News 5/1/13
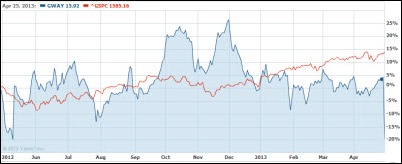
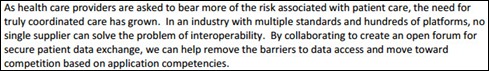
Greenway Medical announces that it will swing to a loss for the current fiscal year because of declining sales and deferred revenue. The company’s fiscal year earnings estimate of $0.10 to $0.17 on $145-$150 million in revenue was revised to a loss of $0.11 to $0.13 on revenue of $132-$134 million. The fiscal year ends June 30. Shares dropped from Friday’s $16.05 close to just above $12 by Tuesday morning, but had rebounded to $13.47 by Tuesday’s close. Above is the one-year GWAY share price (blue) vs. the S&P 500 (red).
Reader Comments
From Big Tex: “Re: Epic deals. St. David’s Healthcare in Austin and Methodist in Houston are both heading to Epic, though I don’t think either has officially announced yet.” Unverified.
From John: “Re: interesting comment from an FBR analyst covering Nuance’s poor earnings announcement. ‘While several industry/external (smart phone consolidation, transcription transition, EMEA weakness) factors have put pressure on mobile and healthcare growth, we believe the blame lies squarely around Nuance’s execution in the field, coupled with management’s feverish acquisition strategy over the last year, which has put onerous integration risks back into the Nuance story. While we believe potential activism could put a floor on Nuance shares and ultimately enhance shareholder value over time (e.g., management changes, split-up of the company, M&A path), we find it hard to remain positive on the Nuance story as the company goes through a challenging transition process in its business over the next six to nine months.’” Carl Icahn just announced that he’s loaded up on more shares, so the surprisingly poor results for both revenue and earnings help make his eventual argument that the company should be broken up or sold outright.
From Mr. Eko: “Re: HIMSS Middle East. Started Monday. Some American-based companies there are Cerner, GE, and Medicity. Judy Faulkner, CEO of Epic, was spotted yesterday morning eating breakfast in the Four Seasons hotel. Rumor has it they are pitching to the Ministry of Health for Saudi Arabia.”
From Giles: “Re: healthcare IT decision making. Interesting reader comments. What’s your opinion?” I agree with some of the comments that healthcare organizations are quicker to promote and retain executives who wouldn’t qualify for comparable jobs in most other industries based on their education and experience. However, healthcare is a different world, trying to balance the demands of an increasingly interventionist government, regulators, special interests, politicians, clinicians, community leaders, and giant insurance companies with the patients and families who are hardly typical customers. I’ve seen cases where hotshot IT people from allegedly more progressive sectors were brought in with near disastrous results, even though the IT shop looked like a showcase on paper. Some healthcare CIOs are not very good at strategic planning, management, and customer engagement, but they have a small domain with minimal clout and high operating and capital expenses due to decisions almost always made by someone else with more influence. Healthcare CIOs also aren’t given a lot of unilateral decision-making over anything other than infrastructure – everybody likes to suggest and approve massive change management projects that get incorrectly tagged as IT initiatives, but those folks disappear when their own lack of leadership ability starts sending the project down the drain due to poor user acceptance, lack of resources, and poor project decisions. My opinion, therefore, is that healthcare IT leaders aren’t empowered to make a lot of decisions on their own, are struggling to deal with the mess foisted upon them by their fellow executives and third parties, and are trying to deal with the squeeze of ever-increasing demand with an ever-decreasing budget. I’m fairly certain that swapping them out with fat-resume private sector CIOs wouldn’t make much difference on the plus side of the ledger, but would cause all kinds of unintended consequences to patient care. It’s easy to shoot the messenger, and with regard to many high-profile projects, that’s all the CIO is allowed to be. If nothing else, consider the high degree of CIO turnover – if all it took was new people in the chair, you’d be seeing wide swings in success from that alone and that’s not the case.
HIStalk Announcements and Requests
The global reach of @histalk here at #himssME at the Faisalea Tower in Riyadh #HealthIT twitter.com/drnic1/status/…
— Nick van Terheyden (@drnic1) April 30, 2013
Nick van Terheyden, MBBS, CMIO of Nuance, posted the cool photo above on Twitter. If you’re traveling anywhere interesting, send a fun local photo with something that identifies HIStalk and I’ll run it here.
Welcome to new HIStalk Gold Sponsor Porter Research, A Billian Company. The company provides its clients with customized market intelligence and research insight that includes go-to-market strategy, focus groups, win-loss analysis, prospect profiling and lead generation, competitive analysis, customer and market analysis, and M&A research. Don Graham (GM of both Porter Research and Billian’s HealthDATA) and Cynthia Porter (president) have many years of industry experience with major healthcare IT firms. The company offers a brochure, case studies, a newsletter, and white papers that illustrate its expertise. Thanks to Porter Research for supporting HIStalk.
Acquisitions, Funding, Business, and Stock

Emdeon completes re-pricing of its existing senior secured credit facilities, securing lower interest rates on its term and revolving loans.
Nuance reports Q2 results: revenue up 15.9 percent, EPS $0.34 vs. $0.43, missing estimates on both and sending shares down 18 percent and increasing speculation that activist investor Carl Icahn will use his recently acquired 10.7 percent of the company’s shares to force a breakup.
USARAD.com launches SecondOpinions.com, which offers same-day medical second opinions. Radiology-related reports range from $29 for an X-ray to $99 for an MRI. The company also offers second opinions for primary care, surgery, dermatology, and other services.
Forms automation vendor FormFast opens a UK-based subsidiary.
Sales
Trinity Health (MI) signs a multi-year agreement with Explorys for data analytics solutions.
Saint Mary’s Regional Medical Center (NV), Renown Health (NV), and Chandler Regional Medical Center (AZ) select MRO Corp.’s ROI Online platform to manage release of information.
West Florida ACO will deploy Sandlot Connect, Dimensions, and Metrix from Sandlot Solutions for patient health information management.
Methodist Health System (NE) selects Wolters Kluwer ProVation Medical software for its gastroenterology procedure documentation and coding.
Amerinet contracts with Cornerstone Advisors Group to provide HIT advisory and implementation services to its group purchasing members.
Tri-State Orthopaedics (IN) selects SRS EHR for its 24 providers.
Saudi Arabia’s King Fahd University Hospital will implement Nuance Healthcare Dragon Medical 360 | Network Edition hospital-wide.
The Cleveland Clinic’s MyPractice Healthcare Solutions will provide project management and implementation assistance to Glens Falls Hospital (NY) as it deploys Epic at its physician and specialty practices.
People
MedMatica Consulting Associates appoints Jerry Howell (KPMG) CEO and a member of the company’s board of directors.
Thomas H. Lee, MD (Partners HealthCare) joins Press Ganey as chief medical officer.
CSI Healthcare IT hires Martin O’Neil (Charts In Time) as health information management practice director.
Meditab Software appoints Adele Nasr (WebMetro) VP of marketing.
A. John Blair III, MD, CEO of EMR consulting firm MedAllies, is elected chair of independent Direct community DirectTrust.org.
Christopher Mansueti, former VP of client services for RelWare, died Friday, April 26 of amyotrophic lateral sclerosis. He was 53.
Announcements and Implementations
VHA, Inc. adds physician dashboards to enhance its VHA IMPERATIV Advantage performance improvement solution, which leverages transactional-level data through Truven Health Analytics and UHC.
MDI Achieve, provider of the MatrixCare EHR for long-term acute care, will integrate with Homecare Homebase, a provider of homecare and hospice technology solutions.
Heywood Hospital (MA) streamlines clinician workflow following its implementation of Accent On Integration’s Accelero Connect integration platform.
Samaritan Albany General Hospital (OR) moves from Meditech to Epic this week.
Transylvania Regional Hospital (NC) goes live on Cerner.
Children’s Hospitals and Clinics of Minnesota implements wireless data transmission between Cerner’s EMR and CareFusion’s infusion pumps.
PeriGen recognizes its client Banner Health (AZ) for reducing unnecessary early-term deliveries by 22 percent, earning the health system a Showcase in Excellence Award from the Arizona Quality Alliance.
Florida Hospital Tampa implements the EarlySense bedside patient monitoring system.
A Modern Healthcare article covers the State of West Virginia’s VistA implementation. It’s paying Medsphere $8.4 million per year for support and an unspecified amount to InterSystems for Cache’ licenses. The state also added financial systems from NTT DATA to replace VistA’s minimal capabilities. Update: Modern Healthcare issued a correction to this article – Medsphere has been paid $8.4 million over the life of the contract (since 2005), around $940,000 per year.
The Pittsburgh paper profiles Omnyx, a five-year-old digital pathology systems vendor formed as a joint venture between UPMC and GE Healthcare.
Government and Politics
Arizona lawmakers pass legislation that will require health insurers to pay for telemedicine treatment for certain specific conditions for patients living in 13 rural counties.
Rep. Ted Poe (R-TX) introduces a bill that would prohibit HHS from mandating providers to switch to ICD-10 code sets, which Poe contends would cost about $80,000 for individual doctors and $250,000 for practices with five to 10 physicians.
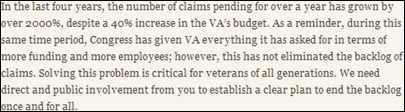
A bipartisan group of 67 senators sends President Obama a letter calling for him to be more directly involved in the VA’s disability claims backlog situation. The senators note that the average wait time for first-time disability claims is around 316 days, with a delay of up to 681 days in certain parts of the country. Of 900,000 pending claims, more than 600,000 are over 125 days old.
Innovation and Research
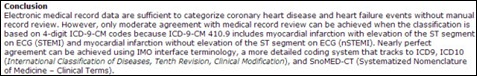
A peer-reviewed article published by the CDC finds that the interface technology of Intelligent Medical Objects is superior to population classification techniques as a disease surveillance tool. The findings are based on a study that showed IMO terminology service was 32 to 42 percent more accurate in identifying coronary heart disease compared to algorithms using reimbursement coding and classification techniques in identifying coronary heart disease.
Technology
AirStrip Technologies settles its patent dispute with MVisum, Inc., a competitor it accused of infringing on its patent for real-time viewing of patient data on mobile devices. MVisum agreed not to offer infringing products that include “streaming or displaying real time or near real-time patient physiological data.”
NextGen Healthcare launches Comparison Utility, a proprietary ICD-9/ICD-10 comparison tool that is available a no charge to its customers.
Healthcare Holdings Group acquires the exclusive rights to 3D-Practice’s patient education graphics technology, which it will embed in its ChartZoneMD EHR.
Other
Athenahealth and MIT’s H@cking Medicine host a May 4-5 Hack-a-Thon aimed at at bringing about disruptive and meaningful solutions to healthcare challenges.
Anthony Weiner, the former Congressman who resigned after admitting to sending sexually suggestive text messages and photos to several women, is making big money as a corporate consultant. One of his clients is EMR vendor CureMD.
Here’s Imprivata’s latest HIT cartoon.
Sponsor Updates
- DrFirst publishes a white paper highlighting the 428 percent growth in e-prescribing for controlled substances.
- Medseek holds the inaugural meeting of its Clinical Advisory Council , formed to enhance patient engagement.
- MedAptus highlights three customers and their seamless integrations between the MedAptus charge capture solution and their EHRs.
- GetWellNetwork recognizes 12 hospitals and individuals for improving clinical care and outcomes through the use of IPC technology.
- Inland Northwest Health Services releases its 2012 Community Report.
- Martin’s Point Health Care (ME) discusses how its use of PopulationManager by ForwardHealth Group has improved its ability to respond to patient needs, identify gaps in care, and make systemic changes based on performance.
- Imprivata hosts May 9 Webinar introducing the benefits of OneSign for healthcare.
- Nuesoft hosts a May 8 Webinar on using technology to improve revenue cycle.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.

































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…