Top News

HHS announces its Accountable Care Organization rules (Medicare Shared Savings and the Advance Payment Model.) Some differences between the preliminary and final versions:
- Quality measures reduced from 65 to 33
- Use of an EHR is not a requirement to participate
- Introduction of a savings-only track without financial risk during the initial contract period
- CHCs and rural health clinics now have an option to lead ACOs
- A longer phase-in for reporting and performance measures
- Multiple start dates established
- CMS will provide approved marketing guidelines and language (so ACOs don’t have to wait for CMS approval, as was stated in prelim)
Reader Comments

 From EHR Geek: “Re: Joel Diamond. I love your posts so much that sometimes I feel like a stalker. With the current healthcare environment, it seems like you could make so much more money (just by dropping your malpractice alone) by doing standup comedy. Please?” Like EHR Geek, I love Dr. Diamond’s posts, which I find laugh-out-loud funny. This week, he discusses all that is good in healthcare. The topic only sounds benign.
From EHR Geek: “Re: Joel Diamond. I love your posts so much that sometimes I feel like a stalker. With the current healthcare environment, it seems like you could make so much more money (just by dropping your malpractice alone) by doing standup comedy. Please?” Like EHR Geek, I love Dr. Diamond’s posts, which I find laugh-out-loud funny. This week, he discusses all that is good in healthcare. The topic only sounds benign.
 From WhatTheDell: “Re: resignation. Jim Fitzgerald recently resigned from Dell’s Meditech Solutions Group. Big loss given his role of all things Meditech.” Unverified. There is no change in his LinkedIn profile or on Dell’s “About Us” page.
From WhatTheDell: “Re: resignation. Jim Fitzgerald recently resigned from Dell’s Meditech Solutions Group. Big loss given his role of all things Meditech.” Unverified. There is no change in his LinkedIn profile or on Dell’s “About Us” page.

 From Colorado Kid: “Re: University of Colorado Hospital. Went live on Epic in September, including physician documentation, CPOE, RN barcoding and charting, OR, anesthesia, inpatient pharmacy, labor and delivery, radiology, and ED. Outpatient clinics are 70% deployed, to be completed with Beacon oncology and Phoenix transplant by mid-2012.”
From Colorado Kid: “Re: University of Colorado Hospital. Went live on Epic in September, including physician documentation, CPOE, RN barcoding and charting, OR, anesthesia, inpatient pharmacy, labor and delivery, radiology, and ED. Outpatient clinics are 70% deployed, to be completed with Beacon oncology and Phoenix transplant by mid-2012.”
 From Lady Pharmacist: “Re: National Pharmacy Week, October 16-22. It’s time for the annual shout-out for pharmacists and pharmacy technicians. Healthcare informatics plays a vital role with and for these clinical and medication distribution folks who make medication usage safe in our institutions!” As I usually say, a hospital is a very clean hotel that offers only three interventions: surgery, treatments, and drugs. Pharmacists and techs manage that last set of interventions with extraordinary skill given the complexity involved (not to mention that most of the country is taking a plethora of pills – a new study found that 11% of Americans over the age of 12 take antidepressants, which is in itself depressing.) Congratulations to those folks behind the counters, down in the basement, and (increasingly) out on the floors.
From Lady Pharmacist: “Re: National Pharmacy Week, October 16-22. It’s time for the annual shout-out for pharmacists and pharmacy technicians. Healthcare informatics plays a vital role with and for these clinical and medication distribution folks who make medication usage safe in our institutions!” As I usually say, a hospital is a very clean hotel that offers only three interventions: surgery, treatments, and drugs. Pharmacists and techs manage that last set of interventions with extraordinary skill given the complexity involved (not to mention that most of the country is taking a plethora of pills – a new study found that 11% of Americans over the age of 12 take antidepressants, which is in itself depressing.) Congratulations to those folks behind the counters, down in the basement, and (increasingly) out on the floors.
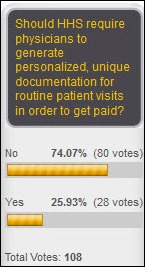
 From MM: “Re: Dr. Jayne on cloned documentation. Did we really expect anything else? If you have been around medical reimbursement rules for any amount of time, you know that when the rules begin to be met by the majority of providers, the rules will change. It is really all about who gets to keep the money. We used to bill by diagnoses, then by time, now by documentation. All these rules were created by the insurers, and each time we achieve competence at following the billing rules, they change them.” I’ve said that for years. Payment is a shell game, where there isn’t enough money to stick under every shell. It is inevitable that when some individual or group starts winning too often, the dealer will move the shells around and change the rules, sometimes drastically altering the lifestyles of professionals along the way (nurse anesthetists and physical therapists come to mind if you look back 25 years or so). That’s really the problem with healthcare – providers flock to profitable services like bugs to a zapper, but patients don’t usually benefit. Expecting healthcare providers, even theoretically non-profit hospitals, to just keep doing the same work without regard to what they’ll get paid is just silly.
From MM: “Re: Dr. Jayne on cloned documentation. Did we really expect anything else? If you have been around medical reimbursement rules for any amount of time, you know that when the rules begin to be met by the majority of providers, the rules will change. It is really all about who gets to keep the money. We used to bill by diagnoses, then by time, now by documentation. All these rules were created by the insurers, and each time we achieve competence at following the billing rules, they change them.” I’ve said that for years. Payment is a shell game, where there isn’t enough money to stick under every shell. It is inevitable that when some individual or group starts winning too often, the dealer will move the shells around and change the rules, sometimes drastically altering the lifestyles of professionals along the way (nurse anesthetists and physical therapists come to mind if you look back 25 years or so). That’s really the problem with healthcare – providers flock to profitable services like bugs to a zapper, but patients don’t usually benefit. Expecting healthcare providers, even theoretically non-profit hospitals, to just keep doing the same work without regard to what they’ll get paid is just silly.
HIStalk Announcements and Requests
 I am heading to MGMA in Las Vegas this weekend and will be posting updates on some of the action. If you are attending, be sure to take a look at HIStalk’s Must-See Vendors for MGMA 2011. The guide includes some tips on vendor giveaways (hint: you don’t want to miss a visit to Allscripts, MED3OOO, and Culbert Healthcare.) And if you see one of these desktop signs in a vendor’s booth, please take a moment and thank them for supporting HIStalk, HIStalk Practice, and HIStalk Mobile.
I am heading to MGMA in Las Vegas this weekend and will be posting updates on some of the action. If you are attending, be sure to take a look at HIStalk’s Must-See Vendors for MGMA 2011. The guide includes some tips on vendor giveaways (hint: you don’t want to miss a visit to Allscripts, MED3OOO, and Culbert Healthcare.) And if you see one of these desktop signs in a vendor’s booth, please take a moment and thank them for supporting HIStalk, HIStalk Practice, and HIStalk Mobile.
 Listening: reader-recommended The Heard, rootsy Southern rockers from Reading, PA. Sounds kinds of Allmans-meet-R.E.M. to me. Also reader-recommended: BluesMotel, some guys from the Netherlands that play Chicago blues. I can almost smell the smoke and beer.
Listening: reader-recommended The Heard, rootsy Southern rockers from Reading, PA. Sounds kinds of Allmans-meet-R.E.M. to me. Also reader-recommended: BluesMotel, some guys from the Netherlands that play Chicago blues. I can almost smell the smoke and beer.
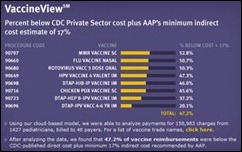
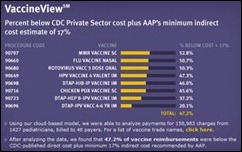
 This week on HIStalk Practice: in addition to our MGMA guide and a post from Dr. Joel Diamond, athenahealth reports that pediatricians are under-reimbursed for certain vaccines almost half the time. CalOptima REC names its preferred EHR vendors. The Department of Pathology at the Medical City Dallas Hospital (TX) goes with McKesson for billing and RCM. Emdeon expands the capabilities of its Office Suite solution. Radiology Medical Group (CA) announces plans to outsource its billing and lay off 24 employees. If you are interested in the ambulatory HIT world, highlights from MGMA, shoe fashion, and/or Inga’s mental health, please sign up for e-mail updates while visiting HIStalk Practice. Thanks for reading.
This week on HIStalk Practice: in addition to our MGMA guide and a post from Dr. Joel Diamond, athenahealth reports that pediatricians are under-reimbursed for certain vaccines almost half the time. CalOptima REC names its preferred EHR vendors. The Department of Pathology at the Medical City Dallas Hospital (TX) goes with McKesson for billing and RCM. Emdeon expands the capabilities of its Office Suite solution. Radiology Medical Group (CA) announces plans to outsource its billing and lay off 24 employees. If you are interested in the ambulatory HIT world, highlights from MGMA, shoe fashion, and/or Inga’s mental health, please sign up for e-mail updates while visiting HIStalk Practice. Thanks for reading.

 Thanks to NexJ Systems of Toronto, ON, now supporting HIStalk as a Platinum Sponsor. The company is all about eHealth, offering its Health Information Exchange solution that includes its Universal Health Connector (global messaging and controlled vocabularies and terminology) to facilitate interoperability among providers, ACOs, payors, and public health agencies. They also offer tools for chronic disease management, disease registry, electronic referrals, patient portal, provider credentialing, and a wellness platform. Other offerings include platforms for provider health, consumer health, and analytics. Click the image above to check out their October 28 Webinar on next-generation, open-architecture HIE technologies that are fast, flexible, and cost effective. Thanks to NexJ for supporting HIStalk and its readers.
Thanks to NexJ Systems of Toronto, ON, now supporting HIStalk as a Platinum Sponsor. The company is all about eHealth, offering its Health Information Exchange solution that includes its Universal Health Connector (global messaging and controlled vocabularies and terminology) to facilitate interoperability among providers, ACOs, payors, and public health agencies. They also offer tools for chronic disease management, disease registry, electronic referrals, patient portal, provider credentialing, and a wellness platform. Other offerings include platforms for provider health, consumer health, and analytics. Click the image above to check out their October 28 Webinar on next-generation, open-architecture HIE technologies that are fast, flexible, and cost effective. Thanks to NexJ for supporting HIStalk and its readers.
 Pardon me while I communicate in techo-gibberish with my fellow geeks (non-nerds, hands over ears, please). You may have noticed that HIStalk loads faster now. Reason: I replaced Apache with the Litespeed WebServer. It’s hard to picture a Web server that’s running *NIX without Apache, but you’re soaking in it. I also had the PHP handler changed from DSO to SUPHP to improve security and to fix some CHMOD problems. (end of nerdspeak)
Pardon me while I communicate in techo-gibberish with my fellow geeks (non-nerds, hands over ears, please). You may have noticed that HIStalk loads faster now. Reason: I replaced Apache with the Litespeed WebServer. It’s hard to picture a Web server that’s running *NIX without Apache, but you’re soaking in it. I also had the PHP handler changed from DSO to SUPHP to improve security and to fix some CHMOD problems. (end of nerdspeak)

 October is Breast Cancer Awareness Month, meaning it’s time to watch those cool Pink Glove Dance videos. My favorite so far is from Victoria Hospital – Prince Albert Parkland Health Region, Prince Albert, Saskatchewan (although they’ve disabled putting the video directly on HIStalk this time around, so you’ll have to click.) Check out all great videos and vote for your favorite here.
October is Breast Cancer Awareness Month, meaning it’s time to watch those cool Pink Glove Dance videos. My favorite so far is from Victoria Hospital – Prince Albert Parkland Health Region, Prince Albert, Saskatchewan (although they’ve disabled putting the video directly on HIStalk this time around, so you’ll have to click.) Check out all great videos and vote for your favorite here.
 On the Jobs Board: Senior Business Analyst – Salesforce.com, HL7 Interface Developer, Account Manager. On Healthcare IT Jobs: Director – Epic and Clinical Systems, Security Engineer, Business Continuity Analyst, Clinical Nurse Analyst.
On the Jobs Board: Senior Business Analyst – Salesforce.com, HL7 Interface Developer, Account Manager. On Healthcare IT Jobs: Director – Epic and Clinical Systems, Security Engineer, Business Continuity Analyst, Clinical Nurse Analyst.
 Don’t let Inga’s swaggering online demeanor fool you. Those of us who know her recognize that she’s sensitive (sniffles at movies), self-doubting (always convinced she doesn’t know enough to write authoritatively about topics she’s followed for many years), and fragile (I’ve quit telling her to stop double-spacing after a period because it devalues her). You can imagine the emotional harm wreaked by those who don’t sign up for e-mail updates; who fail to connect with us on LinkedIn and Facebook; who don’t support our sponsors and click their ads and Resource Center listings occasionally; and who hurtfully neglect to send her newsworthy scoops and fun information so she can at least temporarily feel confident about her knowledge base (cue emotion-tugging Sarah McLachlan warbling). In lieu of giving her a hug, consider checking off the items on the list above, ‘cause when Mama ain’t happy, ain’t nobody happy.
Don’t let Inga’s swaggering online demeanor fool you. Those of us who know her recognize that she’s sensitive (sniffles at movies), self-doubting (always convinced she doesn’t know enough to write authoritatively about topics she’s followed for many years), and fragile (I’ve quit telling her to stop double-spacing after a period because it devalues her). You can imagine the emotional harm wreaked by those who don’t sign up for e-mail updates; who fail to connect with us on LinkedIn and Facebook; who don’t support our sponsors and click their ads and Resource Center listings occasionally; and who hurtfully neglect to send her newsworthy scoops and fun information so she can at least temporarily feel confident about her knowledge base (cue emotion-tugging Sarah McLachlan warbling). In lieu of giving her a hug, consider checking off the items on the list above, ‘cause when Mama ain’t happy, ain’t nobody happy.
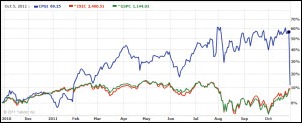
Acquisitions, Funding, Business, and Stock
TransUnion acquires Financial Healthcare Services, a provider of a patient payment estimation solution.

Microsoft announces Q1 numbers: revenue up 7%, EPS $0.68 vs. $0.62, beating and meeting expectations, respectively.

Athenahealth announces Q3 numbers: revenue up 33%, EPS $0.15 vs. $0.11, beating expectations on both and raising fiscal year guidance.

 San Diego’s West family, who made their $2 billion fortune from telemarketing and who established the West Wireless Health Institute in 2009, create a $100 million venture investment fund to invest in early-stage technology companies that can reduce healthcare costs. They pledge to invest any profits in medical research.
San Diego’s West family, who made their $2 billion fortune from telemarketing and who established the West Wireless Health Institute in 2009, create a $100 million venture investment fund to invest in early-stage technology companies that can reduce healthcare costs. They pledge to invest any profits in medical research.
Sales
Alexian Brothers Health System (IL) expands its relationship with athenahealth by selecting athenaClinicals and athena Communicator for its network of 150 employed providers. In addition, athenaCollector client Harbin Clinic (GA) adds athenaClinicals for its 210 providers. Both are Allscripts replacements.
People
The Hay Group consulting firm promotes Bill Quirk from director of business development to national director of its US healthcare practice. He was previously with Sullivan, Cotter and Associates and Towers-Perrin.

The TriZetto Group names President and CEO Trace Devanny as the company’s chairman, succeeding TriZetto founder Jeff Margolis, who will serve as chairman emeritus. Devanny was president of Cerner until last year.

Streamline Health hires Tom Dean, formerly with CareCentric, as VP of product engineering.

Robert J. Bunker joins the board of directors of T-System. He is chairman and CEO of The Medical Staffing Network Inc. and started his work in healthcare as Humana’s COO in 1994 after serving 20 years in the US Air Force Medical Service, retiring with a rank of lieutenant colonel.

Joan Bishop, formerly with Lockeed Martin, joins Encore Health Resources as principal of its government client services business.
Announcements and Implementations

AtlantiCare (NJ) announces plans to to launch AtlantiCare Health Solutions, an accountable care organization.
 Aprima Medical certifies GFI Software’s FaxMaker for use with Aprima’s EHR and PM solutions. Which reminds me of a recent need I had for a copy of certain medical records. My doctor’s office said I had to fax them a request form. Since I don’t have a fax machine, I asked if I could e-mail the form. They responded that they didn’t have e-mail. I had to double check the year to make sure I wasn’t in some sort of time warp.
Aprima Medical certifies GFI Software’s FaxMaker for use with Aprima’s EHR and PM solutions. Which reminds me of a recent need I had for a copy of certain medical records. My doctor’s office said I had to fax them a request form. Since I don’t have a fax machine, I asked if I could e-mail the form. They responded that they didn’t have e-mail. I had to double check the year to make sure I wasn’t in some sort of time warp.
ONC validates the South East Michigan Health Information Exchange (SEMHIE) for conformance and interoperability testing, allowing SEMHIE to go live on the Nationwide Health Information Network Exchange.
Intelerad Medical Systems launches InteleSuite, a RIS/PACS solution that combines Interad’s standalone PACS and RIS offerings.
University of Michigan Health System and Great Lakes Health Information Exchange sign an agreement to exchange information. Other members are Michigan State and Sparrow Health System.

 A Detroit jury finds that Beaumont Hospital (MI) and an OB doctor let a woman deliver a 10-pound, 12-ounce baby vaginally instead of by C-section, causing brain injuries in the newborn girl. Despite the hospital’s claim that the disabilities of the child (now a teenager) were caused by the mother’s gestational diabetes, the jury awards the family $144 million.
A Detroit jury finds that Beaumont Hospital (MI) and an OB doctor let a woman deliver a 10-pound, 12-ounce baby vaginally instead of by C-section, causing brain injuries in the newborn girl. Despite the hospital’s claim that the disabilities of the child (now a teenager) were caused by the mother’s gestational diabetes, the jury awards the family $144 million.
 I received an e-mail from Steve Pelton, VP of enterprise applications for Ministry Health Care (WI). They have completed their EHR certification tests through Drummond Group (“tough, but fair,” he says) and expect to demonstrate Meaningful Use and attest early next year after the 90-day demonstration period. He raises an interesting point:
I received an e-mail from Steve Pelton, VP of enterprise applications for Ministry Health Care (WI). They have completed their EHR certification tests through Drummond Group (“tough, but fair,” he says) and expect to demonstrate Meaningful Use and attest early next year after the 90-day demonstration period. He raises an interesting point:
From the CHPL web site, it appears that only 16 hospital and health systems have achieved either modular or complete EHR certification. While many or even most hospitals will wait for their vendors to provide updated, certified products for them to install, it does seem surprising that so few of the over 5,000 hospitals in the US have not gone through the self-certification process. Like Ministry Health Care, most of the 16 hospital and health systems achieved modular certification, which allows for the Meaningful Use of a collection of certified products. The most common modules that are self-certified seem to be homegrown data repositories. One would expect that many hospitals that have either homegrown systems or uncertified niche systems would attempt to certify them. One would also expect hospitals to self-certify their existing systems while they are working to replace or upgrade to a certified version. What is everyone waiting for?

 Weird News Andy summarizes this story as, “Socialized medicine. Gotta love it.” An 82-year-old woman visiting her dying husband in a Canadian hospital falls in its lobby, breaking her hip. Two ED nurses and a security guard observe her lying face-down on a metal grate and bleeding, but refuse to help until an ambulance arrives. The top executive can’t explain why a code wasn’t called. The same hospital made headlines last year when a woman who had stopped breathing was driven to the hospital by her boyfriend, but the ED staff refused to help since the couple were in their car in the parking lot and told the boyfriend to call 911 instead. The 39-year-old woman died a few days later of a heart event. The employees thought they wouldn’t be covered by malpractice insurance if they helped someone outside the four walls of the hospital.
Weird News Andy summarizes this story as, “Socialized medicine. Gotta love it.” An 82-year-old woman visiting her dying husband in a Canadian hospital falls in its lobby, breaking her hip. Two ED nurses and a security guard observe her lying face-down on a metal grate and bleeding, but refuse to help until an ambulance arrives. The top executive can’t explain why a code wasn’t called. The same hospital made headlines last year when a woman who had stopped breathing was driven to the hospital by her boyfriend, but the ED staff refused to help since the couple were in their car in the parking lot and told the boyfriend to call 911 instead. The 39-year-old woman died a few days later of a heart event. The employees thought they wouldn’t be covered by malpractice insurance if they helped someone outside the four walls of the hospital.
Government and Politics
ONC adds a principal deputy position to its organization, tasked with duties similar to that of a COO in the private sector. The yet-unnamed deputy will report to ONC coordinator Farzad Mostashari.
The VA gives Harris Corp. a two-year, $200 million blanket purchase agreement to develop VistA-connected outreach tools, including creating a point-of-service kiosk, redesigning the VA’s quality Web site, supporting the National Utilization Management Integration project, and developing a replacement bed management system.

The government’s Substance Abuse and Mental Health Services Administration (SAMHSA) awards 29 grants totalling $25 million over three years to increase access to behavioral health services with information technology.

Federal prosecutors file an $8.1 million fraud suit against Kernan Hospital (MD), part of the University of Maryland Medical System. The government says the hospital intentionally changed its billing system to create a diagnosis of severe malnutrition, looking for the words “protein malnutrition” and pressuring physicians to add that condition as a secondary disease.
Other

Nearly 300 GE Healthcare employees in Salt Lake city form a human pink ribbon in recognition of Breast Cancer Awareness Month. The company has scheduled similar displays across a couple of dozen cities.

The hospital EHR market is expected to peak in 2012, with revenues of $6.5 billion.

Twenty-six percent of CHIME CIOs say their organizations have qualified to receive Meaningful Use funding, with 13% actually having been paid. About 93% expect to achieve the Stage 1 MU during the first three years of the program.
 An Internet outage in a small North Carolina town leaves a medical practice that uses a Web-based EMR out of luck. “We’re electronic medical records, and neither one of our softwares will come up because we’re Internet-based. If the Internet goes down, we have to just call patients back to get appointments re-scheduled.”
An Internet outage in a small North Carolina town leaves a medical practice that uses a Web-based EMR out of luck. “We’re electronic medical records, and neither one of our softwares will come up because we’re Internet-based. If the Internet goes down, we have to just call patients back to get appointments re-scheduled.”
 An Illinois physician claims his health system employer placed him on administrative leave because he has “no computer skills.” Steven Kottermann MD, who was a family physician with Memorial Health System, admits that he fell behind on his electronic charting after the health system’s implementation of Epic. The doctor believes that Memorial is at fault because “they bought a lousy system.” The hospital’s chief medical officer says the issues go beyond the doctor’s EMR proficiency.
An Illinois physician claims his health system employer placed him on administrative leave because he has “no computer skills.” Steven Kottermann MD, who was a family physician with Memorial Health System, admits that he fell behind on his electronic charting after the health system’s implementation of Epic. The doctor believes that Memorial is at fault because “they bought a lousy system.” The hospital’s chief medical officer says the issues go beyond the doctor’s EMR proficiency.
Sponsor Updates

- GE Healthcare recognizes Frederik Memorial Hospital (MD) and Northeast Georgia Medical Center (GA) as winners of its 2011 Leaders of Change Awards at the Centricity Perinatal Users’ Group National Conference.
- Sentry Data Systems earns a spot on the South Florida Business Journal’s Top 25 Fast Tech Awards for significant revenue growth.
- Khalid Moidu, MD, PhD (Orlando Health) and Stephen Claypool, MD (Wolters Kluwer Health) will present Innovation Lab: Evidence Based Order Sets Tools from a Dynamic Hospital-Vendor Partnership at AMIA 2011.
- NVISION Laser Eye Centers (CA) selects NextGen for its 10 eye centers.
- NexJ Systems will host a free Webinar entitled The Next Generation of Health Information Exchange October 28th. NexJ Systems, by the way, was recently named the sixth fastest-growing company in North America on Deloitte’s 2011 Technology Fast 500.
- AdvancedMD receives the Healthcare Hero Award for Innovation from Utah Business Magazine.
- OptumInsight releases a guide for physicians to minimize security risks entitled Keep Patient Data Secure: Simple Actions for a Digital World.
- dbMotion and Allscripts will co-host a webinar on physician EHR connectivity on November 16th featuring dbMotion CMIO Joel Diamond MD and Ryan Winn, VP and CIO of MidMichigan Health.
- Perceptive Software will showcase its enterprise content management solutions at the Gartner Symposium/ITexpo in Spain.
- Newton-Wellesley Radiology Associates (MA) boosts its financial performance and prepares for ICD-10 using McKesson’s Revenue Management Solutions.
EPtalk by Dr. Jayne
Now that we’re in the last quarter of 2011, Physician Quality Reporting System (the artist formerly known as PQRI) data is available through the CMS quality portal. Groups can access data by taxpayer ID and individual providers can also request reports based on their NPI. Next year should be a little different, with CMS agreeing to provide interim feedback reports to those who use claims-based reporting. Too bad for those of us who are Meaningful Users of our EHR technology and are reporting through registries rather than claims.
Speaking of CMS, regulatory reforms are on the table, with two proposals being introduced and a third being finalized this week. Modifications to the Medicare Conditions of Participation would allow multi-hospital systems to have a single governing body for multiple hospitals rather than requiring each have its own governance structure. Hopefully combining governance structures will help those of us on staff at multiple hospitals within a health system to reduce the number of committees on which we are forced to serve.
Proposed modifications for non-hospital providers address durable medical equipment suppliers and dialysis providers. Also addressed are outdated e-prescribing technical requirements. Hiding towards the end of the document is language to end the use of the term “Medicaid recipient” and replace it with “Medicaid beneficiary.” Although this makes it parallel Medicare, I can’t help but think there are political games afoot, with this being one more move to make people think that Medicaid is insurance rather than an entitlement program.
We all know we live in a society that’s increasingly saturated by technology, specifically audiovisual media. The American Academy of Pediatrics Council on Communications and Media releases guidelines stating that children under age two should avoid television viewing. This also includes passive viewing while playing in a room where an adult or sibling may be watching.
There’s an app for that: Mobile MIM is one of a growing number of apps to receive FDA approval. It allows viewing of diagnostic images, including MRI and CT scans. Although the app (one version for physicians, one for patients) is free, physicians must pay $1 to upload each image to its cloud-based repository. Viewing the study costs $1 to $2 depending on the receiving device. Earning FDA approval took more than two years and included modification to the app to detect poor lighting conditions that are inappropriate for the interpretation of radiologic studies. Maybe the FDA should also include logic to detect whether it is being used in a bar, as my colleague was attempting.
Recent data from social media analytics firm Amplicate shows that over the last year, 69% of Facebook and Twitter users reported hating a particular insurance carrier. Data from over 2,500 posts is aggregated by payer. In contrast, the other industries the firm tracks were more positive, with 56% of users loving their grocery store chain and a 70% expressing a love connection for fast food chains. More negative than health insurers: banks.
The FDA approves Hologic’s Trident specimen radiography system. The system is designed for intraoperative specimen imaging during minimally-invasive, stereotactic, or ultrasound-guided breast biopsies and includes the ability to export to PACS.

October is Breast Cancer Awareness month. I first saw the Pink Glove Dance on HIStalk. It’s always good to see healthcare workers having fun and raising awareness about a disease that impacts so many people. More than 100 organizations are competing for thousands of dollars to donate to their favorite charities, so get out there and vote. Here’s a shout out to my co-workers who are fighting this disease and a special nod to all the women in my family who have beat it, including one 20+ year survivor. Love you, Mom!

Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.

































































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…