Jeff Richards, MS, MBA is co-founder and chief development and operation officer of SnapCare.

Tell me about yourself and the company.
I spent the first 19 years of my career as a clinician and administrator in anesthesia at a large public health teaching hospital here in Atlanta, Georgia. Grady Hospital was connected to Emory University, which where I went to school. I educated clinicians that came in. I eventually moved into a leadership role, where I dealt with the complex balancing act that every administrator does — providing some clinical care, overseeing a staff of almost 100, and doing the schedule, which was the seed for launching this company with my partner in Atlanta.
When I went back and got an MBA in 2016, I wrote a paper about a mobile healthcare staffing app. Out of the blue, a classmate of mine from 19 years before reached out and said, hey, can you help me with my startup? It’s called SnapNnurse. I had not intended to start a company when I went to MBA school, but I teamed up with her and we went out to raise capital. We talked to lots of VCs who said, this is a brilliant idea, healthcare often lags behind, and creating a mobile-friendly platform for clinicians to sign up and for facilities to book staff is right on time, in 2017 anyway. We ended up raising $1 million in seed capital in the summer of 2017, launched the company, had good success here in Atlanta, and created a marketplace with about 60 facilities and 10 ,000 clinicians.
Two and a half years into our entrepreneurial journey, COVID hit. We couldn’t have known that the platform would scale the way it did or predict the benefit of how we interact with social media to sign up clinicians. We pointed it at that situation, turned into a rapid response company, and essentially grew to a billion-dollar company in 2021 and 2022, deploying thousands of clinicians in all 50 states and scaling into a different entity.
In the last 10 months, we’ve rebranded from SnapNurse to SnapCare because we’ve become a broader workforce solution, not just a contingent staffing mobile application. It’s also well past nurses and goes into the entire healthcare clinician continuum other than physicians, which we don’t staff, but do subcontract.
How has the clinician labor market and the use of contract resources changed in the past year or two as healthcare organizations tried to resolve the pandemic-caused, unsustainable labor cost trajectory?
That unprecedented demand was what was needed at the time. You needed to move clinicians around the country as fast as you could from the different hotspots, sometimes happening simultaneously. As the pandemic waned, that demand went away and went below many of the pre -pandemic levels.
As that was happening, we had evolved from a technology platform. Our orientation and what we had built changed. We said, why don’t we put the technology that we use to mobilize clinicians, engage them, match them, attract them, onboard them, credential them, and deploy them, in the hands of clients themselves? Why not empower them by plugging them into the software?
As that demand was waning, we were in the midst of rebranding into the company that we are today. Facilities are struggling from contingent staffing. There’s a lot that we can offer them as a company to help them manage their internal staff and attract, credential, and onboard candidates more efficiently than they do today.
The moving around of clinicians was like a shell game, where the supply was limited and the demand for their services was at least temporarily unlimited, which predictably sent pay rates up. Will we ever have enough clinicians to avoid ever-increasing compensation as organizations poach them from each other?
When we started this company, my research in MBA school was in the state of Georgia. In 2007, the Georgia state legislature commissioned a study to better understand and predict the healthcare workforce shortage. What they predicted was that without a massive change in the number of school schools and the number of educators – which is a huge piece of this puzzle – and the investment to support all of that, there would be a healthcare healthcare workforce shortage would begin to peak in 2017, which was when I was writing the paper. The legislature did the right thing and was correct in their assessment, but they did not fund the initiatives that would would have alleviated the problem.
To your question, the answer is a decade-long investment across the country to enable the number of clinicians who are going into school and the number of educators that are needed. A lot of resources got pulled away as facilities attracted clinicians out of educational roles to work at the bedside. It is a complex problem in the sense that that’s a decade-long fix, with lots of steps in between.
AI will probably play a role in the solution. It’s in telehealth. It’s in the way that you manage the internal staff. We recently did an acquisition, a company called Medecipher, that has a machine learning and AI algorithm for predictive analytics. It helps deploy internal staff across a six- or eight-week schedule to better match the acuity of the clinician, their specific certifications and qualifications, to the census and to the acuity of the patients. They are in different departments throughout a facility. There are absolutely tools and technologies that are on the table to help manage it, but the big picture solution is to increase the supply of clinicians.
I think AI is the future of this industry. It’s often an overused buzzword, but there’s a there’s a fast-paced change going on. Artificial intelligence has changed the speed with which technology keeps doubling the capacity. Moore’s Law, which was established by Gordon Moore in the 1960s, says that the number of transistors in a microchip doubles approximately every two years. Somehow through technology innovations and the number of chips and the way we make those chips internationally, we’ve maintained that.
Everyone thinks that AI has only come along in the last couple of years, but it has been decades in the making. But in the last 12 years, the speed with which the capacity for AI — which is software, it’s not hardware — has been doubling at a rate of every 3.4 months. It gets a little geeky to get that specific, but the highlight is that at the end of the year, it’s 400% more capable. Every quarter, things are getting faster and faster and faster.
I think we are in the beginning of a two-ish year run where the way facilities and clinicians engage will be heavily driven by AI. The companies that figure that out and leverage it will be the leaders ,and clinicians will be attracted to them because of how they can interact, get access to jobs and onboard, and maintain their credentials. All of it will be significantly easier than it is today.
How are organizations using an internal resource pool and related technologies to reduce their reliance on higher-cost outside resources?
The internal resource pool for us is a natural, the other side of the coin of the Medecipher acquisition. Number one would be to deploy Medecipher and use no contingent staff whatsoever, just better utilizing the staff that you have. Then combining it with our platform, which has a shift booking engine and matching algorithm to ensure that every facility has a pool of PRN type candidates, often without benefits at a slightly higher rate, who do that for flexibility. Maybe they work at two or three locations around town.
Most organizations don’t have the technology to send out the shift requests, send reminders, and ensure that once they do work, they get notifications to submit time cards and things like that. This is basic technology that we have used for years, and that is the offering to take that and use it to develop internal resource pool. We think that the smartest combination is to combine that with a predictive analytics scheduling solution.
Moving people around to unfamiliar facilities with different practices must create some degree of patient safety risk, plus it seems logical that a clinician would prefer to pick up extra shifts at their home organization rather than moving around. Are employers trying to create an environment to support that?
Absolutely. The facilities as employers want to ensure that. The larger part of their workforce is made up of full -time employees with full-time benefits and the facility is working well for them. But there is always a sizeable percentage, five to 10% – which is hundreds of people when you’re talking about 4,000 or 5,000 clinicians — who want to work in a more flexible way and may opt out of benefits. It may not be that they’re moving to different facilities across town. It could be that it’s a system that has two or three hospitals that are in relatively close proximity. For the option of the flexibility, to have a little more control over their schedule, they are willing to opt out of benefits.
To move them around and to mobilize them in the smartest way, you need a technology platform that can help distribute the shift requests, send reminders, and support an on-call backup auto notification that can go two or three levels deep into those who didn’t get the shift but have opted in to be in an on-call capacity. Those are basic bread and butter techniques to ensure that you have the staff when you need them and where you need them. That technology, whether its sounds staggeringly innovative or not, is missing in most facilities. We offer it as a platform.
What are the benefits of your transparent pricing promise?
We hear from facilities the same thing that I felt myself as an administrator at Grady. I’m paying this high bill rate, but what are you paying the clinician? Inevitably, somebody will get it out of the clinician. Administrators are already frustrated because they don’t want to be using contingent staffing, so they do it in a somewhat begrudging way. But it should be transparent. You should know where the dollars are going. When you’re hiring someone at a premium, dollars also go to the stipend, because you’ve relocated them. If it’s a local contractor, then you’re going to see what that margin is.
It’s a promise of trust to our clients that when when they use contingent staff, they know what it costs. We have such trust and confidence in our technology that we have driven the cost down. Those margins are much lower than a traditional legacy staffing agency, which often has brick and mortar buildings, a larger group of staff, and lower utilization of technology that require it to maintain a higher margin to pay for all of that.
Why do health systems use your services to recruit for making direct hires?
Some facilities need to make 300 hires and their HR department is not up to do that, so they seek us out. The way we differentiate ourselves is twofold. Because of our cost structure as a technology company, we can do it for less and have some of the lowest one-time costs for permanent placement when you’re doing direct hire. Then, the way we combine the our platform with social media to reach out to candidates is a broader way to access them and whatever pools they are in. The message leverages what the facility wants to do, whether they want to have an incentive like a sign-on bonus or speak to the benefits that they offer at their facility. Our reach and the interactivity of the platform with social media is another differentiator. Overall, it’s cost and the technology platform itself.
Where does the company go from here?
It’s really the shift from external contingent human capital management — the contingent staffing world whether technology enabled or not — into an increasingly pure SaaS product, where significant elements of the business are dedicated to predictive analytics. That’s the reason for the acquisition that’s only two months old. Leveraging the internal resource pool, and only when they have exhausted those techniques as well as permanent placement and have decided to use contingent staffing, to use a best in class marketplace that can aggregate PRN contract staffing, leveraging the technology across multiple different agencies to leverage the cost, get it down. We differentiate ourselves from contingent staffing competitors by seeing ourselves as constantly transforming further down the pathway towards a technology-only company.
Comments Off on HIStalk Interviews Jeff Richards, Co-Founder and COO, SnapCare




























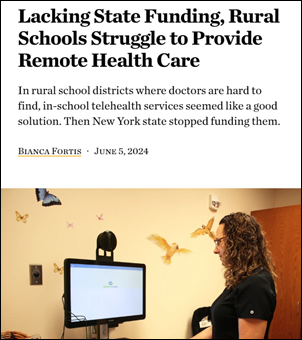

















Today's post contains the phoenixes rising from the ashes of the post COVID telehealth era. There's two things that destroy…