Glen Tullman is CEO of Allscripts. Phil Pead is president and CEO of Eclipsys. This interview was conducted Tuesday evening, June 15.


Do you think it’s going to be a distraction, in the heat of HITECH and the window of opportunity that’s there, to be trying to merge two organizations?
Glen: We are already working together doing many of the things we would be doing as part of the merger. We have top clients of ours who have shared clients like Columbia, like Hartford, like North Shore – Long Island Jewish, who’ve been saying to Phil and to me, separately, “The two of your organizations need to work together to create an integrated end-to-end solution.” So we’ve been doing that in a very haphazard, unplanned way.
The beauty of this is that now we can be much more efficient. Our teams can work together, That actually saves rather than adding complication. That reduces it.
The other piece I’ll tell you is our joint sales forces now have a much broader offering, which is easier to sell, than they did prior to the merger.
The last point I’d make is that usually in a merger the technology is an issue, but the beauty here is that we’re both from an architectural standpoint. We have Microsoft .NET and other technologies that fit together very well.
So from my perspective, it’s not a distraction, it’s actually an accelerator.
Phil: I’ll just add to that by telling you that we’ve actually had one RFP process reopen after the announcement of the merger because they loved what they saw.
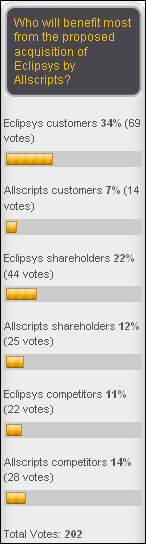
On the poll I’m running, I was surprised that the leading response of who benefits from this is Eclipsys clients, which I didn’t really expect. Does that surprise you?
Phil: I think maybe the poll views it that way, but I think it’s a great benefit for both sets of clients because as Glen mentioned, we share mutual clients today. New York Presbyterian, Columbia would be a good example of that. Obviously, North Shore, which is our largest client, has also gone with Allscripts.
I think there’s a big benefit, certainly for the Eclipsys clients who are looking to broaden the Sunrise platform out into the community, which was a big driver for us to do this deal. So many of our clients are looking to incorporate the ambulatory physicians into their environment and with the huge footprint that Allscripts has. That meant a lot to us and it obviously means a lot to our clients.
On the flip side, there are a lot of Allscripts clients who would love to create that seamless patient experience going from the ambulatory back into the inpatient. This gives Allscripts an opportunity really, now with Eclipsys, to offer an inpatient solution that ties it all together. Too many physicians used to say, “Look, I’m working in my office, I see a patient, and the next thing you know I work in the hospital and I’m using a different system and I don’t even get the data out of my existing system back in the office.” I think that probably from the poll that you’re seeing it looks that way, but frankly, I think it’s a mutual benefit for both of us.
Glen: I would just add that this is a merger, and the reason it’s a merger is because both sides benefit. What this is really about is it’s capitalizing on what today is the hottest and most important trend in healthcare, and that is hospitals are aggressively moving to capture the communities that they operate within. Hospitals have said, “We want to connect to physicians. That’s our lifeblood.”
If you think about that, each physician is worth between $1 million and $2 million to a hospital, so they want to be connected. They can’t buy all those physicians, so they want to connect with them. It would be easier to do business with them and do that electronically.
Eclipsys is tops in terms of usability in hospitals. If you believe the US News and World Report list of best hospitals, of the top 21, 18 are Eclipsys. We’ve got the top hospitals that are now going to be connected into the largest base of physician practices out in the community. It’s more than 40,000 practices.
I use the analogy — if you were starting a new bank and you came into a community and said, “I’m starting a new bank and I want to have an ATM network,” and you had a choice: should I build one, or should I connect to the ATM network that already has 40,000 locations? The choice would be, of course, connect to the network that’s already established that has 40,000 locations.
What we’ve done by putting these two companies together, we’ve created a new company that essentially has the top hospitals connected to the largest network in America of not only physicians, but ambulatory care. Post-acute care facilities, I should say. So when you talk about closing the loop of care … because at the end of the day, this is about the patient having one record and that means you pull information from the hospital, from the ambulatory world, and from the post-acute world, and you present it in one patient record. That’s what we can do today. No one else really has those capabilities all bundled together.
Both companies clearly had a reason to both hate and fear Epic. How does that change with the merger?
Glen: I don’t think it’s so much hating and fearing Epic. I think the fact of the matter is that Epic’s solution is based on 25-year-old software. They have an ambulatory system that doesn’t really work for smaller practices, and that’s half the physicians in America. It’s the equivalent of trying to put a mainframe into a two-doc office. Can we do it? You can do it. Should you do it from a cost, quality, and usability standpoint? You really shouldn’t.
This is less about fearing Epic. I mean, frankly, Epic needs to worry about what we’ve just created because this is a real solution on modern software with a real connection between usable hospital software and 40,000-plus practices that are already using at least one piece of Allscripts software, 10,000 post-acute facilities that are using it. Now you’ve got a real network. Somebody last week, one of the analysts, called it the Verizon of healthcare, which is a real connected network. For the first time, there’s software that can actually be used. I think this is going to create a very distinct competitive advantage versus an Epic.
Phil: I’d just add to that. If you just look at the healthcare marketplace, the merger will create a network of 180,000 physicians, about 1,500 hospitals, and as Glen said, 10,000 post-acute, but it actually goes beyond that, because one of the things that I think all the physicians really crave is, OK, so now I’m connected — so what?
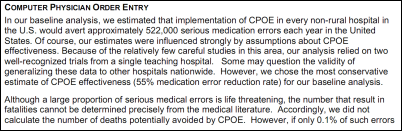
Well, the ‘so what’ is … and let me just give you a really interesting example of a client that I talked to just the end of last week. One of their biggest problems is that they track all this data, or all these hospitals do this. They showed — and this is a typical big scenario — one patient that showed up seven times over a two-year span for the same problem in the hospital. When they analyzed why that happened, this patient shows up in the hospital the first time with this problem and they’ve got the best, brightest minds with all the CPOE, the integrated environment the hospital creates, and they see this patient and they go, “I know what’s wrong with this patient,” and they follow the protocols that are already built into order entry. They’ve got their order sets, they take care of this patient, and the patient leaves.
The patient then goes back into a primary care environment and then they start to deteriorate for whatever reason. They didn’t control whatever their chronic disease was. They go to the primary care and the primary care goes, “Yup, I’ve seen this before about 30 years ago, and this is how I treat that patient.” None of the protocols that treated that patient successfully in the hospital transfer to the ambulatory environment.
So, the ‘so what’ here for us is now that we’ve got these physicians connected, our goal is to use clinical analytics and clinical decision support to take the fundamental care that patients are receiving in a hospital. When they move to a post-acute or go back to their home, all these protocols will follow with them so they’re not returning to the hospital at a higher level of acuity because they go back into an environment that doesn’t understand how to treat them.
This is the massive inefficiency that exists in our healthcare system today. What’s interesting is Medicare is going to stop that. They’re already starting at a high level, I would call it, with the Never Events. But at some point when you can look at following a protocol of care and the pathways associated with an optimal outcome that a physician doesn’t follow in an ambulatory setting that results in that patient showing up in an acute care facility and at a higher cost, someone’s going to know that. I think that’s ultimately where we’re going to get to in this bundled payment for quality reimbursement that I think we’re going to move to over the next 3-5 years.
Glen: One other thing I’d just mention. You mentioned Epic. We are both, Eclipsys and Allscripts, big believers in open systems. We’ll connect to anyone. We’re working with a variety of systems. That’s important because while our offerings will be richer and more vibrant, we are an open system and we believe that the information has to flow. That’s a very big difference from somebody like an Epic.
You mentioned in terms of the differences — again, modern software versus 25-year-old MUMPS; open versus closed; ambulatory — we have it, they don’t; and again, more of a PC versus a mainframe. When you put all that together, what’s really happened is, for the first time, the market has real choice. We think they’re going to choose this new, combined organization that we’ve created together.
Some would say the advantage of Epic is that they’re privately held and all the work that you have to do to integrate two quite different companies and two quite different sets of products has to be done under the careful scrutiny of Wall Street. Are you concerned about how long this will take and what kind of scrutiny you will get while this all takes place under the covers?
Phil: We actually love the scrutiny. We really do. I think that’s a great point, and the reason that we love it is that you’re going to be able to see the progress every quarter. When you’re a private company, you have no clue what’s going on behind the curtain. You don’t know how profitable they are; how many people they’ve got working on all the problems.
You know, I got LASIK surgery about three years ago, maybe a little longer now. The reason that I chose the company I went with was because they were public. I could read every one of their filings and see who was suing them for not doing a good job. You have no clue what goes on in a private organization.
I like the scrutiny. I think Glen does, too. I’m responsible, with Chris Perkins, for the integration. We’re going to be able to demonstrate the progress that we make, but let me just say this, and I think that Glen started off by saying it. We already have mutual clients that have merged or integrated, where we can believe that there’s a level of integration between our software.
The reason I say, ‘believe it’ is because at their level. what the user sees, what a physician uses at Columbia and that’s integrated with Sunrise, is very real to them. That level of integration has already occurred. You could talk to them tomorrow and they’ll tell you absolutely, I get whatever I need and I’m done. But that level of integration is at that first phase. We’ve made it usable, data transfers, and as far as they’re concerned, they’re done. We’d like to do it at a much deeper level, but it’s transparent to the user. That’s the first thing.
The second thing is we’re both Microsoft .NET and SQL Server. That makes the level of integration far less complex as a result of the platforms being the same, and as Glen mentioned earlier, the open architecture that we have. Allscripts has an architecture called UAI and we have Helios. The similarities are quite amazing, and of course we didn’t realize this until we started doing our diligence, but both of us have abilities to actually integrate levels of applications at a speed that would be very difficult if they were Oracle, Linux, MUMPS. It’s just fortuitous in many ways that we’ve got the similarities in the platform.
As far as the operational integration goes; again, there’s incredible complementary resources between the two companies. I won’t get in and bore you with all the details, but I will tell you that operationally, Allscripts was taking advantage of some of the back office functionality at Misys. They can now take advantage of the back office functionality of Eclipsys. It almost transfers over pretty neatly when we move the operations into a combined company.
We have substantial resources in India for development, for product support, for back office finance functions. Allscripts can take advantage of those. We’ve already mapped out — and of course, we’re going to get down into it at a far deeper level of detail now — but we’ve already mapped out exactly how the integration would work on an operational level. We’ve already started our planning an integration team on the product side.
We’re already getting excited because we’ve already been able to do stuff in just a few days because we’re actually working together, as Glen said, in an organized fashion as opposed to two companies separately sharing clients out there. We can actually do things that we never thought about doing earlier and we can do it a lot more quickly.
Glen: The timing is perfect. It’s interesting. We were just getting ready to spend millions of dollars on upgrading to a new financial system and, lo and behold, one of the choices is one that Eclipsys is already using and they have great expertise in. Now that makes that decision and saves millions of dollars. It makes the decision easy and they have the expertise to do what we would have probably struggled with. Again, when you look at some of the things we have to do, it fits together very well.
I’d also point out … you talked about being public. Being public means you have a certain discipline, and when you’re well-managed, you don’t mind that. But if you look at what we’ve created together, this is a company that’s going to be accretive in 2011. This merger is going to be accretive, number one.
Number two, we’re going to be producing $40 to 45 million per quarter free cash flow. Forty to $45 million per quarter free cash flow. And we’re talking about a synergy, cost synergies, that will ramp up to about $40 million per year. When you look at those numbers … and doing all that, our R&D spent between the two organizations will be one of the highest in the whole industry. With all of that, we can create great returns for our mutual shareholders and yet deliver world-class products.
Phil mentioned Sunrise 5.5. That’s brand new, it’s coming out. It’s been a year longer than anyone else — a year in QA and QC to make sure that this product, when it hits, is perfect, or as close to perfect as software can be. In the first installs, we’re seeing that … all that investment.
Similarly, on the Allscripts side, both our Enterprise and Professional products have been updated recently. We’ve worked through some of the kinks that we had in the Enterprise product. Professional, that came out — the full redo of that — without any issues, and it has the least number of defects, I think, of any product in the industry.
Quality products, strong financials, and a great base to draw from. We think that when you put these together… You know, the most important thing, I’d say is the genesis of this transaction. Sometimes you see companies merge and say, “Why’d they do that?” Other times you see companies merge and the clients scratch their heads. This merger was driven, in large part, by a lot of our clients, some of the most prestigious organizations in the country, who said, “The two of you belong together. This would be better for the client if you were and better for the industry.” A lot of people are frankly saying it’s wonderful to have an alternative to some of the old-time choices that they had before. We think that the clients’ reaction has been strong and we couldn’t be more excited.
There was a number given, I think, in the conference call of expected annual growth of 8-10%, which doesn’t seem all that impressive. Is that basically just under-promising and over-delivering?
Glen: Well, there’s a little bit of that, but more important, a strength of both organizations is almost 60% of Allscripts revenues — and Phil, roughly the same amount for Eclipsys? — are recurring.
Phil: That’s right.
Glen: So you’ve got this enormous base of recurring revenue because we both have such great customer bases. The problem with that … that’s great news for an investor, but on the flip side, that base doesn’t grow the way new sales grow. When you look at that, that base is probably growing kind of CPI. The base is growing 2-3%. If someone’s paying you software maintenance on their software from year to year, you’re not going to be increasing that very much because that’s so big. If that’s only growing — that huge base of 60% of your business — is growing 1-2%, to get to 10%, that means the other parts of your base have to be growing 20, 25, 30%. That’s surely true in areas like electronic health records, where our separate growth in those areas is in the 20s and 30s. Again, you have to accept it.
Phil: Yes, the metric there is really on backlog growth. As Glen said, if you remember on the Eclipsys pricing model, we sell predominantly on a subscription basis and we spread that revenue over a 5-7 year period. Unlike a Cerner, for example, that takes revenue upfront, that’s why you’re going to get a different metric. But the metric to follow is really the number of deals that we’re signing and the backlog growth that we have.
Glen: By the way, it’s better for — let’s be clear — it’s better for the clients if you balance the revenue with how they use the product, as opposed to taking a big hit upfront the day they sign it. That’s not a benefit to anybody. We actually have to do the work to get paid for it. We think that’s good for clients, and it’s good for us. It aligns us with our clients.
Probably the one consistent observation is, gosh, there are too many EMRs now under what will be the same banner. Surely some of them have to be retired. What are the thoughts about, are there too many and are there plans, preliminary or otherwise, to prune the family tree a little bit?
Phil: I love this question. It’s a great question, and I’ll tell you why I love it. It’s because the marketplace demands different kinds of solutions depending on the workflows and specialties of the physician practices and the workflows and complexities of the acute care environment.
Let’s just take the ambulatory piece, and I’ll let Glen jump in here, but if you look at our combined ambulatory EMR solutions, you’ve got MyWay — great product for the single-physician practice, simple, easy to install, allows them to keep a workflow that allows them to see a patient every 15 minutes. Primary care, they’ve got 50 codes they need to bill, and they’re in and out and done.
PeakPractice on the Allscripts side is a great product that will take the market slightly bigger than that, where they’re looking at a more complex environment, and Peak is Software as a Service. Again, it’s a great technology. It’s brand new. As you know, Eclipsys purchased that from a company the end of 2008. We’ll be able to take advantage of some of the great content now that Allscripts has and pour that into the Peak product so we’ll be able to address that next tier up in the segmentation of the physicians.
Then you’ve got the mid-tier market, so we’re looking at the 10-20 physician range, and that’s where Professional fits. Again, it takes those physician practices with a higher level of complexity, different workflows, and Professional is a perfect product for that.
Then you go into the larger-scale practices; the faculty plans, all that good stuff. That’s where Enterprise plays, and that’s where Enterprise is being very successful. Now what you need to do there is you need to do something a little different. You’ll still be able to sell Enterprise on a standalone basis because you’ll still have the large physician practices out there who may want to have a standalone, but a connection back to the hospital. But more often than not, that’s going to be a full Enterprise solution where you’ve got the content and workflows of Enterprise being integrated onto the Sunrise platform.
Again, .NET, single database, single sign-on, auditing, context management will all be built into the Eclipsys platform. So now you get a seamless environment between the owned physicians — especially if they’re at a big group level, faculty plan, and so on — back into the hospital. We see zero overlap on the ambulatory side and we see that market segmentation naturally fits into our respective product lines.
Glen: It’s interesting because if we wanted to optimize our bottom line, sure, we could only have one. I mean, Epic only has one. The problem is it doesn’t work in a one-doc or a five-doc practice. You’re trying to put a mainframe where a PC can do the job.
Phil: Which is the majority of physicians.
Glen: Yes. So they’re actually not optimized. I mean, again, look at the auto industry. You have a pickup truck, you have a minivan, you have a sports car. Imagine if somebody said to you, “Don’t you think you have too many? You have three different ones.” People would laugh. They’d say, they’re for three different uses, three different markets. Even within that, you have some variation for different specialties and the like.
There’s a reason that Eclipsys has been the leader in CPOE. There’s a reason that Allscripts has been the leader across each of the small-doc, midsize-doc, and large-doc practices in the market. That’s because we have products that fit the needs of our clients. The reality is if the clients stop buying them — you know, it’s great to speculate; for analysts and everybody else to speculate — but the fact of the matter is the clients are buying them and they’re buying them in record numbers.
If you look at our numbers from last quarter, last quarter we actually raised our guidance on bookings, on sales. Then, one quarter later, as you heard our CFO Bill Davis report when he announced this merger one quarter later, we’ve substantially exceeded the guidance we had given one quarter earlier for sales. Why did we do that? Because the clients are buying. They like the offerings that we have.
Ultimately, at the end of the day, people can speculate, but I like to use the metric of who’s buying the most. Where we see that, the clients are buying. We feel like the strategy works and that’s, I think, the best vote in the marketplace.
Phil: One more point, not to bore you to death here, but Sunrise Ambulatory Care, for example, on the Eclipsys side, will benefit hugely from the richness of the content that Allscripts has built up over the years. Again, if you’ve followed Eclipsys, we have really great clients using Sunrise Ambulatory and we’ve made, I think, a huge market out of the oncology area. Now we’ll be able to really address a lot of the other ambulatory specialties which will benefit from that content and workflow out of the enterprise.
So when we talk about too many, we’ve actually got a perfect number, and we’re going to be looking to integrate back onto the Sunrise platform at the top end; and then work our way down through the segmentations. But every single one of those products will connect back to the hospital at whatever level of integration the hospital desires and the physician desires.
Glen, you mentioned some of the analysis commentary. When you look at what you’ve read after the announcement, both from the analyst perspective and from the industry perspective; are there aspects of what people have said that you think are either unfair, or that they’ve missed key points about why you’re doing this?
Glen: I think that generally, the industry has understood, the analysts have understood, the investors have understood the strategic rationale. I think everyone buys into that. I think where people have had some confusion is the structure of the agreement. That is, why is Misys, who owns 55%, selling, and how is it structured?
The reality is there’s a technical rule on the London Stock Exchange where Misys PLC is traded. That says if you’re going to make an investment, you either have to control that investment, or it has to be de minimis. To translate that in rough terms, you either have to have more than 50% or less than 10%.
Because of that, when we came along and our Board looked at this and said, “It is a perfect fit here for Allscripts and Eclipsys to come together,” we looked at that and we said, “Boy, the way to do this is to use stock for this transaction, because that way, the Eclipsys shareholders and the existing Allscripts shareholders all benefit from this new, combined organization that we’re going to create.” So that was the way to do it.
The problem is if you use stock to facilitate this merger, then all of a sudden the shared ownership of Misys PLC would drop down to 40%. That’s not allowed, because now they don’t control the asset and it’s not less than 10%. They were faced with a decision: should they invest hundreds of millions of dollars more in that company or should they use the opportunity to give their shareholders $1.3 billion back, keep 8% of the company, and allow us to move forward strategically in a way that best suits our own shareholders?
I think they made a very good decision. That decision is good for their shareholders. They have a billion dollars. That decision was good for Allscripts. The shareholders have a better position than ever. That decision benefits the Eclipsys shareholders because they’re going to, from this combined company, they’re going to have a larger, stronger platform to work with.
I think it was a smart decision, but I think there’s been some confusion because people don’t understand the intricacies of the London Stock Exchange and why Misys was essentially forced to either divest a large portion of their holdings or invest hundreds of millions of dollars more to keep their share above 50%.
I think that’s the most confusing part of what is otherwise a very strategic and understandable transaction. I mean, in today’s world, if you look at this, we’re combining two companies in what is one of the hottest, fastest-growing areas in the largest sector of our economy, and that’s healthcare. It is a $30-billion government stimulus being injected, and getting that money is all based on utilization. Just taking the two companies that are the leaders in utilization, Eclipsys in CPOE and Allscripts in the ambulatory area, and we’ve combined them to create a new powerhouse in this area of healthcare that is going to change the way healthcare is driven in America.
If I were going to grade the two of your performances, let’s say two years after the acquisition closes, what should my criteria be?
Phil: Let me start, and I’ll tell you from a shareholder perspective, I would like to see you grow the top line and prove your earnings per share leverage over that period. If I was a client, I would grade you by the integration between the product solutions to make this a great experience for their hospital and ambulatory environments so that the two came together. If you were looking at it from the employees, I would want to say that the next few years will be some of the most exciting with all the new opportunities they have to plan. Of course, the employee part you know you’ll get because employees love to share their rumors and stuff like that.
Then, finally, I’d tell you that the folks who I think are going to benefit the most from this will be the patients. Too often they’re the ones who get left out in any of these merger discussions, but ultimately, our goal — Glen’s goal, my goal — is to bring to healthcare what we’ve all wanted as individuals. That is, that wherever we receive care, by whatever specialists we see, whatever primary care physician we see, whatever hospital we go to, I won’t have to deal with the triplicate forms. I won’t have to deal with the duplicate tests. I won’t have to deal with an environment where physicians have no clue who I am.
Restaurants today, with OpenTable.com, have more information on me as somebody just sitting down to dinner than a physician has one me looking at me and my health, my life. If Glen and I can truly change that in the next two years by what we’re doing, then frankly, I think this has all been really worthwhile.
Glen: There is nothing I can add to that, which is rare for me, but I think that summarizes it perfectly.
Is there anything I didn’t ask you that you want to talk about or any concluding thoughts?
Glen: I’d just say that it’s really a privilege — and I think both Phil and I feel this way — to have this opportunity to provide a connected system of health that really gives an integrated, end-to-end solution, which is what everyone has been … that’s been the Holy Grail of healthcare, and it is within reach.
We’re in the perfect storm of all the reasons that people should change. The financials are there, the need is there, physicians are ready, the software is ready. This is the most exciting time in healthcare that we’ve ever had. We feel, like sitting on top of this new organization, we have a very unique opportunity and it’s a great opportunity, as Phil said, for all of the stakeholders in healthcare.






















































Thank you for your comments on Amazon. Agree 100%