News 6/14/24
Top News

Ascension provides updates about its May 8 ransomware attack:
- The cyberattack was launched by a malicious email that was opened by an unsuspecting employee.
- The attackers took information from file services that employees use for daily and routine tasks, some of which are likely to contain PHI.
- Ascension is offering free credit monitoring and identity theft protection services to any patient or employee who requests it.
- EHR access has been restored in nine regions and in parts of two other regions. Organization-wide EHR access restoration is still on track for Friday, June 14.
Reader Comments
From Siri Soundalike: “Re: advice for my nurse colleague. He has many years of experience in several aspects of healthcare, earned an MBA, and was involved in starting an unrelated business. He is looking for other career opportunities and wondered what directions the diverse HIStalk readership suggests.” I will invite readers to add their thoughts. Their advice could be more targeted if they understood the type of work he wants to do (corporate employee, hands-on provider, entrepreneur,etc.) and whether he has geographic restrictions. Advice would also likely vary if he’s 30 with young children versus a financially secure 50-year-old. My first question would be, is his dream job as an employee or as a business owner? If he says “either is OK,” then more self-reflection is indicated before bringing others into the discussion.
From Kinko: “Re: healthcare disruptors. Just because a big company is dabbling in healthcare doesn’t make it a disruptor.” Agreed. You’re just a disruptor-wannabe until you actually disrupt something, which rarely happens in healthcare except in some niche where insurers and regulators don’t tread. The lumbering interlopers usually end their would-be role as healthcare disruptors and instead slink away as healthcare departers.
HIStalk Announcements and Requests
Maybe healthcare should do this. Mrs. H received an email from the shop that is checking out her car after it went into limp mode, requiring it to be towed and me to rescue her from anxious roadside pacing. A phone-recorded video that was attached to the email featured the mechanic walking around explaining what he found as he pointed at parts. An estimate or email summary would have been equally effective, but it felt more personal to have the expert explaining informally.
Webinars
June 26 (Wednesday) noon ET. “Population Risk Management in Action: Automating Clinical Workflows to Improve Medication Adherence.” Sponsor: DrFirst. Presenters: Colin Banas, MD, MHA, chief medical officer, DrFirst; Weston Blakeslee, PhD, VP of population health, DrFirst. What if you could measure and manage medication adherence in a way that would eliminate the burdens of medication history collection, patient identification, and prioritization? The presenters will describe how to use MedHx PRM’s new capabilities to harness the most complete medication history data on the market, benefit from near real-time medication data delivered within 24 hours, automatically build rosters of eligible patients, and identify gaps of care in seconds.
June 27 (Thursday) noon ET. “Snackable Summer Series, Session 1: The Intelligent Health Record.” Sponsor: Health Data Analytics Institute. This webinar will describe how HealthVision, HDAI’s Intelligent Health Management System, is transforming care across health systems and value-based care organizations. This 30-minute session will answer the question: what if you could see critical information from hundreds of EHR pages in a one-page patient chart and risk summary that serves the entire care team? We will tour the Spotlight, an easy-to-digest health profile and risk prediction tool. Session 2 will describe HDAI’s Intelligent Analytics solution, while Session 3 will tour HDAI’s Intelligent Workflow solution.
Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
Microsoft retires the GPT Builder part of its $20 Copilot Pro subscription three months after it announced it, saying that the company will shift focus to commercial and enterprise sales.
Sales
- Cloud PACS vendor Synthesis Health announces new customers Tahoe Carson Radiology, Naugatuck Valley Radiology, and Intermountain Medical Imaging.
People

Matt Wojcik, MPH (Crossroads) joins Solaris Health as CIO.
Announcements and Implementations
HealthLynked rolls out an online medical record request form that uses DocuSign to send patient information requests to hospitals, physician offices, and laboratories. The records are added to the company’s network, which allows patients to share their own records with providers.
Komodo Health announces Komodo Patient Insurance, which offers the pharmacy and medical insurance status of 200 million de-identified US lives.
Government and Politics
Federal agents arrest the CEO and clinical president of ADHD telehealth provider Done on charges of distributing Adderall, healthcare fraud, and obstruction of justice. The Department of Justice charged founder and CEO Ruthia He and Clinical President David Brody, MD for illegally distributing 40 million units of Adderall and other stimulants without medical justification, which DoJ says generated $100 million in revenue.

The Justice Department and FTC settle their claims under behavioral telehealth vendor Cerebral, which will pay $5 million in consumer refunds and $2 million in civil penalties for exposing user health information via deficient security practices and lax prescribing of Adderall. The government will continue charges against former CEO Kyle Robertson, who left the company in 2022 to start vanity online drug provider Zealthy, which targets patients who seek drugs for depression, obesity, erectile dysfunction, hair loss, and testosterone deficiency. The federal government has added Zealthy to its complaint.

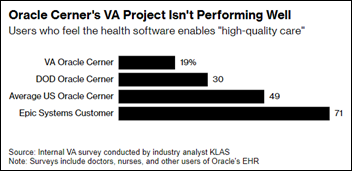
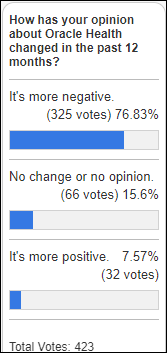
The VA extends its contract with Oracle Health for an unspecified term, presumably the one-year period that Congress mandated to hold the company more accountable for the troubled implementation.
The VA moves several technology projects and 600 personnel under its Digital Health Office, which it launched on June 2. The office will include connected care, population health, health informatics, and AI programs as the VA’s central coordinator of digital health projects. The VA is recruiting for the office’s permanent leadership, with the interim being Nadia Smith, MBA, acting chief digital health officer, who joined the VA in September 2023 after 27 years of federal government consulting.
Real Time Medical Systems accuses post-acute EHR vendor PointClickCare (PCC) of information blocking, seeking a federal judge’s intervention to compel PCC to grant access to skilled nursing patient data. PCC argues that providing that access would expose its systems to hacker bots that could slow operations or compromise patient data. Analytics vendor Real Time contends that PCC, which offers a competing service, is attempting to drive it out of business. Real Time claims that PCC previously forced its employees to perform manual queries after completing a CAPTCHA challenge, despite Real Time’s HITRUST certification. PCC says provides information to 1,900 companies via a more secure method. Real Time claims that PCC told it directly that its own introduction of a competing product meant that it would no longer provide Real Time with data access.
CMS actuaries estimate that US healthcare spending will outpace economic growth with an average 5.6% annually from 2023 to 2032. Hospital spending increased an estimated 10.1% last year. Medicare has the highest predicted 10-year average annual increase of 7.4% among payers due to increased enrollment of baby boomers through 2029. The actuaries predict that healthcare spending will increase to nearly 20% of the gross domestic product.

A US Senate Finance Committee report finds that Vanderbilt University Medical Center failed to protect patient privacy when it provided the requested records of 82 transgender patients to Tennessee Attorney General Jonathan Skrmetti. VUMC says it did not violate privacy laws because it was required to provide the records, a premise that is being questioned by a patient lawsuit and an HHS OCR investigation. The affected patients were not notified until ACLU filed a lawsuit.
Sponsor Updates

- HCTec sponsors the Tennessee HIMSS Chapter’s annual golf tournament.
- FinThrive releases a new Healthcare Rethink Podcast, “Rebel Healthcare: The True Patient Lead Journey Toward Improving Healthcare.”
- Laudio will exhibit at the Organization of Nurse Leaders Annual Meeting June 13-14 in Newport, Rhode Island.
- Bizmatics will integrate DrFirst’s RxInform patient engagement solution into its EHR to improve medication adherence.
Blog Posts
- Findhelp & NextGen: Integrating to Support the Whole Patient (Findhelp)
- Cyber Security in Healthcare: How Providers Can Improve Data Safety and Cyber Resilience (FinThrive)
- CCW Panel Recap: How We Can Empower Those Around Us (Five9)
- Breaking Silos: How SOC and Compliance Teams Can Transform Healthcare Security (Fortified Health Security)
- Award-Winning Data Visualization Solution: A Deep Dive into SDOH Software for Life Sciences (Inovalon)
- Advancing GenAI Capabilities and Bringing Interoperability Solutions to Researchers and Patients (InterSystems)
- Meditech supports innovation and cultivates partnerships at MUSE Inspire 2024 (Meditech)
- Elevate Your Quality Scores: A Guide to Maximize MIPS/MVP in 2024 (MRO)
- Embracing AI in Healthcare: Overcoming Concerns Benefits All (Net Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.


































Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…