Top News

Workflow automation vendor Athelas acquires Commure and announces a $70 million investment from General Catalyst that values the combined company at $6 billion. The business will operate under the Commure name.
Commure offers analytics workflow tools and the PatientKeeper EHR, which it bought from HCA two years ago.
Athelas co-founder and CEO Tanay Tandon will continue as CEO of Commure. The 25-year-old started Athelas when he was 17, offering a malaria test kit for smartphones.
Commure CEO Ashwini Zenooz, MD will move to a non-executive role on the company’s board. The acquisition brings together 300 employees from Commure and 500 from Athelas.
Reader Comments
From Winky: “Re: insurance company IT issues. Anybody having lick getting them to fix their problems? Things are pretty bleak at just one insurer, just as the healthcare industry tries to automate revenue cycle.”
HIStalk Announcements and Requests
Going to HLTH? So are my sponsors Best Buy Health, Biofourmis, Five9, Get-to-Market Health, Healthcare Growth Partners, Medicomp Systems, and Trust Commerce. They describe their activities in my HLTH 2023 guide.
I hadn’t use Skype for years, but it was the best choice for my video-tutoring a Ukraine woman in conversational English as a volunteer with ENGin (Ukraine has one of the lowest rates of speaking English in all of Europe, which limits its post-war market participation). Using the free, Microsoft-owned Skype was a better experience than I expected.
Webinars
October 25 (Wednesday) 2 ET. “AMA: The Power of Data Completeness.” Sponsor: Particle Health. Presenters: Jason Prestinario, MSME, CEO, Particle Health; Carolyn Ward, MD, director of clinical strategy, Particle Health. Is your healthcare organization looking to drive profitability and scale quickly? Our experts will explore how comprehensive clinical data can revolutionize the health tech landscape. This engaging discussion will cover trending topics such as leveraging AI and data innovation to enhance patient care and outcomes, real-world examples of organizations leading the charge in data-driven healthcare, overcoming challenges in data completeness and interoperability, and visionary perspectives on the future of care delivery.
Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
RCM technology vendor Alpha II acquires RCxRules, which provides revenue cycle automation.
Autism provider company Cortica raises $40 million in a Series D extension, completing the round at $115 million.
A Black Book survey of venture capital and technology investors finds the 50 top-rated emerging health IT vendors for 2023.
The $217 million growth and opportunity fund of 7wireVentures – whose founders and managing partners are industry long-timers Glen Tullman and Lee Shapiro – closes its capital raise and will use its assets to move the firm’s high-potential investments to later states and to invest in other Series B and C companies. The fund has already invested in NOCD (obsessive compulsive disorder), Folx Health (a virtual healthcare platform for LGBTQUA+), and Parsley Health (virtual chronic care).
Headway, which connects patients to in-network therapists, raises $125 million a Series C round that values the company at $1 billion.
Sales
- Four-hospital Wisconsin health system ProHealth Care outsources revenue cycle management, IT, informatics, analytics, and inpatient care management to Optum, which will take on the 800 employees who are involved.
- Fraser chooses Netsmart CareFabric to support its transition to a Certified Community Behavioral Health Clinic.
Announcements and Implementations
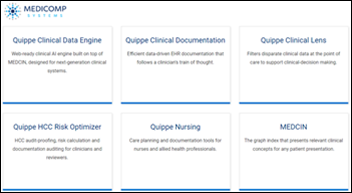
Medicomp Systems announces that its MEDCIN clinical relevancy engine features mapping of 10 million clinical codes and concepts across 12 terminologies.
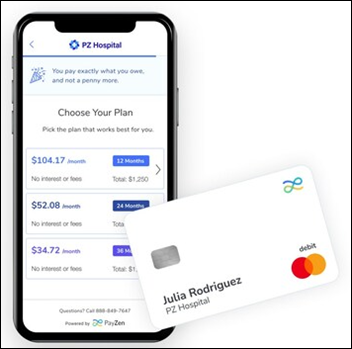
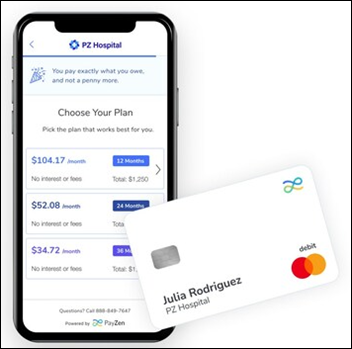
PayZen offers PayZen Care Card with partners Geisinger and UTMB, which offers patients a zero-interest payment plan for outstanding balances in the form of an upfront debit card that pays providers immediately on use.
Elation Health announces GA of a unified EHR and billing solution for high-value primary care.
University Hospitals of Cleveland completes its transition from the former Allscripts Sunrise suite to Epic.
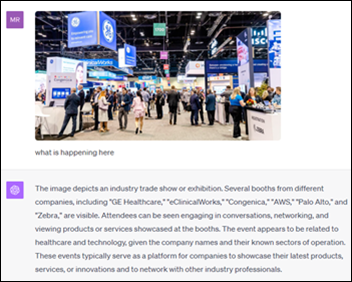
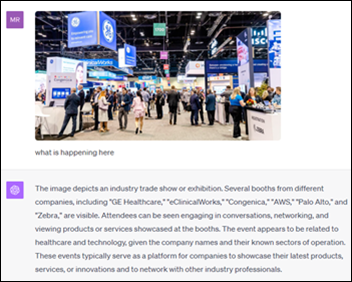
ChatGPT can now analyze images, as evidenced by this inquiry I made by posting a HIMSS conference exhibit hall photo. It proved to be more irony-aware than many humans, and more capable of explaining than I, when I asked why the HIStalk logo features a doctor who is smoking:
The image portrays a stylized and somewhat whimsical character. The pipe-smoking doctor might be an artistic choice to evoke a certain image, possibly hinting at an older, “classic” or “traditional” stereotype of a learned or scholarly individual. In literature and older media, a pipe has often been associated with contemplation, wisdom, or intellect. However, given the modern understanding of the health risks of smoking, such a depiction in a healthcare-related setting is likely intended to be ironic or tongue-in-cheek. It’s a design decision by the creators of the image and may be intended to make the character more memorable or to convey a specific tone or mood.
Government and Politics
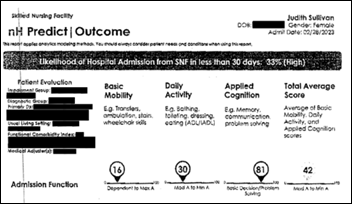
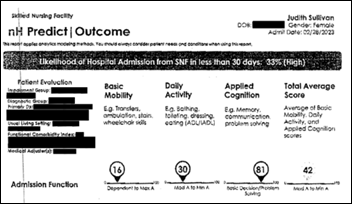
CMS will restrict the use of predictive AI tools by Medicare Advantage plans to make coverage decisions. Patients and providers complained that MA plan operator UnitedHealthcare – which uses an algorithm developed by NavHealth, which it acquired in 2020 for a reported $2.5 billion – was using its predicted discharge date to cut off coverage without considering individual patient needs as traditional Medicare would have done. NaviHealth says its algorithm was designed to personalize post-acute charge discharge planning, not to drive coverage decisions. The new federal rules, which take effect in January, will allow such software to be used only if it takes individual patient circumstances into consideration.
HHS’s ARPA-H designates up to $50 million for funding for six contract awards for developing advanced technologies to secure healthcare data. The DIGIHEALS awardees submitted these projects:
- Develop an automated medical device patching system.
- Create a cognitive health assistant.
- Develop clinician-focused tools and techniques for use during ransomware attacks.
- Identify legacy medical device vulnerabilities.
- Discover and report parsing bugs in EHRs.
- Automate cybersecurity risk assessment for medical devices.
Other
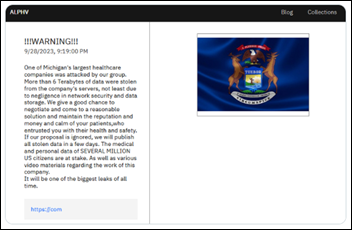
UVM Medical Center’s tells a US House cyberthreat committee that managing its 2020 ransomware attack was “much harder than the pandemic by far” as the hospital lost internet, phones, and access to the EHR for 28 days at a cost of $65 million.
A ProPublica investigation finds that pharma giant GSK developed a vaccine for TB – which kills 1.6 million mostly poor people each year – then put it on the back burner to focus on the world’s most profitable market of the US, where higher incomes and insurers can afford products such as the company’s Shingrix vaccine that has generated $14 billion in five years. The TB vaccine was developed under contract with the US Army, after which GSK patented the active ingredient, took charge of the global ingredient supply, and accepted government and non-profit funding to develop the commercial product that won’t be widely available until 2028, 10 years after it was developed, and only then because the Gates Foundation is funding it. The vaccine’s co-inventor, who originally took his idea to GSK in hopes of getting the injections to people who desperately need them, says in criticizing how Big Pharma co-opts public health research, “You get a big company to take it forward? Bullshit. That model is gone. It’s failed. It’s dead. We have to create a new one.”
The problem-plagued EClinicalWorks EHR of Hawaii’s prison system may cause a deceased inmate’s malpractice lawsuit to be dropped because the state hasn’t been able to produce his medical records 18 months into the allowed 24 month discovery period. Hawaii’s Department of Public Safety admits that the system was down for two months in one stretch, broke down again two weeks after it was restored, and is still plagued by bugs and corrupted tables. The state says it is looking for a replacement system.

Marginally health IT related, but fascinating to me, is this description of Epic’s new audio production system. Epic uses an SSL C100 HD digital audio console to broadcast software introductions – including sound effects and musical cues — to 15 countries, also producing related media in an attached “live room.” Audio engineer Paul Micksch is a former musician who started with Epic in 2006 as a software trainer. You just know that Epic Deep Space Auditorium is loaded with cool behind-the-scenes stuff.
Sponsor Updates
- Surescripts publishes a new data brief, “Pharmacy Availability & Prescribing Patterns Hint at the Future of Primary Care.”
- Robbins Dermatology experiences streamlined payment collections and processing using Healow Payment Services from EClinicalWorks.
- Medicomp Systems directly maps over 10 million clinical codes and concepts across more than 12 terminologies to its Medcin clinical relevancy engine.
- First Databank names Steve Fite regional manager, Jessica Landis commercial operations manager, and Courtney Kessler digital customer success manager.
- Rhapsody announces the availability of Corepoint Integration Engine version 7.6.
- Nordic releases a new episode of DocTalk, “DocTalk Ep. 210 | Optimizing value from EHR investments.”
Blog Posts
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.





































Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…