Healthcare data sucks - that song turned my Friday to Friyay!!! Gave me the much needed boost to get through…
Monday Morning Update 8/16/10
From Delgado: “Re: contracts. I thought you might want to check out a contract between an HIE and its EMR vendor participants. Some doozies: the price is fixed for all EMR vendors with no deviation and the vendor can’t charge for support for the first five years.” I was amused that this particular HIE requires that any communication to it be sent by both snail mail and fax. Maybe HIEs don’t really buy into the whole idea of electronic communication of important information.
From Nuther1BitesDaDust: “Re: MedeAnalytics. If Ralph Keiser is in as SVP, then Sandy Cugliotta must be out. When will they stop shooting the sales leader messengers? The stuff is losing in the market.” Unverified. Both still list the company as their current employer.
Listening: Sister 7, reader-recommended, female-led funk or rock or something (whatever it is, I like it). I can’t figure out if the Austin band is still active.
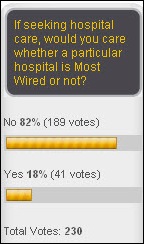
The magazines try to convince everybody that Most Wired matters. It doesn’t, according to the 82% of industry expert readers who said on my poll that it’s irrelevant to their choice of hospital (if HIT experts don’t care about a hospital’s HIT, who should?). New poll to your right, because I’ve run a similar one before and I know people get stirred up about it: what educational level should a hospital CIO have achieved? The poll accepts comments, so feel free to argue your position while expressing it.
I interviewed Debby Madeira, a nurse manager at Huntington Memorial Hospital (CA) about mobile devices on HIStalk Mobile. I don’t get the chance to interview front-line people all that often, so I would welcome more opportunities.
Verified: Ben Clark, SVP of client support for Allscripts, is leaving. He’ll be replaced by his Eclipsys counterpart, Cos Battinelli.
The Milwaukee paper does a nice piece on API Healthcare’s success following its acquisition by Francisco Partners and its appointment of J.P. Fingado as CEO.
Response to Ed Marx’s post on multitasking was overwhelming, with over 100 folks requesting a copy of his personal strategic plan. Inga and I e-mailed out a bunch of copies until Ed offered to let me make it available for anyone to download here (he felt sorry for us having to send individual copies). Note: browser quirks sometimes cause it to download as a .zip file (at least on my PC), so just rename it back to .docx so Word can open it.
Weird News Andy won’t refuse this story: paper medical records from four Massachusetts hospitals, including pathology reports, are found in a public dump. The hospitals said the former owner of a billing service used by their pathologists told them he dumped the records when he sold the company in June. I think he’ll probably regret that decision.
Shareholders of Eclipsys and Allscripts approve the acquisition of the former by the latter.
A reader sent over a copy of the McKinsey article that says hospitals will need to spend $80-100K per bed to meet HITECH requirements (with HITECH money offsetting only a small percentage of that), but will save $25-44K per bed per year as a result. Unfortunately, the article was light on detail, making any kind of critique impossible.
UK hospitals are using a not-for-profit social networking site for patients to post updates about the condition of patients. Patients can post messages or use instant messaging. NHS says the service doesn’t cost them anything to use, plus it saves nurses time since family members don’t have to call them for updates. Brilliant. I’d be selling ads, though.
Big contractor CSC says it will sue if NHS cancels NPfIT as it’s threatening to do.
Epic Staffing Guide
A reader sent over a copy of the staffing guide that Epic provides to its customers. I thought it was interesting, first and foremost in that Epic is so specific in its implementation plan that it sends customers an 18-page document on how staff their part of the project.
Epic emphasizes that many hospitals can staff their projects internally, choosing people who know the organization. However, they emphasize choosing the best and brightest, not those with time to spare. Epic advocates the same approach it takes in its own hiring: don’t worry about relevant experience, choose people with the right traits, qualities, and skills, they say.
The guide suggests hiring recent college graduates for analyst roles. Ability is more important than experience, it says. That includes reviewing a candidate’s college GPA and standardized test scores.
I bet many readers were taught by their HR departments to do behavioral interviewing, i.e. “Tell me about a time when you …” Epic says that’s crap, suggesting instead that candidates be given scenarios and asked how they would respond. They also say that interviews are not predictive of work quality since some people just interview well.
Don’t just hire the agreeable candidate, the guide says, since it may take someone annoying to push a project along or to ask the hard but important questions that all the suck-ups will avoid.
Epic likes giving candidates tests, particularly those of the logic variety.
Given my dismal experience with clueless hospital HR departments (was that redundant?), I love this guide.
Editorial Critique
Chris Lehmann, editor in chief of the online-only Applied Clinical Informatics, asked me to discuss this editorial from the current issue. It’s called Electronic Health Records – Beyond Meaningful Use, written by Asif Ahmad, soon-to-be outgoing CIO at Duke University Health System (he’s leaving for US Oncology next month). Some of its points:
- HIT adoption in academic medical centers has experienced two key events since 2000: (a) publication of an IT chapter in IOM’s 2001 Crossing the quality chasm, and (b) the HITECH act.
- HITECH makes it too easy for hospitals to look at EHRs as just having a checklist of features that lead to a buying decision.
- Hospitals should use analytics to continuously improve their EHR systems.
- Duke believes that the natural extension of Meaningful Use includes (a) support translational research; (b) support patient empowerment; (c) streamline care delivery; (d) reduce costs; (e) enable knowledge extraction and application.
It conclusion, as I inferred it, is that instead of rushing to buy and implement new EHR products simply to qualify for HITECH payments, hospitals should use and improve what they have to meet their local needs.
My first reaction was that the editorial states the obvious. However, I’m reconsidering since cooler heads need to prevail during the EHR gold rush that’s consuming the energies and budgets of many hospitals, many or most of which are likely to be disappointed by the result.
Contrary to popular perception, HITECH does not require providers to buy new systems. They’ll get paid for results, not rebated for newly incurred IT capital expense. As long as their existing system is certified, the rest is based on how they use it. It’s not a vendor problem.
For some providers, their HITECH checks will be pure gravy. They’ll just use their existing systems better and earn a check without spending any new capital dollars.
For other providers, disappointment lurks. Just buying a new system doesn’t get you anything. Writing a big vendor check won’t automatically trigger even bigger government checks. HITECH money must be earned the hard way — by creating change.
I’ve been involved in a few hospital EHR selections and implementations. It takes quite a while to do them wrong and even longer to do them right. I would bet most of the Johnny-come-latelys won’t be ready by 2012 even if their vendors are. And I can only hope they don’t harm patients in their frenzied attempts to take the HITECH checkered flag.
Asif’s third point is easy to gloss over. Everybody talks about analytics, so it’s easy to miss his point: EHRs are massively complex living and breathing packages of processes that coalesce around business and clinical rules that are almost always poorly defined and documented. EHR customers cause many more EHR failures than EHR vendors. These aren’t set-it-and-forget-it systems that can be checked off as completed once the switch is thrown and the IT people are sent away to work on other stuff.
Asif doesn’t offer examples of analytics, but here are some I came up with. How has CPOE changed ordering and utilization patterns? How quickly can be be used to correct clinical problems, such as inappropriate drug utilization or lack of documentation needed for research or reimbursement? How quickly can CPOE and decision support changed clinical practice based on new findings, such as new dosing algorithms or promising adjustments in how diabetic patients are managed? How often do providers heed guidance offered in order entry and documentation? How have clinical system changes impacted length of stay, cost per DRG, and outcomes? What information is available to analyze outcomes by provider, by treatment, or by predisposing factors? What can be done to standardize practice by the use of order sets and predefined pathways? How can clinical systems support applied research, such as the effect of rotating antibiotics on a given service or the use of new medical devices in selected patient populations?
One of the most disgraceful aspects of US healthcare is also one of the least noticed: it takes decades before doctors actually use in practice the mountains of available (and expensive) research that could improve lives. Unless someone or something pushes them forcefully, doctors keep practicing like they did straight out of residency (that’s not opinion, that’s fact). The best way to get their attention is to pay them to do it a certain way. The second best way is to push them electronically by making it convenient for them to do the right thing.
Asif’s last point is also easy to gloss over as fluff, but it’s not. Let me paraphrase to make his point more clear: hospitals are lazy, incompetent, or both if they can’t think of anything better to do with their expensive new EHRs than punch an MU checklist and bank their stimulus check. I believe that’s Asif’s challenge to hospitals: do something with your EHR that benefits patients and not just your CFO.
Those with hospital experience know how big IT projects progress: (a) internal interest turns into impatience after the fun parts of the project, like site visits and system selection, are over; (b) once the hard work begins, the vendor and product chosen are almost always maligned as deceitful, undesirable, and unresponsive; (c) going live is such a drawn-out process that the project team is disbanded immediately afterward to catch up on deferred work; and (d) nobody goes back to measure before-and-after performance and push the organization to keep using, improving, and learning (often because that wasn’t budgeted upfront).
The five points he lists as the role of the EHR are nearly universally applicable. Even if they aren’t, every hospital should make their own list: what exactly do you hope to accomplish with this software other than to make people use it in some unspecified way? What are your success criteria and how will you measure them in a way that’s specific to patients? Is the organization capable of mandating change?
Practice makes perfect in almost everything, including EHR usage. Nobody get it right at go-live. Docs scream, nurses roll their eyes, and the IT people cast downward glances at their shoes even more often than usual. When the first batter doesn’t knock one out of the park, the crowd streams for the exits.
None of that makes any sense whatsoever. Quality improvement is, by definition, continuous. Usually it happens without anyone even noticing until some obscure quality geek armed with Excel e-mails out a graph that startles everyone: holy crap, we actually changed something for the better. The overriding question should always be: are we delivering better patient care today than we were yesterday?
Uncle Sam, Asif, and your vendor can tell you how to Meaningfully Use your EHR. They can’t tell you how to use it meaningfully. There’s a difference. Each hospital must choose its own goals and the methods by which it will achieve them. MU is the least common denominator, the gentleman’s C that causes no shame, but earns little respect. What hospitals do beyond being minimally compliant with the MU checklist is meaningful. That’s the part that will make all those taxpayer billions worth it.



I think too many people are drinking the cool aide in the hospital cafeteria. Who are we here to please? Obama? ARRA? histalk? CEO’s? HIMSS? How about we just cure some patients or get them to take better care of themselves….llllllll One at a time.
Re: Epic staffing guide
Epic likes giving candidates tests, particularly those of the logic variety.
They’ve flunked their own test with these staffing recommendations.
While there’s some good point there, the part about “not worrying about relevant experience” and about “hiring recent college graduates as HIT project analysts” is downright frightening.
Medical environments and clinical affairs are not a playground for novices, no matter how smart their grades or testing might show them to supposedly be.
From a personal perspective, my grades and testing out of college were very high, and the ‘modern me’ (after medical, IT and informatics education and experience) knows I would not have wanted the ‘young me’ to have been involved in critical IT functions on that basis.
Re Epic Staffing Guide:
Epic stressing that people chose the “best and brightest” fosters an unusual workplace attitudes. Management seems to think that they are king-makers, anointing certain individuals who should be forever grateful that they have been “chosen” for Epic. Employees seem to be eating this up, seeing certification as the bullet train to awesome-town. The people most susceptible to this thinking are people who haven’t been in HIT for very long…the very people that Epic wants on their projects.
Your editorail comment was well written and pointed. It continues to be assumed without proof by Asif, you, the government, and of course the vendors, that HIT is safe.
If no one is recording the problems and adverse events as part of MU, the ignorance remains bliss.
I fathom what medical care would be like if the HITECH funds paid for more and better nurses and hospital support staff to take better care of the patients, one at a time, as the airzoneman suggests.
[From Mr. HIStalk] Can you prove that paper is safe? There’s a mountain of recorded adverse events involving paper, so I’d be surprised if so. And can you prove that paying for more and better employees improves care? I’ve seen no scientific proof that hospitals with better staffing have improved patient safety (some of the most horrific errors have come from the best and brightest academic medical centers that are wildly overstaffed compared to the average community hospital). As you can see, it’s a slippery slope when you try to challenge a point by asking for proof while letting the status quo slide by unchallenged.
Mr. HISTalk,
You editorial is one of the best I’ve read about our business. A dose of common sense, keen observations, and insights drawn from years of experience.
Thanks for the Sunday afternoon read.
Epic Staffing–some of the comments above missed the point of Epic’s strategy. They are not advocating leaders of the Epic IT project to be inexperienced novices but instead have established, experienced leadership that trains highly talented people regardless of experience to be the lower level employee. Having read the guide referenced in the blog and having seen Epic clients execute this plan over and over successfully I have become a believer.
Re: what is safe?
Medicine is not “safe.” Drugs when used as directed cause death.
Your comment merits my comment: “As you can see, it’s a slippery slope when you try to challenge a point by asking for proof while letting the status quo slide by unchallenged.” That is not the point. There are not results to answer the questions you pose. It is not known, and probably, a hybrid system will provide the flexibility to maximize safety and efficiency. If the industry sponsored studies of CPOE devices (which were pinpoint narrow in scope at the getgo) were removed, the data does not support any modicum of safety for CPOE devices. There are not any studies proving benefit in overall care, nor are there studies proving reduced costs. They are known to be user unfriendly and disruptive devices, and, in the “overstaffed” academic medical centers committing horrific mistakes, such mistakes were associated with HIT devices and deployments.
As funds are being invested in this new unproven technology, it behooves all that there be detailed study in pilots of overall hospital care, rather than gagging the users with intimidation tactics to keep the truth about the dangers from being in the public domaine, and rather than industry favorable cya press releases from CIOs claiming always that no patient care is affected when the electronic records disappear from the screens. You will get your answers then, and only then.
[From Mr. HIStalk] Can you prove that paper is safe?
The issue really is: is health IT safer than paper?
There is no conclusive evidence it is, such as a strong trail of RCT’s. It seems instead that what we have are projections and guesstimates, the kind of evidence that would never be accepted in the pharma and medical device industries.
Further, evidence is mounting that health IT introduces new risks, or is no better than paper (see examples here and here). Further, contractual arrangements with vendors, physician fear of retaliation, and other factors such as hush money make sharing of adverse events information — or even actual screen shots of commercial HIT – difficult. Potential NHS whistlelblowers regarding all aspects of care are certainly well-gagged, see here.
Not that I am statign that healthcare IT is less safe than paper. I am saying nobody truly knows for sure. The technology is experimental.
It is inconsistent with medical ethics as I know them to introduce experimental technology on a national scale for use on patients who do not give explicit, well-informed consent on the belief and hope that the experimental technology is beneficial and beneficent. The technology’s not yet ready for widespread adoption, as per observations by the National Research Council and others such as here.
Further, when such experimentation funnels sorely needed funds from the healthcare sector to the IT sector at a time when the latter sector is in tremendous distress, having difficulty providing quality care to the most vulnerable.
I entered this field to help perfect healthcare IT. I never expected premature enthusiasm to cause it to be released large-scale prematurely, and I deeply fear that the dream o fhealthcare improvement via HIT will be denuded or destroyed by the irrational exuberance now prevalent.
My first “examples” link does not work in #7. The correct URL is here.
IT Consultant Says:
They are not advocating leaders of the Epic IT project to be inexperienced novices but instead have established, experienced leadership that trains highly talented people regardless of experience to be the lower level employee.
Good point, but these are medical environments, not warehouses of widgets. By contrast, medical interns on July 1 have had 2 years of classroom training in the clinical sciences, and actual clinical rotations in years 3 and 4 where patient care is actually provided by them. They are then overseen by the more experienced in providing progressive amounts of patient care.
You do not have to be so defensive: “There’s a mountain of recorded adverse events involving paper, so I’d be surprised if so.” It is well known that the IOM report was conflicted and a gross exaggeration, yet it is the foundation for national medical policy, and serves as the carte blanche for HIT, no matter how defective it is. Even the LeapFroggers have come to their senses.
Mr. HIStalk, there’s a mountain of and mounting recorded evidence of adverse events from CPOE and EMR systems, though these are blown off as “anecdotes” by the chief defender and promoter of HIT, Blumenthal.
The definitive take down of the IOM report on medical errors was written by none other than informatics pioneer Clem McDonald:
JAMA. 2000;284(1):93-95 (doi:10.1001/jama.284.1.93)
Clement J. McDonald; Michael Weiner; Siu L. Hui
Deaths Due to Medical Errors Are Exaggerated in Institute of Medicine Report
http://jama.ama-assn.org/cgi/content/full/284/1/93
McDonald’s paper also available at http://uwf.edu/sahls/medicalinformatics/docfiles/Debates%20USA%20death%20rates.pdf
Re: Epic Staffers. I have worked with a number of different Epic account reps. I have almost always found them to be bright, thoughtful, and very hard-working. However, they also had virtualy no understanding of Healthcare or especially workflow. They understood how the software worked, but not the environment in which it was deployed. So unless your site assigns very knowledgeable Analysts to work with them, you may not achieve the outcome you desire.
“EHR customers cause many more EHR failures than EHR vendors.” That’s a powerful statement, and the whole comment obviously elicited some powerful responses. I’ll agree that the way HITECH is being rolled out probably deserves some fair criticism. However, I’d suggest that we look beyond that fear and work toward a solution. What I see Mr. HIStalk and others advocating is not a wholesale rush to the finish line (as, admittedly, HITECH seems to push), but rather a measured inspection of current technology options that asks, “How can I use these tools to better my hospital or practice?”
It’s true that there have been adverse reactions when users handled HIT. It’s also true there have been adverse reactions when users handled paper records (as in this Monday Update). There have been adverse reactions when users handled medication, testing, and surgery. There are risk when pilots fly, drivers get in cars, and even when bicyclists ride around. Often, there is a combination of product and user flaws at work. The trick isn’t always to wholesale ban a service but an examination of what the problems are and what solutions can be found.
Fear itself can be as harmful as reckless enthusiasm. I wrote about this conflict today over at the blog, and my challenge to us all is this: what problems exist, and how can we be part of the solution?
Spot on Michelle W. stating that ‘…what problems exist, and how can we be part of the solution?’
Until the landscape of problems from and of HIT is mapped, we can not be part of the solution.
Let’s establish a national data base to which to report all deaths, injuries, adverse events, device failures,deployment insufficiencies, etc from HIT which is to include the electronic repositories and the CPOEs. Bet that the vendors will freak, as will the US Government, and Blumenthal.
Let’s establish a national data base to which to report all deaths, injuries, adverse events, device failures,deployment insufficiencies, etc from HIT which is to include the electronic repositories and the CPOEs. Bet that the vendors will freak, as will the US Government, and Blumenthal.
Wouldn’t it make more sense to report problems to the people who can fix them?
Michelle: What I see Mr. HIStalk and others advocating is not a wholesale rush to the finish line (as, admittedly, HITECH seems to push), but rather a measured inspection of current technology options that asks, “How can I use these tools to better my hospital or practice?”
Agree, but the vendors need to be asking the parallel question:
“How can I better these tools to make them more likely to permit clinician to better their hospitals and practices?”
Solid rumor: Ingenix/UnitedHealth will announce after the market close Monday that it has acquired HIE vendor Axolotl.
Re: A reader sent over a copy of the McKinsey article that says hospitals will need to spend $80-100K per bed to meet HITECH requirements (with HITECH money offsetting only a small percentage of that), but will save $25-44K per bed per year
If we take these numbers at face value, and map them against the feds expected ROI for MU bonuses…we come up very, very short. Over ten years the feds expect to save over $800 bill after putting in a $25 bill investment in IT via MU bonuses. If you take the higher numbers shown in the McKinsey report…the best you get is a 4 to 1 ten year ROI.
With numbers like that, it’s going to be tough being a CIO or CFO a few years out.
Back away from the irony, comrade Says:
Wouldn’t it make more sense to report problems to the people who can fix them?
They need more motivation than they have now.
They need more motivation than they have now
We get paid the same whether you report the problems or not. But if you don’t report them, they don’t get fixed.
In any case, exactly how do you expect this “national database” to work? You don’t trust the hospitals. You don’t trust the vendors. You don’t trust the government. Even the most advanced user isn’t going to know the cause of most problems. Who do you think is going to run this thing?
Back away from the irony, comrade Says: ‘In any case, exactly how do you expect this “national database” to work?’
Your lack of medical and pharmaceutical industry experience is showing.
Back away from the irony, comrade Says: ‘In any case, exactly how do you expect this “national database” to work?’
Like this one, and like this program.
Last time I checked the FDA was part of the government that you don’t trust.