Monday Morning Update 12/22/25
Top News

New Mountain Capital private equity president Matt Holt leaves the firm after nearly 25 years to combine five of New Mountain’s healthcare portfolio companies into Thoreau, which will use AI to reduce medical costs. The companies are:
- Datavant — health data exchange, includes the acquired former Ciox Health.
- Swoop — drug company marketing.
- Machinify — payment integrity.
- Smarter Technologies — payment processing, formed by New Mountain in May 2025 by combining Access Healthcare, Thoughtful.ai, and SmarterDx.
- Office Ally – claims clearinghouse, payments processing, and medical practice systems.
HIStalk Announcements and Requests
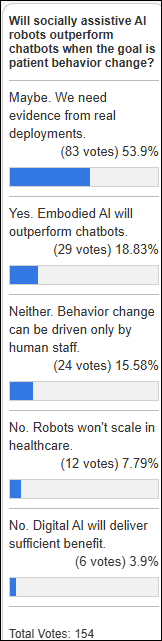
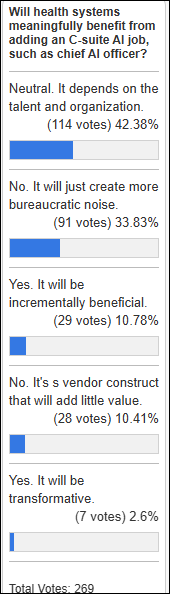
AI-powered personal care robots get a definitive “maybe” from poll respondents.
New poll to your right or here, for providers: Does your organization rely on RPM revenue enough to get excited about insurer RPM payment changes?

The top-of-page HIStalk banner has been solidly booked for years, but it is available now to the first company that commits. Its previous occupant generated over 10,000 clicks in the past 12 months, so it draws attention and interest from people who read health tech news on purpose and make decisions accordingly. Contact Lorre.
A generous donation from Mike, plus matching funds from outside organizations as well as my Anonymous Vendor Executive, fully funded these Donors Choose teacher grant requests:
- Lunar New Year resources for Ms. H’s elementary school science academy class in Youngstown, OH.
- Math tiles for Ms. M’s elementary school class in Charlotte, NC.
- Math practice headphones and markers for Ms. A’s middle school class in Ayden, NC.
- Headphones for Dr. P’s elementary school math class in Orlando, FL.
- Science fair supplies for Ms. D’s high school class in Aurora, CO.
- Hands-on science kits for Ms. G’s elementary school class in Hope Mills, NC.
- Dry erase boards and markers for Ms. F’s middle school math class in Riverdale, GA.
- Math games for Ms. M’s elementary school class in Springfield, MO.
- Classroom pillows, balance ball seating, and learning prizes for Ms. D’s high school class in Los Lunas, NM.
- Supplies, dyslexia tools, and math boards for Ms. J’s elementary school class in Las Vegas, NV.
- Special Olympics shirt-making supplies for Ms. E’s elementary school class in Dallas, TX.
- Pi Day match celebration activities and decorations for Ms. D’s middle school class in Panorama City, CA.
I note with appreciation the matching funds that my Anonymous Vendor Executive provides annually. Most readers know this person, who asks that their donations remain anonymous and instead requests giving teachers the credit. I mostly choose STEM-related teacher needs in historically underfunded schools.
Sponsored Events and Resources
None scheduled soon. Contact Lorre to have your resource listed.
Acquisitions, Funding, Business, and Stock
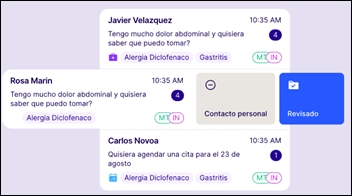
Mexico-based Leona Health raises $14 million seed funding and launches its AI copilot for physicians who use Meta-owned WhatsApp (meaning everywhere in the world except the US, China, and North Korea). Patient WhatsApp messages are routed to Leona’s app, which categorizes them, suggests responses, and supports team collaboration without exposing the user’s telephone number. I use WhatsApp on the desktop for my weekly video chats with my Ukrainian English student since Teams gave us problems after Microsoft killed Skype.
People

MRO promotes Hassan Abdallah, JD to VP / chief compliance and privacy officer.

Aaron Martin, MBA (Amazon) joins Humana as president of Medicare Advantage and will move to Insurance Segment President upon the retirement of George Renaudin in Q3 2026.
Government and Politics
HHS publishes an RFI seeking feedback on how it can use its regulatory, payment, and R&D activities to increase healthcare AI adoption.
Diagnostic radiology software vendor PenRad Technologies will pay $529,069 to settle False Claims Act allegations that its software used default settings that caused providers to bill Medicare and MassHealth for medically unnecessary breast cancer screening procedures. The whistleblower lawsuit was brought by Community Health Programs, Inc., which will collect $93,000 of the settlement. Intelerad acquired PenRad in August 2022.
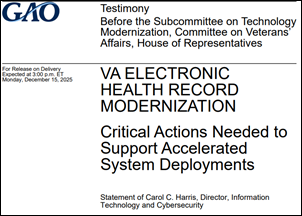
Three Democratic senators express concern to VA Secretary Doug Collins that the VA plans to implement its EHR at 13 new sites in 2026 despite unresolved issues and software defects, asking for information on rollout support resources, provider feedback, unimplemented GAO recommendations, planned staffing levels, and pharmacy-specific corrective actions.
Other
Not new, but new to me. CBS Evening News covers Baltimore family physician Michael Zollicoffer, MD, who was left without radiation treatment for his newly diagnosed cancer when his insurer declined to pay and he didn’t have the money to self-pay. His patients created a GoFundMe that has raised $300,000. He said in an award acceptance speech, “You cannot see the patient from a computer. Put it down. Look at their faces, look at their hearts, and look at their souls.”
Sponsor Updates
- TruBridge and RevSpring expand their partnership to bring enhanced financial engagement and payment solutions to rural and community healthcare.
- Wolters Kluwer Health announces the introduction of Lippincott CoursePoint+ with Expert AI for nursing education.
- CHIME’s “Leader2Leader” podcast features Optimum Healthcare IT Chief Strategy Officer Rick Shepardson.
Blog Posts
- HOPE Early Impressions: How Hospice Teams Are Navigating the New Era of Quality Reporting (Netsmart)
- 2026 Patient Experience Predictions: The Year Healthcare Becomes Consumer‑Driven (Praia Health)
- 2025: A Year in Review (RLDatix)
- Patient experience tips for mother-baby units (Sonifi Health)
- Clinical Evidence AI for Healthcare: Promises and Pitfalls (Symplr)
- Topics That Sparked Your Interest in 2025 (Tegria)
- Application Rationalization – Critical, Complex, and Absolutely Attainable (CereCore)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Follow on X, Bluesky, and LinkedIn.
Sponsorship information.
Contact us.














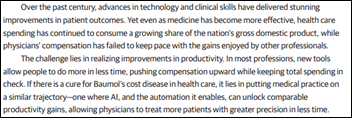












Today's post contains the phoenixes rising from the ashes of the post COVID telehealth era. There's two things that destroy…