless warnings that providers see. There’s no really smart way to tell whether two PRN meds that both contain acetaminophen will be a problem – if the patient gets one or the other but not both, then there’s really no duplication (but that can’t be determined until administration time, not when the order is entered). Smarter systems ignore route differences (IV vs. topical gentamicin) and maybe skip PRN duplicates and those from the same order set completely, but otherwise it’s almost impossible to separate intentional duplication vs. unintentional. Give the high percentage of provider overrides, one might postulate that duplicate warnings do more harm than good, masking significant problems of other types with their sheer volume and rarely resulting in DC’ing one of the alleged duplicates. I’m not optimistic that it’s a solvable problem – you won’t get a useful answer if you ask providers to sketch out a universal decision tree of when to trigger a duplicate alert, so you can’t expect the computer to improve a process that can’t really be designed. Turning duplicate alerts off completely might be the best strategy.
A reader sent over a new JAMIA article called Factors Contributing to an Increase in Duplicate Medication Orders After CPOE Implementation. It looked at the impact of implementing Epic’s CPOE in a 400-bed hospital’s adult and cardiac ICUs (Geisinger, I believe). The number of duplicate med warnings quadrupled, which the study found was caused by (a) multiple providers entering orders at the same time; (b) lack of hand-offs; (c) design problems that caused false alarms; (d) poor data display, where providers entered a new order because they didn’t notice an existing one; and (e) poor local design of order sets that contained pre-built duplicates. Providers both pre- and post-study were neutral about the value of duplicate therapy alerts. The study also found that some potentially duplicate orders weren’t flagged, such as duplicates with differing routes of administration and serial orders where the same therapy was ordered at slightly different times. I didn’t see anything surprising here: duplicate warnings are the ‘stupidest’ of the usual medication screening types (drug, dose, allergy, interaction, drug-lab, drug-disease, etc.) and usually make up at least half of the useless warnings that providers see. There’s no really smart way to tell whether two PRN meds that both contain acetaminophen will be a problem – if the patient gets one or the other but not both, then there’s really no duplication (but that can’t be determined until administration time, not when the order is entered). Smarter systems ignore route differences (IV vs. topical gentamicin) and maybe skip PRN duplicates and those from the same order set completely, but otherwise it’s almost impossible to separate intentional duplication vs. unintentional. Give the high percentage of provider overrides, one might postulate that duplicate warnings do more harm than good, masking significant problems of other types with their sheer volume and rarely resulting in DC’ing one of the alleged duplicates. I’m not optimistic that it’s a solvable problem – you won’t get a useful answer if you ask providers to sketch out a universal decision tree of when to trigger a duplicate alert, so you can’t expect the computer to improve a process that can’t really be designed. Turning duplicate alerts off completely might be the best strategy.
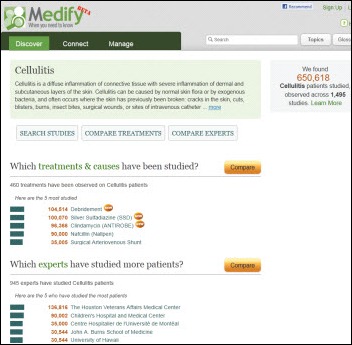
![]() Seattle startup Medify, staffed with former employees of airfare prediction company Farecast, is creating a searchable consumer database of vetted research study information covering side effects, treatments, and symptoms with social networking connections to similar patients. I struck out on my first search when it didn’t recognize “congestive heart failure” as a medical term, but got a lot of information on “cellulitis” (which talked a lot about maggot therapy for debridement). It’s aimed at consumers, but it looks to me like clinicians would find it useful to get current thought on treatments (not to mention that consumers aren’t going to pay out of their own pockets, but the usual pharma/insurance companies might if it could improve outcomes or cost). Besides, a lot of what it returns is barely understandable even to providers, like when I clicked “clindamycin” for cellulitis and got, “A semisynthetic broad spectrum antibiotic produced by chemical modification of the parent compound lincomycin. Clindamycin dissociates peptidyl-tRNA
Seattle startup Medify, staffed with former employees of airfare prediction company Farecast, is creating a searchable consumer database of vetted research study information covering side effects, treatments, and symptoms with social networking connections to similar patients. I struck out on my first search when it didn’t recognize “congestive heart failure” as a medical term, but got a lot of information on “cellulitis” (which talked a lot about maggot therapy for debridement). It’s aimed at consumers, but it looks to me like clinicians would find it useful to get current thought on treatments (not to mention that consumers aren’t going to pay out of their own pockets, but the usual pharma/insurance companies might if it could improve outcomes or cost). Besides, a lot of what it returns is barely understandable even to providers, like when I clicked “clindamycin” for cellulitis and got, “A semisynthetic broad spectrum antibiotic produced by chemical modification of the parent compound lincomycin. Clindamycin dissociates peptidyl-tRNA
from the bacterial ribosome, thereby disrupting bacterial protein synthesis. (NCI04)” Not exactly a compelling Facebook post like the maggots would have been.
![]() The Washington Post highlights an interesting conflict: Medicaid is trying to reduce overuse of EDs as free doctors’ offices to save taxpayer dollars, but much of the potential savings isn’t being realized because hospitals are aggressively marketing their EDs for routine care, hoping to pump up profitable admissions. A quote from South Carolina’s Medicaid director: “When you are advertising on billboards that your ER wait time is three minutes, you are not advertising to stroke and heart attack victims.” For-profits HCA (which runs wait time billboards) and Tenet (which runs billboards and also accepts online ED appointments) claim they haven’t seen a significant increase in Medicaid visits.
The Washington Post highlights an interesting conflict: Medicaid is trying to reduce overuse of EDs as free doctors’ offices to save taxpayer dollars, but much of the potential savings isn’t being realized because hospitals are aggressively marketing their EDs for routine care, hoping to pump up profitable admissions. A quote from South Carolina’s Medicaid director: “When you are advertising on billboards that your ER wait time is three minutes, you are not advertising to stroke and heart attack victims.” For-profits HCA (which runs wait time billboards) and Tenet (which runs billboards and also accepts online ED appointments) claim they haven’t seen a significant increase in Medicaid visits.
Hospitals in Wales are testing university-developed software that can reduce wait times and analyze the cost-effectiveness of medical treatments. It uses simulation and queuing theory, which the project’s director likens to a 1990s computer game called Theme Hospital that allows what-if analysis.
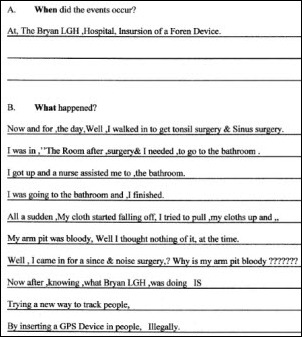
![]() Here’s the kind of lawsuit lunacy that forces hospitals to hire expensive lawyers. A (barely literate) former patient claims a hospital surgeon, while removing his tonsils, implanted a GPS tracker into his armpit.
Here’s the kind of lawsuit lunacy that forces hospitals to hire expensive lawyers. A (barely literate) former patient claims a hospital surgeon, while removing his tonsils, implanted a GPS tracker into his armpit.
Sponsor Updates
- Shareable Ink will participate in the Innovation Booth at next week’s Allscripts user group meeting, ACE. The company also gets a mention in a Wall Street Journal article discussing Nashville’s growing healthcare industry.
- Holon introduces Pharmacy Workflow Manager, which allow hospitals and IDNs with multiple locations to manage and report workload and productivity.
- GE Healthcare launches Centricity Business 5.0.
- TeleTracking announces the release of RTLS TempTracking.
- CynergisTek announces the release of its Meaningful Use Security Program to assesses compliance with security regs and reduces risk in preparation for MU attestation.
- Modern Healthcare’s 2011 Top 100 Best Places to Work in Healthcare includes Aspen Advisors, Encore Health Resources, Enterprise Software Deployment (ESD), Hayes Management Consulting, Iatric Systems, Impact Advisors, maxIT Healthcare, and The Advisory Board Company. Rankings will be revealed in October.
- Sentry Data Systems will attend Health Connect Partners Hospital Pharmacy Conference next month in Phoenix.
- Orion Health is hosting a free webinar on August 31 entitled Integrating HIE into Clinical Workflow.
- e-MDs launches e-MDs Rounds for the iPhone, giving doctors access to their EHR data via their mobile device.
- Jason Colquitt, Greenway Medical’s director of research services, is elected to a two-year term on the HIMSS EHR Association’s executive committee.
- Perceptive Software hosts a job fair this week at its Shawnee, KS headquarters. The company is seeking to hire more than 60 people in R&D, sales, and professional and technical services. Also announced: the company’s ImageNow product has earned Modular HER certification for both inpatient and ambulatory.
- Informatics Corporation of America and the Health Information Exchange of Montana announce that as of June 6, 2011, three hospitals and one community health center are connected using ICA’s CareAlign HIE solution.
- ZirMed earns its sixth consecutive spot on Inc magazine’s annual ranking of the nation’s fastest-growing private companies.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.



















I’d be happy to start up a fun, informative public health version of HIStalk as a public service if CDC wants to spend some of its legendary grant money to allow me to quit my day job, but otherwise I don’t have the time to take on new challenges.
Soooo, why don’t you throw that out there so someone in that “specialty” and see who bites? We have Inga, Jayne, Gregg, Ed, and more all bringing their various viewpoints to the table. I actually might be interested in reading about PH and CHCs once in awhile afterall, I think healthcare will become even more “global” and less siloed/isolated in the years to come and these venues will be just that. We’ll see more of a continuum of care across practice settings me thinks!
Re: 11YearHITVet: It is possible to do consulting work without traveling extensively. I have done so the last 6 years. The key for me has been to live in a larger (doesn’t necessarily have to be NYC or LA) metro area and have experience with a major EMR system- Cerner, Epic or Meditech. Even better to have experience with more than one system.
Mr H:
Bryan LGH is in Lincoln, NE. We have our own set of weirdos.
[From Mr. H] Thanks, Pete. The patient is actually suing Baylor and Bryan LGH together for some reason even though only Bryan is mentioned in the part of the complaint I listed.
re: 11YearHITVet. I also consult 100% remotely, and Mr. H is correct – this type of role works well for building/technical support. Many hospitals still operate under the “if we don’t see you, you’re not working”, applied to both consultants and FTEs, but being in a build role means that you have tangible progress on projects that they can measure. Project Management may be hard to do remotely – after all, how many spreadsheets are you really asked to put together in a day?
In your recitation of HIT companies in Modern Healthcare’s “Best Places to Work” list, you overlooked Beacon Partners.
Modern Healthcare top 100 – Should I count myself fortunate that not a single one of the named persons is a Facebook friend or on my 500+ LinkedIn connections list? Or is my career forever to be doomed in the low swampland of Healthcare IT?
🙂
Reader99: If you looked at the entire list it’s obvious Beacon Partners (surely your employer) wasn’t overlooked. Only a sampling of the list was provided on HISTalk. There are a number of HIT companies that weren’t included here. And of the ones that were mentioned, many of them are adveritisers on the blog.
Mr H,
Your comments about the JAMA article on duplicate med warnings is timely.
At the 5/11/2011 HITPolicy Committee Meeting, Carl Dvorak, EVP of Epic Systems made the following request concerning drug-drug interaction checking. Carl asked if it would be possible to get a nationally standardized list of overrides as soon as possible to avoid change management problems for software vendors. Chairman Paul Tang indicated that this activity would be moved to the HIT Standards Committee (HITSC) as soon as possible so that they can either point to an appropriate list (if one exists) or begin developing one soon.
I polled my pharmacy friends who told me in no uncertain terms – there is no standardization. The drug interaction arena is very messy. Every hospital has something, but it is always modified, and rarely very effective. It’s even true for the big chain drug stores – they each have their own. My view is if the Committee opens this box they will surely find Pandora, and if they enter it we may never hear from them again. Maybe not such a bad outcome?
The shock? The horror?! Why is anyone remotely surprised there were a select number of Health IT companies that lobbied to push their interests in DC for a pile of money at stake. Pale in comparison to other medical/health care lobbies let alone energy, financial, or defense-related lobbies.