Top News
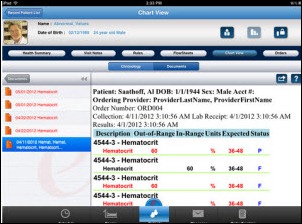
AirStrip Technologies wastes no time in filing a lawsuit claiming that clinical mobility vendor mVisum is violating its remote monitoring patent, awarded September 11, 2012. Travis wrote about the patent on HIStalk Mobile at that time, musing about its potential effect on innovation against the backdrop of Apple’s $1 billion patent victory over Samsung. Travis said:
There isn’t an answer yet as to exactly how this patent will protect AirStrip or how it will affect other mobile health vendors developing solutions to enable remote, mobile viewing of physiologic data by providers. As a methodology patent, can AirStrip use it to protect the experience of viewing a EKG, zooming into specific leads, accessing relevant additional data at the at point in time? … It’s interesting to consider the potential of a company’s defining and protecting the experience of mobile patient data viewing. As we start to see more intuitive user experience design for providers, will a standard emerge and can it be protected, enabling a patent holder to require licensing of the its patents to mirror the user experience?
Reader Comments

From Iguana: “Re: MED3OOO leadership conference. I was pleased to hear McKesson exec Pat Leonard suggest that InteGreat may be the go-forward ambulatory EHR product for hospitals implementing Paragon. Another highlight was former Highmark CEO Kenneth Melani, who provided a terrific synopsis of healthcare reform and where it’s heading.” The MED3OOO folks say several hundred clients participated in last week’s National Healthcare Leadership Conference and Users Meeting in St Thomas, USVI.

From Ms. Kravitz “Re: HIStalk’s Must See Vendors for MGMA 12. How do vendors get on this list?” The“Must See Vendors” lists for MGMA and HIMSS includes those HIStalk, HIStalk Practice, and HIStalk Mobile sponsors who chose to be included (there’s no charge) and provided exhibit information. The MGMA list includes over 50 vendors. Most of them will have a booth on the exhibit floor, while a few others aren’t exhibiting but will have people available for one-on-one meetings.
From F. Jackie: “Re: LogiXML fake 1960s TV commercial. Totally cheesy, but I needed a good laugh and it delivered.” I like it.
From Awkward Debates: “Re: degrees. I’m considering a post-grad education and wonder how the industry, particularly the vendor side, views degrees. MBA? Health informatics? Finance?” Vendor side, I’d go with an MBA unless you’re interested in sales or the executive ranks, in which case degrees (advanced or otherwise) matter little and many folks in the job don’t have them. Health informatics is a good advanced degree or certificate program, but less useful if you don’t already have a clinical degree to pair it up with. My experience is that if you have good qualities (ambition, smarts, relevant experience) and make early connections then a degree doesn’t matter all that much, especially the higher you go up the ladder, and there aren’t many cases where the degree itself is going to get you a job that you couldn’t get otherwise except in technical areas. Personally, I’d say an MBA was my best investment, but the one I admire the most in healthcare specifically is an MPH plus a professional degree (physician, nurse, pharmacist, PT, etc.) We’re going to need public health expertise since you can’t fix healthcare while ignoring health.
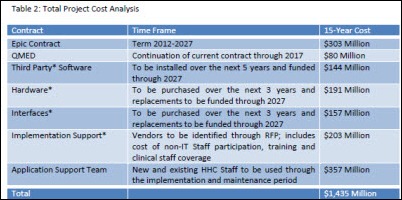
From Academic CIO: “Re: Allscripts protest of NYHHC’s Epic selection. We had a similar experience with Cerner. After losing on all counts, including price (Cerner’s five-year cost of ownership was twice Epic’s), Cerner had the audacity to aggressively pursue a Freedom of Information Act request for all of our e-mails, notes, meeting minutes, and Epic-supplied documents in an obvious attempt to get competitive information on Epic. At the end of day, we didn’t have to give it them, but it cost us a great of taxpayer-supplied resources to comply with their request. This was one of many attempts they made to circumvent the selection process. I would never do business again with them under any circumstances.” As I wrote previously, it’s a high-reward, high-risk strategy for a vendor to try to force itself on a customer who prefers a competitor’s product. Maybe you get a desperately needed new client and keep Wall Street off your back for one quarter, but who’s going to invite you to bid in the future knowing your history of being a sore loser?

From In the Know: “Re: Arcadia Solutions and the Azara Healthcare spinoff. The Pohlad family will sell them to a private equity firm, with the deal expected to close November 1.” Unverified. Arcadia is a consulting firm, while Azara offers analytics. The Minneapolis-based Pohlad Family Companies, which made its founder one of the richest people in America, bought Arcadia in 2007, adding it to holdings that include the Minnesota Twins, real estate, car dealerships, and banks.
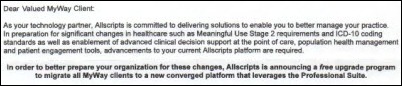
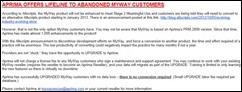
From Oh MyWay – Dust in the Wind: “Re: MyWay. Here’s the Allscripts letter sent to each MyWay client with the grim confirmation. Interesting that the letter wasn’t from Glen, but rather Laurie McGraw. I guess he has bigger issues trying to find a buyer for his company.” It’s a good deal (free) for those MyWay customers who want Pro, but it’s anybody’s guess as to the percentage of MyWay customers in that camp, not to mention that changing systems is always tough. Allscripts says everybody will be upgraded from January to September 2013, which seems ambitious given the tendency of practices to delay until the last minute. I’m curious: if you attended ACE in August, what was said about MyWay then? I assume MyWay clients weren’t forewarned even though Allscripts surely had already planned its strategy. Given that Allscripts says MyWay isn’t ready for Meaningful Use Stage 2 or ICD-10, what were customers led to expect? Still, it’s probably a good decision – Inga asked Glen Tullman an insightful question when she interviewed him on HIStalk Practice in April 2010:
It seems almost as if Allscripts really has two businesses, one that’s focused on the selling the inexpensive MyWay option to small practices through resellers and the other focused on selling to the large, integrated delivery networks and hospitals that subsidize the small practices and offering them the Allscripts EHR products. Explain the strategy and tell me how you avoid channel conflicts.
From Lady Pharmacist: “Re: National Health-System Pharmacy Week next week. It’s time for the annual shout-out to pharmacists and pharmacy technicians, who from an IT perspective are helping their organizations attest for Meaningful Use, closing practicing gaps, and helping with medication-related safety initiatives related to CPOE, medication reconciliation, barcode medication administration, and e-prescribing.” Consider it shouted out.
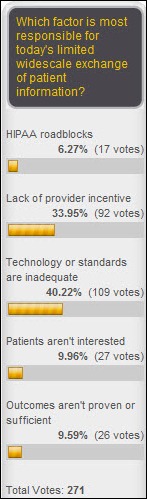
From Patty Melt: “Re: HIEs. This article from Crain’s Detroit reminds me of the Rodney King line – can’t we all just get along? Do you ever wonder what the cost to society is for lack of consensus and cooperation?” The article says that the state’s two biggest HIEs (Great Lakes HIE and Michigan Health Connect) are competing to become the statewide exchange and aren’t sharing patient information with each other. The CEO of Oakwood Healthcare says they’re happy with Epic and not interested in joining an HIE until there’s just one because they could connect with one that won’t survive. Beaumont, also on Epic, said the state needs to get more involved but healthcare reform will force information exchange in any case.
HIStalk Announcements and Requests
 Highlights from HIStalk Practice this week include: Mount Sinai Queens (NY) implements Epic at its ambulatory care locations. MED3OOO and SRS provide updates on their user conferences. Patients who are comfortable accessing and understanding their health information online will use PHRs more willingly. A REC advocacy organization defends the Meaningful Use program. CBS Morning News profiles a pediatrician’s use of social media. Dr. Gregg ponders whether HIT is becoming passé. And as mentioned above, our HIStalk Must See Vendor Guide for MGMA12 is a must-read for anyone heading to MGMA in San Antonio this weekend. Nothing says I love you like a gift of Lucchese cowboy boots (since I am Texas-bound) or your e-mail address for our HIStalk Practice updates. Thanks for reading.
Highlights from HIStalk Practice this week include: Mount Sinai Queens (NY) implements Epic at its ambulatory care locations. MED3OOO and SRS provide updates on their user conferences. Patients who are comfortable accessing and understanding their health information online will use PHRs more willingly. A REC advocacy organization defends the Meaningful Use program. CBS Morning News profiles a pediatrician’s use of social media. Dr. Gregg ponders whether HIT is becoming passé. And as mentioned above, our HIStalk Must See Vendor Guide for MGMA12 is a must-read for anyone heading to MGMA in San Antonio this weekend. Nothing says I love you like a gift of Lucchese cowboy boots (since I am Texas-bound) or your e-mail address for our HIStalk Practice updates. Thanks for reading.
 Speaking of MGMA, I will be posting conference updates starting Sunday night or Monday morning (depending, of course, on the quality of the Sunday evening parties.) Our exhibiting HIStalk sponsors will have signs indicating their support of HIStalk, so please take a moment to tell them thanks on our behalf. If you have any suggestions for sessions or exhibits I should peruse, let me know. Please also take a moment to share any conference comments you might have, as well as your photos. See you in San Antonio! E-mail me.
Speaking of MGMA, I will be posting conference updates starting Sunday night or Monday morning (depending, of course, on the quality of the Sunday evening parties.) Our exhibiting HIStalk sponsors will have signs indicating their support of HIStalk, so please take a moment to tell them thanks on our behalf. If you have any suggestions for sessions or exhibits I should peruse, let me know. Please also take a moment to share any conference comments you might have, as well as your photos. See you in San Antonio! E-mail me.

I was initially startled and then pleased to receive this HIStalk sponsorship announcement at my hospital e-mail address. I finally realized that it went out a broad audience, not just me. Inga got one too, and we agreed that it’s nice when a sponsor is publicly proud of supporting our work (as most seem to be). It made our day.

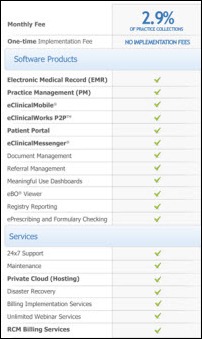
Welcome to Aprima, sponsoring both HIStalk and HIStalk Practice at the Platinum level. The company offers a certified, fully integrated, single application, single database EHR/PM solution along with RCM services. The template-free design is chief complaint-driven with adaptive learning capability. The company, which has a 14-year track record, is offering a timely deal (free license and data migration with a signed support agreement) to users of Allscripts MyWay, for which it provided the original code in 2008. A partial list of the nearly 1,000 enhancements Aprima has made to the product since then is here. MyWay customers and resellers can connect with the Aprima folks at MGMA next week or AAFP this week. Thanks to Aprima for supporting HIStalk and HIStalk Practice.

Welcome to new HIStalk Platinum Sponsor SuccessEHS. The Birmingham, AL-based company offers a Certified Complete EHR and PM that it says can prepare practices for Meaningful Use within 60 days, not to mention that its clients experience an average 11 percent in visit increases and a 19 percent increase in collections in the first six months. The company has been in business for 15 years and is profitable and debt free, with 425 clients and 4,200 providers. Calling support gets you an in-house employee sitting in Birmingham. They’ll be at MGMA next week, also presenting the results of their new practice survey on maximizing revenue. They’re also offering a white paper on healthcare reform (e-Prescribing incentive, Meaningful Use, ICD-10, PQRS). Thanks to SuccessEHS for supporting HIStalk.
I always hit YouTube to see what a new sponsor has out there, so here’s an introductory video from SuccessEHS.
Listening: new from Brooklyn-based Woods, sometimes labeled as folk, but to my ear is more 1970s-influenced trippy, jangly guitar rock with lots of hooks and thoughtful lyrics. I liked it even from the first listen. Best song to me: “Find Them Empty,” featuring wailing psychedelic guitars and keyboard work that could pass for paisley ‘70s bands like Strawberry Alarm Clock or Vanilla Fudge.
On the Jobs Page: Product Manager, Regional Sales Executive.
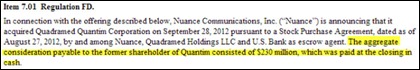
Acquisitions, Funding, Business, and Stock

Athenahealth reports
Q3 numbers: revenue up 26 percent, EPS $0.30 vs. $0.24, falling short on revenue expectations. Shares are down 3 percent in after hours trading.
Microsoft’s Q1 numbers: revenue down 7.9 percent, EPS $0.53 vs. $0.68, missing earnings estimates on continued weakening in PC demand and a corresponding drop in Windows sales.
Shares in Google dropped precipitously Thursday when the company’s financial printer filed its 8K report in the middle of the trading day instead of after hours as intended. Trading in GOOG was temporarily halted, but shares still ended up down 8 percent at the market’s close because of slowing revenue growth.
Trinity Health and Catholic Health East announce plans to merge, forming a new system with annual operating revenues of about $13.3 billion and 87,000 employees. Trinity’s president and CEO Joseph R. Swedish would head the new organization and Catholic Health East’s president CEO Judith M. Persichilli would be EVP. The organizations anticipate reaching a definitive consolidation agreement in the spring of 2013.
Sales
Australia’s UnitingCare Health will implement Cerner at the recently-opened St. Stephen’s Hospital, which claims it will be the country’s first digital hospital.
The 60-provider Mid Dakota Clinic (ND) selects athenahealth’s EHR, practice management, and care coordination solutions.

Wenatchee Valley Medical Center (WA) chooses Merge’s iConnect Enterprise Archive.
The University of California, Irvine Medical Center, will deploy MModal Fluency Direct and MModal Catalyst integrated with Allscripts Sunrise Clinical Manager.
People

RCM and consulting services provider Cymetrix names Jeffrey Nieman (Accelion) SVP of remote operations.

Alan Fowles, managing director of Cerner Europe and overseer of the first Cerner NHS installations, resigns after 11 years with the company.

RCM provider Office Ally names Daniel Wojta (United Healthcare) director of eSolutions and business development.

Health First (FL) appoints Lori DeLone (PatientKeeper) SVP/CIO.

Mobile PHR provider Cognovant hires Andrew Lambert (Press Ganey) as EVP of business development.

Lynn Danko (Lawson Software) joins Amcom Software as CFO.
Ambulatory surgical center and rehabilitation clinic software vendor SourceMedical announces the resignation of CEO Larry McTavish and the promotion of Ralph Riccardi from EVP/COO to president and CEO. The company announced last month that PE firm ABRY Partners had made a significant investment.
Standard Register promotes John King from VP of sales to president of Standard Register Healthcare. He replaces Brad Cates, who is leaving the company to serve as CEO at another company.
Announcements and Implementations
Omnicell and Cerner will develop interoperability between their products using CareAware iBus, Cerner’s medical device connectivity solution .
HIMSS names the 91-provider Coastal Medical (RI) the winner of its 2012 Ambulatory HIMSS Davies Award of Excellence.
Kennewick General Hospital (WA) launches McKesson Paragon CPOE.

Baptist Memorial Health Care (TN) deploys EMC VNX and Citrix virtualization technologies in advance of its Epic implementation.
University of Kentucky Healthcare implements Harris Corporation’s Business Intelligence Documentation and Coding dashboard.
MedAptus announces the availability of its ICD-10 software suite.
Government and Politics
National Coordinator Farzad Mostashari, MD says the HIT Policy committee will review whether EHRs are leading doctors to overbill Medicare. He says repeated copying and pasting of patient information is “not good medicine” and wants to determine if EHR functions that prompt doctors to inflate their bills should be made “off limits.”
An Institute of Medicine report finds that the DoD and VA’s failure to create a sequential prescription number system has hindered joint EHR development at the co-managed Captain James A. Lovell Federal Health Center (IL). Because the DoD and VA have both agreed not to charge their respective EHRs, the departments are spending $700,000 a year for pharmacists to manually input prescription data. The IOM recommends that the DoD and VA avoid establishing other combined facilities until an integrated EHR is available.
The VA launches a contest to encourage the development of an appointment scheduling system to work with VistA EHR open source applications.
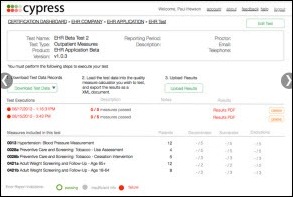
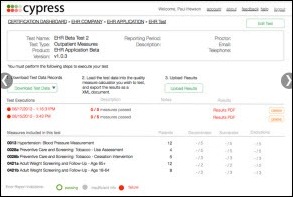
ONC announces availability of Cypress, an open source certification tool for testing the availability of complete or modular EHR systems to meet Stage 2 MU requirements for clinical quality measures.
As of September, almost 50 percent of all EPs and nearly 81 percent of hospitals have registered for the MU program. CMS also reports total program-to-date payments of $7.7 billion, including $4.8 billion to hospitals and $2.6 billion to eligible providers and healthcare professionals.
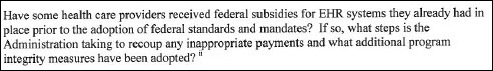
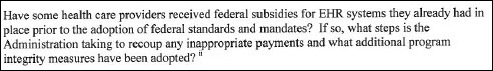
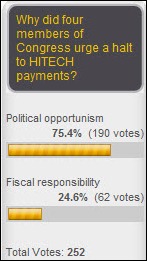
Two weeks after House Republicans call for a freeze on all MU payments, four Republican senators request a meeting with HHS Secretary Sebelius to discuss the incentive program. The senators would like CMS and ONC to address four questions, including whether EHRs are increasing the volume of diagnostic tests and Medicare billings. One of those questions (above) indicates a lack of familiarity with the HITECH program, which did not require providers to buy anything at all to qualify for taxpayer-funded incentives.
Technology
eMDs launches its nMotion EHR iPad application.
Medsphere Systems contributes its MSC FileMan database management system to the OSEHRA open source community, which chose it for collaborative development work on VistA.
An article in MIT’s Technology Review says that medical devices in hospitals are regularly infected with viruses because vendors are so scared of the FDA’s requirements that they won’t allow hospitals to keep their operating system patches and antivirus software current. I’ve seen this personally: my former hospital had a nasty worm that was flinging itself with impunity from one networked system to another because our vendors wouldn’t allow us to apply any changes to their FDA-approved configuration (even including applying the latest antivirus update that was known to fix the problem). We had to take the entire imaging network and several systems offline to the extreme displeasure of our physicians, while the vendor said they might get us an answer in a few weeks. I told the network team to ignore everything they had heard and simply do what they knew needed to be done. We were worm-free within a few hours and I have no doubt patients would have suffered had we not ignored our vendor’s advice, albeit at our own risk.
Other
Former Beth Israel Deaconess Medical Center CEO Paul Levy, writing in his Not Running a Hospital blog, equates buying Epic to the Stockholm syndrome, where hostages develop affection for their captors. He concludes that Epic’s market share, driven by HITECH money, makes the company a target for Congressional retribution if a system malfunction harms patients. He also complains, “How did this firm get such a big share of such a critical market with no government review?”
The local paper covers Michigan-based HipaaCat, an image sharing and messaging app developed by a plastic surgeon.

Dan and Colin from Divurgent said Olympic bling-bearers Kerri Walsh Jennings and Misty May-Treanor were “great fun and great sports” in posing with attendees like themselves at CHIME 2012 this week. They (Kerri and Misty, that is) look a lot different with sunglasses off and clothes on.
In England, a healthcare trust that’s in such serious financial straits that it may be dissolved takes heat from the local paper for sending five managers to the Cerner Health Conference. The paper couldn’t find a source to back up its predetermined editorial outrage, so it quoted some guy who whose partner “does not wish to be named who worked as a nurse at Princess Royal Hospital.” It also seems to find a sinister connotation to KC’s power and light district, which it repeatedly places inside quotation marks as though it’s a code word for a hooker-staffed crack house. Must have been a slow news day.
Weird News Andy thinks maybe someone misspelled “birth” as “berth” in this story: a woman delivers her one-month premature baby in a Philadelphia subway car in which she is the only occupant. She calmly walks off the car and finds a police officer, who says the newborn girl “took on her personality” in exhibiting the same calm demeanor as her mother as they were taken to the hospital.
Tweets from CHIME
Sponsor Updates

- PatientKeeper employees donate services, goods, and cash to help a Boston-area homeless family move into a furnished apartment.
- GetWellNetwork launches its Transformative Health blog with an introductory post by CEO Michael O’Neill, Jr.
- Intelligent InSites shares best practices for deploying an enterprise-wide RTLS during an October 25 Webinar.
- Infor opens its new headquarters in NYC and unveils updated branding. Also, the Institute for Transfusion Medicine (PA) upgrades its Infor Healthcare Revenue Management solution to integrate with its outpatient records and receivables solution.
- Oregon Medical Association will offer Dr. First’s RcopiaMU e-prescribing services to its members.
- Emdeon releases a white paper on payment collection best practices for small physician offices.
- Teradata will integrate QlikView in-memory data with Teradata’s Integrated Data Warehouse via the QlikView Direct Discovery utility.
- Physicians in Costa Rica’s public health system use DynaMed’s clinical reference tools to create national breast cancer guidelines.
- Quality IT Partners sponsored last month’s 2012 Hillman Cancer Center Gala in Pittsburgh.
- Imprivata announces 10 additional sponsors of its Imprivata HealthCon 2012 User Conference next month in Boston.
- Cancer Treatment Centers of America and CareTech Solutions present a case study on the need for clinical help desks at this week’s CHIME CIO Forum.
- American Well CEO Roy Schoenberg and Allscripts CMO Douglas A. Gentile discuss the benefits of integrating American Well’s telehealth offer with EHRs offered by Allscripts.
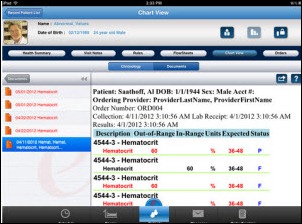
McKesson integrates RelayHealth’s procedure and test results functionality into its Practice Choice EMR and financial management software.
- T-System announces six winners of its T-System Client Excellence Awards.
EPtalk by Dr. Jayne
Researchers at Duke University create a 3D training application for transesophageal echocardiography for anesthesiology residents. It runs only on the iPad, leading one researcher to state that it would have greater effect if it worked on multiple platforms.
Speaking at the American Academy of Family Physicians annual meeting in Philadelphia, Farzad Mostashari encourages physicians to “turn the tables” on vendors that aren’t addressing interoperability issues. He reportedly advised users to report vendors to certification bodies. Considering the rank-and-file primary care physicians I work with every day, I’m not sure many of them are savvy enough to understand the certification requirements, let alone to become whistle-blowers. I’d rather see physicians spending their time learning to use their EHRs efficiently to deliver quality care. I invite my family physician readers who may have heard the speech in its entirety to weigh in – don’t worry, I’ll keep you anonymous.
The Breast Tissue Screening Bra from First Warning Systems has been designed to detect minute temperature changes in breast tissue that may indicate cancer via sensing the growth of new blood vessels. Temperature data is uploaded to the Internet and algorithms provide a reading to the patient. FDA approval is pending, but release in Europe is anticipated next year.
An impending change in the ranks of Medicare administrative contractors prompts concerns from providers that payments could be delayed. CMS is in the process of re-bidding contracts for claims processing, program enrollment, and other administrative functions in several regions. During a 2008 change, some payments were delayed for six to 12 months. Given the rigor with which CMS audits providers and the narrow tolerances in which we must perform to get paid, it would sure be nice if they held their contractors to the same standards. If we don’t file promptly, we don’t get paid – maybe if they don’t pay promptly, they should be fined.

I have to admit that I’ve been jealous reading about Inga’s plans to attend the MGMA meeting in San Antonio next week. I’m trying to find a way to sneak away for a day so the two of us can make a pilgrimage to the source of some of the hottest boots known to (wo)man. I had a chance to buy these beauties last year and flinched. Cross your fingers!
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
More news: HIStalk Practice, HIStalk Mobile.





















































































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…