Curbside Consult with Dr. Jayne 8/12/24
I’ve spent my entire career in healthcare and healthcare IT. I have worked in a number of settings, from small private practices to large health systems, and from startup technology organizations to major EHR vendors. In every one of those settings, the need for teamwork has been emphasized. When you work in a patient care organization, you learn that there are dozens of teams that support patient care, whether directly or indirectly. There are the frontline clinicians, but there are also people in engineering, environmental / housekeeping, supply chain, finance, and more. When you’re working a clinical shift in the hospital, how those teams function can be highly variable.
Where I trained as an intern, we were assigned to teams that rotated the responsibilities for accepting admissions and working up patients who were newly admitted to the hospital. However, we really didn’t function as a team. Each intern was assigned individual patients to care for, and a supervising resident oversaw the activities of the interns on the team. We were only a team in as much as we had similar working schedules for the days we took call. The work was much more individual, even down to the fact that when one intern finished they could go home, while other interns might be knee deep caring for extremely ill patients. In hindsight, after going through formal education on team dynamics, it would have been more accurate to refer to us as an “on-call cohort” rather than an “on-call team.”
I’ve seen that cohort concept play out among nurses who are working a shift on the same unit, where one member of the “team” might be assigned a disproportionate share of the work for a variety of reasons. One of my favorite nurses texted recently about a shift where there was a need to pull nurses away from nursing tasks to serve as sitters for patients that had been identified as having a high risk of falls, disorientation, or self-injury. Instead of figuring out a way to divide the work throughout the 12-hour shift, one nurse was assigned all of the nursing patients for the entire shift, and other nurses were assigned to be sitters for the entirety of the shift.
Since being a sitter is perceived as being an easier job by many, there wasn’t any incentive for people to volunteer to divide the work any other way, such as creating two six-hour nursing blocks and two six-hour sitting blocks, so that the work could be more evenly distributed. It’s difficult to feel like you’re a member of a team when you also feel like you’re the one that has been left holding the proverbial bag for all the patients on the unit, all by yourself.
I experienced a lot of non-team “teamwork” during the height of the pandemic when working in emergency and urgent care settings. Sometimes it just happens because of the varying levels of acuity of patients as they come through the doors, and chance determines whether you wind up with a patient who is relatively straightforward or whether you wind up with one who is extremely ill. While some facilities have algorithms to try to even out those patient loads, others work on a strict rotation that determines who is responsible to pick up the next patient that arrives. The combination of different types of patients you are responsible for often determines whether a shift is perceived as easy or hard, as does the makeup of your support team. When you have a team that clicks, it can make things seem much more tolerable, and it’s that feeling of teamwork that can get you through.
Unfortunately, that feeling of teamwork was also exploited during the busiest parts of the pandemic, as workers were forced to work while sick and when they were at the point of exhaustion. They were pushed to their breaking points and felt like they had to keep going because there was no one else to take their place, and that’s not a situation that anyone wants to be placed in again. That negative application of teamwork – the pressure that you have to do something because “you can’t let the team down” – led to many of my colleagues leaving direct patient care roles as the pandemic’s demands began to decrease. Unfortunately, I continue to see people who are asked to work under poor conditions with “the good of the team” being cited as a reason.
I recently had the chance to observe a technology team where members were not only cross trained, but were intentionally grouped to ensure redundancy. In the event of illness or competing priorities, the team was resourced so that responsibilities could be shifted to multiple other team members, reducing the risk that any one member would feel that work was being dumped on them should someone need to step back due to illness or personal conflicts. Part of the need for redundancy was inherent in the kind of work being done, which involved life support for individuals working in a hazardous environment. But it got me thinking about why we don’t take more of that kind of approach in healthcare. Certainly our patients, who are someone’s mothers, brothers, sisters, fathers, or other loved ones, deserve to have care delivered via processes that don’t allow them to fall through the cracks.
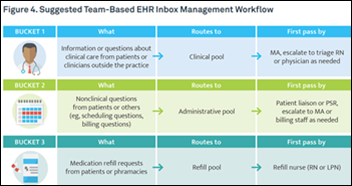
Why do so many care delivery organizations still use what could be described as single-threaded staffing models? For example, one physician, or one nurse, or one patient care technician is assigned to a certain number of patients. What would it be like if we cared for patients in groups, with backup and redundancy? Would we benefit from having more immediate collaboration around how we approach a patient in front of us? You see this in academic centers, where you may have physicians at different levels caring for a patient, such as an intern, a resident, a fellow, and an attending physician. Sometimes one will see something that another didn’t, which can lead to better outcomes for the patient.
I know some organizations are trying to do this in the nursing realm, using new models such as virtual nursing to provide additional layers of support for nurses working on hospital inpatient units. Sometimes the virtual nursing model carves out certain care tasks — such as intake and discharge functions that can be appropriately delivered via virtual modalities — and sometimes it’s more of a virtual mentor model to provide an extra set of eyes for nurses who may have recently completed their training and orientation. Although these models were originally designed to help solve nursing shortages by tapping available nurses who might not be able to work in person, there are additional less tangible benefits, such as improved collaboration and a feeling of collegiality.
The same thing holds for technology teams. I know everyone is trying to run as lean as possible, but there’s a cost to doing so. Running an engineering team ragged because it’s not staffed appropriately generally does not lead to strong performance in the long term. It does, however, lead to resentment, lack of focus, lack of buy-in, and often to employee turnover. Cutting corners may lead to short term savings, but ultimately there are long-term consequences that will need to be addressed.
I never thought I’d reach a point in my career where I would be excited to see organizations that were admittedly playing the long game and that were unashamed about putting people over profits. These are certainly the exception in our industry rather than the norm, but I’ll be keeping my eye out for other examples and following them over the coming months.
Do you work at a place that is willing to pay more to ensure higher quality outcomes? Are they focused on balancing work so that everyone can succeed? Leave a comment or email me.

Email Dr. Jayne.





























Traditionally Professional Courtesy is something that physicians gave each other - but we had to be careful with it when…