Jeff Robbins is founder, president, and CEO of LiveData.
Describe LiveData’s business.
LiveData’s really got two lines of business. Relevant to your readership is our healthcare business. We also got our start, and continue to service, the electric power space with a trusted real-time middleware that’s used all around the world on the electric power grid. That’s actually how we got our start in healthcare.
We were posed a challenge by folks at Mass General, who in collaboration with CIMIT had an “Operating Room of the Future” project. The paradox of new stuff is the more new stuff they brought in, while they had increasing numbers of really great new tools in the OR, the challenge was how to actually pull it all together and use it. So they posed to us the challenge: could we pull all this different kinds of data in real time onto one screen? To which, as CEO I said, “Of course.”
Then we pulled back to figure out, well, how’s that going to work? That launched us into healthcare about five years ago.
What is CIMIT?
It’s a collaborative group that involves Partners HealthCare, the parent organization of Mass General, along with MIT, Draper Labs, and other stakeholders. Their mission is to try to find technology, sometimes outside of the traditional healthcare space, and bring it to bear on healthcare.
I’ve been hearing about “The Operating Room of the Future” for years. Has it produced technologies that are actually being used?
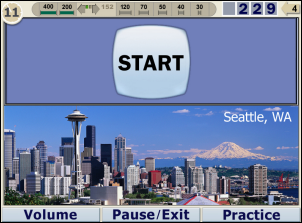
Well, that’s a nice softball for me. [laughs] Certainly one of the outcomes of that project at Mass General was Mass General deciding for their new operating rooms — they put this in their RFP for equipment for the new ORs –to standardize on having LiveData OR-Dashboard in every room. LiveData OR-Dashboard is the product name of what came out of that research.
I should say that the way we were enabled to actually work on this was through a generous grant from the U.S. Army’s TATRC Group. Through the SBIR grant process, we competed for and won a grant that allowed us to take our technology, which was already proven in the electric power space, and tailor it to the healthcare environment.
Everybody’s pushing doctors to use EMRs in their practices. Is anyone advocating OR technology?
The OR, in my opinion, is still in some ways the Wild West or the last frontier. It’s kind of a black box that’s definitely under the dominion of the surgeon. It’s widely recognized that they’re very obviously a delicate area of care. Changes come to it carefully in the hands of hospital administration.
You really do have a dedicated team of professionals among the doctors and nurses who take excellent care of each patient. Trying to get electronic stuff in the mix has all the pitfalls that I’m sure you’re aware of, where you can’t simply create an electronic version of the paper stuff you already have and expect to see better things happen.
You really do have to look at the workflow and find ways, creatively, that automated systems can actually help and reduce workload, not simply add more burden, because now all of a sudden someone’s supposed to not only do critical things on their feet, but then run over to a keyboard somewhere and type a description of it. I’d say that’s what keeps the OR somewhat on the outskirts of a lot of the efforts I read about in your paper.
As you said, physicians often find EMRS cumbersome and not meeting their workflow. Do you find the same challenges with surgeons in the design of your product?
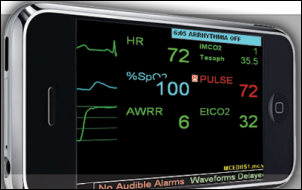
Yes. We set out deliberately to address the gap between the “doing” and the “documenting”. When we started, our product was really a read-only display that derived its information automatically from other systems, be it documentation systems where a nurse was already documenting, or in some cases the physiologic monitor or anesthesia machine. Building up more information out of existing sources without requiring any new typing. That was kind of a first leveled effort to say, “For sure no one’s going to have to do more work with our system. Let’s see if we can’t help anyways.”
Then the next step was to try to see if we couldn’t reduce the amount of work involved in certain documentation steps, with our focus at first being on the Safety Time Out, which has, I think, increasingly gotten press and awareness.
What’s the value of putting the lists in an electronic environment, as in your Active Time Out function?
There was a by-now famous study that was spearheaded by, among others, Atul Gawande out of Boston here, out of the Brigham more specifically, and also at Harvard. Brigham, being one of the teaching hospitals, it was Harvard. But the study showed that through the intervention of adding specific kinds of checklists to the surgical process, you could reduce errors and ultimately save lives and reduce complications. That’s a wonderful result and everyone gets that we need to make sure that everyone’s doing these checklists properly.
But the study itself raised the question, “How do you engineer durability into the system?” and what does that mean? If you have someone with a clipboard watching you while you work, seeing how well you actually execute a specific checklist and you’re aware of that fact, my guess is like most humans, you would start paying more attention and be kind of on-the-spot and do it.
The question is, when the person with the clipboard leaves, who’s checking to make sure you actually keep doing this checklist? Effectively doing the checklist does help. The question is, what helps people stay on task and actually do the checklist on each and every case? That’s where, again, new ways of doing the checklists using electronic technology to help and augment the process can really make a difference. That’s what we’ve been doing with our hospital customers.
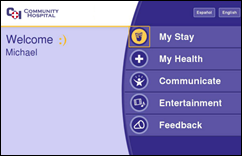
For example, we give the circulating nurse a simple clicker, kind of like a PowerPoint mouse, very inexpensive, very simple. During the Time Out, the nurse literally clicks through the checklist which is up on the wall on a screen. How that differs from having a poster on the wall, let’s say, with the checklist on it is for each step in the checklist, the relevant information for executing that check — like making sure that the proper antibiotics have been given prior to incision, as an example — the system literally scours the records of the documentation to make sure that there’s indeed a record of the proper antibiotic being given and puts that up on the screen.
Simple stuff like patient name, MRN, whatnot. Rather than just having a checklist that says, “Make sure you know who the patient is,” we get the patient’s name and in some cases, even a picture of the patient up on the wall so you can confirm that you have all the salient information to do that step of the checklist.
That’s Part A of it, having all the relevant information available automatically. Part B is, this could sound a little Big Brotherish, but it’s being handled with a lot of sensitivity by our hospital customers — we provide reports for administration as to how long was spent on each step of each checklist item for each case. You actually get beyond the documentation saying, “Yup, we did the checklist; we did the Time Out.” You get some time-based statistics. Did the checklist get done before incision? How long was spent on it? You pretty quickly get a feel, as a team in the room, for what the right amount of time is to spend on a checklist, and you can then start to tell when something really wasn’t done properly.
The hospital that recently got into trouble for not doing surgical time-outs or marking their sites surely knew they should be doing that. What would you suspect caused them not to, and how would your product have made a difference?
Well ultimately “they” — the hospital — devolved into individual surgeons who often aren’t even employees of the hospital, but obviously have privileges to operate there. Our system helps people stay on compliance with the policy and provides a record for each and every case of that actuality. It’s moving, and it’s a culture change, but its part of the hospital making the decision that yes, we shall really see that this happens on every case.
Can the tool change the culture or does the culture have to be ready to accept the tool?
As much as I’d love to say yes to the former, it’s really the latter. No matter what kind of technologies they have, the culture change is ultimately people and processes. Technology is really an adjunct. But again, my point is that technology done right is a useful adjunct that doesn’t add more work. It’s still salient to that discussion about, does the electronic medical record hinder or help our health?
Take me through a typical surgery. What is your product doing and how are people using it?
The product in the OR is part of a bigger suite of products that are all about workflow in the perioperative space. In the OR, the workflow is divvied up into some very high level phases or steps, which we call Set Up — when the room is being set up. The checklist phase. Intraop — the actual surgery is underway; debriefing and some ancillary stages prior to sending the patient off to the PACU. Some of these other phases might be in their own time frame and pop in and out.
For example, there’s workflow associated, on some cases, with sending a specimen from the OR to the pathology lab. The system will, when that’s going on, switch automatically to some information about managing that flow back and forth between the OR and the pathology lab to make sure the specimens had been marked and described the way the surgeon wants; to let the surgeon see where his or her specimen is in the pathology lab’s queue; and then ultimately to get results back from pathology in a way that the surgeon can easily see and have someone in the OR sign off on.
That’s like a detailed dive on one piece, but the major steps again are: the room setup, where the goal is to make sure all the right stuff is in the room. Then once the patient’s in the room, the briefing/checklist phase, to make sure that’s all done properly. Then Intraop is largely details of the case that unfold during the case — highlights of the patient’s vital signs, estimates of any fluid loss; and depending on the kind of case, there might be more details.
Let’s say in an orthopedic case you might have an automated tourniquet pump on for a certain period of time at a certain pressure, and that kind of data can be gleaned automatically and displayed on the wall so everyone can see it, that kind of detail about the work. First of all, we talked to different people in the room and asked them, do they need that? The anesthesiologist has his or her own bank of screens from the monitors; they don’t really need that. The surgeon might think they don’t need that, and often they’ll say that to us, “Oh yeah, I don’t need that.” But once they have it and you observe them during cases, you’ll see they start using it quite frequently just to stay aware.
Most crucially, nurses, some of whom might be changing shifts in the middle of a case or relieving someone who’s going off to lunch, can get kind of a high-level Gestalt of “Where are we in the case?” in one place, versus what they could do in principle, is log into several systems — the record, so to speak — and rummage and try to find out what’s going on that way, or talk to people. But I hope no one’s under the delusion that there’s a lot of that kind ad hoc conversation going on in the OR, because there isn’t — so metaphorically, keeping everyone on the same page.
People have said that critical IT systems should work like a pilot’s heads-up display or as in real-time instrumentation that detects events and alerts. Is the industry moving in that direction?
We feel we have delivered in our product is that heads-up display. I would argue that certain kinds of IT systems already in place in the OR are, correctly, heads-down products because they’re documentation products. Certain things do require a nurse to heads-down and type.
We’re not yet at a point where voice recognition is good enough in that kind of noisy environment, and so there are places where things need to be typed in. That, to my mind, is inherently heads-down, yet there are pieces of what are being typed that are really more high level events that should be monitored and then used.
We use them, first of all, to know what phase of the case we’re in to automatically display the right subset of information. But then, like you say, to have alerts. So if we’re getting to the Time Out before incision and there’s no documentation of antibiotics being applied — sound an alert, let’s find out. You could say, “Hey, you’re actually helping to make sure they gave antibiotics.” Well maybe, but maybe more likely we’re helping make sure that someone actually documents correctly what’s already been done. So somebody’s been given antibiotics, but no one’s documented it yet. Our system serves as a reminder to get that done.
How much overlap is there with traditional surgery or periop systems, and who do you consider to be your competitors?
We’ve actually had discussions with some of the CEOs of the existing periop documentation systems who have told me that they don’t see it as overlapping, and they see it as a logical add-on. Yet if you talk to some of the other larger companies who, it’s all just software, right? At some level they have everything, at least on the drawing board, and they’ll tell you, “Oh yeah, we’re working on something like that.” But I don’t think any of the current well-known companies could claim to have something exactly like this running in a hospital.
Another technology that outsiders seem to be amazed that healthcare doesn’t have is real-time video and data capture for review or teaching or malpractice defense. I noticed your Historian product offers that. How are customers using that?
We’re not directly supplying video recording. What we’re doing is essentially adding automatic data bookmarking to what exists in video logging products. For example, our product is in the market with our distribution partner Karl Storz and they have a line of products called AIDA, which are video loggers. So that’s an example.
In specific instances that hospitals interfaced with other competing video logging systems that other companies do sell into the ORs, there are basically DVD recorders in many ORs replacing the video tape recorders that used to be there. But I think, as you were kind of leading towards, it’s the old-style kind of tape — label it by hand; the surgeon keeps it in his office, maybe shows a clip at a conference.
The next step, we believe, is to make the video part of a richer data record. At the very least, so that you can easily find the salient stretch of tape or image that you want. One of the problems with logging things is you end up with miles of images that nobody ever goes back and looks at. So by merging the data-oriented bookmarks of knowing when the Time Out’s done, knowing when they’re closing, knowing when the physiologic monitor first picked up the pulse-ox or whatever, you can actually rapidly scan ahead to where you want to be instead of wading through a lot of empty air time.
Final thoughts?
I think you already said it for me, but I’ll repeat it. The electronic medical record in many ways seems, from my vantage point, to be somewhat stalled in that documentation phase. It’s really taking that electronic data, fusing it from several sources, applying rules to it, and acting on it that I think starts harvesting the goodness of it and makes it more than just this added documentation burden. Instead, it makes it part of the care delivery system that we’re really excited to be part of. I’d say that’s the exciting trend that is enabled by the correct deployment of electronic records.






















































Thank you for your comments on Amazon. Agree 100%