Readers Write: Early Warning System: How AI-Driven Near Miss Reporting Can Improve Patient Safety
Early Warning System: How AI-Driven Near Miss Reporting Can Improve Patient Safety
By Tim McDonald, MD, JD
Tim McDonald, MD, JD is chief patient safety and risk officer for RLDatix.

A nurse prepares to administer a medication to a patient, notices that it is the wrong medication, and corrects the order. A surgical assistant sees that a patient has been prepped for surgery on the wrong limb and corrects the error. A patient on a liquid diet receives a meal with solid food, but a vigilant nurse notices the mistake and substitutes an appropriate meal.
In hospitals and other healthcare facilities, near miss incidents are commonplace. Robust care protocols and training of clinicians, nurses, and other staff go a long way to reducing incidents and preventing patient harm.
But for a variety of reasons, near misses are underreported across healthcare, representing a multitude of lost opportunities.
The importance of understanding how many near misses occur
The World Health Organization defines a near miss as “an error that has the potential to cause an adverse event (patient harm), but fails to do so because of chance or because it is intercepted.”
Healthcare leaders recognize that a certain number of preventable errors are inevitable. Healthcare delivery is complex, emergency rooms are overcrowded, and staff who are dealing with higher patient volumes are understandably prone to error due to fatigue or burnout.
Hospital leaders want to take measures to reduce the number of preventable harm events and have an opportunity to use near misses as a way to prevent them from escalating into serious incidents. That said, having a large number of near miss reports can be beneficial to a hospital as it indicates that a strong safety culture exists and provides valuable learning opportunities for leadership. Hospitals that effectively encourage robust near miss reporting are better positioned to identify and solve problems before they lead to patient harm.
Heinrich’s safety triangle theory holds that 300 near misses occur for every severe accident that involves a serious injury or fatality. Once hospital leaders have a good idea of how many near misses are occurring, they can use AI tools to analyze their near miss data and predict their risk for more serious adverse events. But the real challenge is getting an accurate near miss number.
Most hospitals have voluntary event reporting systems that include reporting of near miss incidents. But the fact that they are voluntary means they likely underestimate the actual number of near misses occurring. A nurse who notices a patient recovering from surgery walking the hallways without non-slip socks may not report the incident for fear of blame or any consequences of reporting. They also may not report a near miss because they believe the event not to be severe enough to warrant it.
One of the biggest reasons for the underreporting of near-misses is that clinical staff lack the time to log an incident report. For many hospitals, event reporting is manual and time-consuming, often taking around 10 minutes per report. Unless healthcare leaders take steps to simplify and streamline incident reporting, including leveraging AI tools to significantly reduce reporting time, they will lack real visibility into how many near misses are occurring and fail to fully understand the threats to patient safety.
Automating event reporting with AI
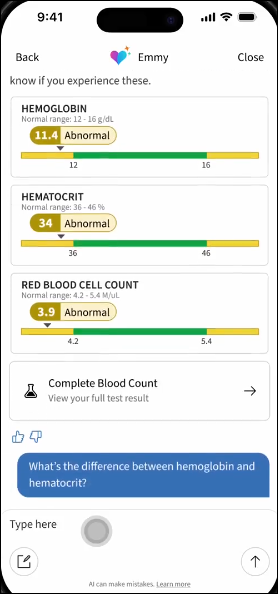
Advancements in generative AI and large language models (LLMs) offer the opportunity for hospitals to not only improve the accuracy of near miss reporting, but reduce the amount of time needed to log a report. These reporting efficiencies give back valuable time to clinical staff to care for patients. LLMs can process unstructured data, such as text, audio, and video transcripts, and understand the context, which makes it possible to extract and organize insights for a report.
For busy clinical staff, using an AI tool to accurately create an incident report, rather than filling out a report manually, could save considerable time.
As an example, say a nurse realizes that a patient with a penicillin allergy has been prescribed amoxicillin. The nurse prevents the dose from being given to the patient and requests an alternative prescription, preventing harm to the patient. The nurse takes a few minutes to make a verbal report using an AI-based event reporting tool, and moves on to their next patient. From the nurse’s voice notes, the event reporting tool generates a complete incident report, giving hospital leaders valuable insights about what happened.
Leaders can use machine learning tools to analyze near miss reports over time and detect patterns and trends, as well as anticipate risks, in order to be able to prevent harm before it happens.
Automating incident reporting, including near misses, helps reduce barriers to reporting and gives clinical staff a more active role in reducing harm system wide.
Better tracking of near-misses can serve as an early warning system
In a way, near miss incidents can indicate the diligence of clinical staff. An attentive nurse who notices an unsecured electrical cord and prevents a patient from tripping is obviously well trained.
Improved near miss reporting creates opportunities to improve processes and protocols, such as improved medication safety protocols, fall prevention measures, emergency department redesign, or training on safe injection methods.
When they are well understood and documented, near misses can act as an early warning system. When hospital leaders have a complete picture of incidents where a patient could have been harmed but wasn’t, only because of the timely intervention of a staff member or just plain luck, they can predict their risk of serious adverse events. They can understand their vulnerabilities and take corrective actions that prevent future incidents of harm.
Hospital leaders shouldn’t leave the future of patient safety to chance. Generative AI tools offer the opportunity for clinical staff to file incident reports seamlessly within their daily workflow, increasing the number of near miss reports received while decreasing the administrative burden that leads to clinician burnout and fatigue. AI and data analytics solutions give hospital leaders the ability to analyze trends over time and gain insights into how many near misses are actually occurring.
With effective use of AI-based tools, staff collaboration, and data-informed decision making, hospital leaders can raise standards of care and safety, reduce risk, and improve outcomes for all.































Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…