Top News

Cerner reports Q3 numbers: revenue up 8 percent, adjusted EPS $0.35 vs. $0.30, falling short on revenue expectations. From the conference call:
- Domestic revenue was up 8 percent, while global revenue increased only 1 percent.
- The company sold its sixth French client and its first one in Brazil.
- Cerner says that by the end of the decade, the EMR will provide just one feed into a population health management system, and the company is already selling solutions and services to customers who don’t use a Cerner EMR.
- Cerner and Epic are distancing themselves further from their competitors, and Cerner says it is gaining momentum against Epic.
- Cerner says its clients have acquired hospitals at six times the rate of Epic’s, giving the company more potential users.
- Cerner has been approved by Apple as the only non-carrier company allowed to sell the iPhone, and it will offer an unlocked, no-plan iPhone for CareAware Connect, which can replace pagers and other communications devices.
- Cerner says its work with Intermountain Healthcare will disrupt the industry and accelerate clinical computing by a decade, reducing healthcare costs by up to 20 percent. Projects include using Intermountain’s Care Process Models as an EMR-agnostic “clinical navigation system” and blending content with the EMR to provide activity-based costing as a resource management system.
- EVP Jeff Townsend compared Epic to Kodak for its suggestion that Meaningful Use be delayed for five years, suggesting that both Epic and Kodak spent too much time selling profitable old technology and trying to delay the inevitably changing future.
- An analyst noted that “Intermountain has a history of chewing up and spitting out vendors” and asked how Cerner can keep them happy. Townsend said Cerner will do an accelerated Millennium implementation so they can get to the “fun stuff” more quickly.
- Cerner says it was chosen over Epic at Intermountain because of population health and the ability to influence cost, saying, “This is not a project. This is a decade, if not a two-decade-type relationship.”
Reader Comments
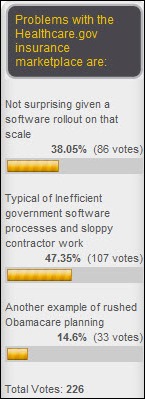
From Digital Bean Counter: “Re: million dollar question. Why hasn’t the government asked any of us health informaticists about fixing the Healthcare.gov website?” It’s not an informatics problem, so that would be pointless. Nobody in healthcare (nor in government contracting, apparently) has the experience needed to plan for the kind of scale Healthcare.gov needs and there’s nothing there at all related to informatics. It requires people who have built monster-sized e-commerce sites, the kind who live in the Silicon Valley instead of the beltway. It’s a shame that the site has turned into a political football – nobody seemed to mind when the VA, DoD, and HHS were burning through millions to billions of dollars in poorly planned and poorly managed IT projects and the website is only marginally related to Obamacare. Nobody can say anything about any topic these days without someone screaming about a perceived political agenda, and politics isn’t the same as the government, which is comfortingly inefficient and wasteful no matter which party is involved. I think I remember a stat that 50 percent of US government software projects are utter failures and a complete waste of taxpayer money and almost all of the rest don’t deliver the expected value.
From Alexis Nexis: “Re: expense reports gone wild. There’s no understanding of what someone on the road experiences: a hotel room and bed, no ability to cook some eggs in the morning, no ability to pack a sandwich for lunch, doing laundry just on the weekend, etc. Not to mention the additional six to 25 non-billable hours of travel (above the commute between hotel and office) typically incurred every week by road warriors. I can assure you that there’s no road warrior getting rich off his meal expenses. I am quite surprised that snacks and coffee are being included. IRS guidelines view meal expenses as breakfast, lunch, and dinner. Shame on the commentator for not having negotiated a contract accordingly. And shame upon those contract administrators who insist upon receipts for when IRS guidelines don’t require them. To have to save my receipt for the toll on the highway or for my $7 of breakfast in the morning is ludicrous. It burdens everyone with additional unnecessary overhead. I routinely put into my contracts the IRS per diem rate for the locale. Perhaps we should wonder about what it is that makes healthcare in the United States the most expensive in the world without our getting the best return what we spend. I would suggest that it’s not the relatively incidental amounts being referred to. By the way, where could I sign up for that $200 an hour rate?” This is one of those “don’t sweat the small stuff” issues. Line item living expenses are annoying because you get into that pointless mental debate over whether a consultant who buys a $4 coffee on the way to the hospital every morning must be screwing you in other ways as well, and yet sometimes that same employer doesn’t give the consultant a clear picture of what work needs to be done or doesn’t have the required internal people lined up. At $200 per hour, that $4 coffee represents just over one minute of billable time, and I’ve seen consultants trying to find things to do for hours each day because they were just shown a cubicle and abandoned because nobody had the time to manage them.
From Bignurse: “Re: Yann Beaullan-Thong of Vindicet. You interviewed him a few weeks ago. The 2013 McKnight Technology Award in the Transitions category was awarded to a Vindicet client for implementing its patient management system. The organization says the system cut admission time to its skilled nursing settings to less than 1 hour.” Yann’s HIStalk interview from December 2012 is here. The company offers referral management and discharge managing systems.
From Boy Oneder: “Re: Epic’s Healthy Planet. It’s population health management and is robust – wellness, chronic disease registries, population outreach, high risk care management, and risk stratification algorithms.” I heard the term “Healthy Planet” and asked Boy Oneder what it was all about. Boy Oneder also says that Epic had documented clinical workflows in the Netherlands years ago in preparation for sales like the two that just happened to two large Amsterdam hospitals. I don’t think Epic is joking when it talks about world domination.
From Player: “Re: Epic hospital. You should interview a CFO, anonymously or otherwise, about how they looked at the cost justification for implementing Epic.” That would be fun. Volunteers?
From Boy Lee: “Re: innovative companies. You profiled some of them years ago.” I ran a series I called Innovator’s Showcase in 2011, which took a ton of work. I invited startups to apply to be profiled on HIStalk, but they had to have an original product, real customers, real revenue (although not too much of it), an a short time in business. I had three folks review their brief applications and we chose seven for the Innovator’s Showcase. We thought these had the best chance of success. None have failed as far as I can tell. They were:
Aventura (clinician computing experience)
Health Care DataWorks (analytics)
OptimizeHIT (which was connected to ImplementHIT in some way that confuses me to this day, which offers EHR training)
Caristix (HL7 and interfacing software)
Logical Progression (acquired by Bottomline Technologies – offered mobile documentation)
Trans World Health Services (benchmarking and analytics)
Health Nuts Media (learning games and educational material)
From DrLyle: “Re: your comments about physician-focused startups with no clue how to make solutions for doctors. I loved your answer. I just wanted to make sure the key word is ‘most’ and not ‘all.’ Some of us are actually making some good stuff that truly uses HIT to automate and delegate care, saving time for docs and improving quality for patients.” I was amused at the number of folks whose brains blocked all but the words they get emotional about, firing them up to argue about what they perceived as an anti-innovation rant. I very specifically mentioned only companies that don’t care about patients or providers and that are clueless, arrogant, insulting, and badly planned. If I were CEO of one of those I’d keep quiet, and if I was one of the better startups, I’d be happy that my unworthy competitors had been called out publicly. I’ve been the hospital IT guy who heard these pitches and I’m fairly certain most of my peers think similarly – don’t come knocking until you’ve done your homework. Hospitals may seem like local businesses that need help, but they are massive enterprises. Getting your fledgling product in the door means someone internal is going to have to go to bat for you, meaning their job is on the line if you can’t deliver. Do you have documentation, an implementation plan, around-the-clock support, and sound technology that isn’t dependent on your one Romanian programmer not finding a better contract?
I should mention that part of my rant came about is because I resent any company (big or small) that barges into healthcare without showing respect for patients and the people who have been involved in taking care of those patients all along. Healthcare is a vendor’s Vietnam, as Misys or Sage or any number of other half-hearted former dabblers can explain. They saw themselves swooping in from other industries with massive firepower and a hearts-and-mind campaign that would ensure a quick and painless surrender by the peaceful, primitive locals. A handful of years later, their thoroughly defeated and demoralized salespeople and executives were climbing over each other’s backs desperate to squeeze onto that last available helicopter ride to safety.
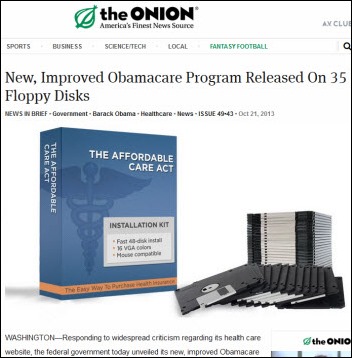
From Lazlo Hollyfeld: “Re: Healthcare.gov. At least the CD version is slated for a ‘16 release.” The Onion is brilliant as usual in its satire about Healthcare.gov.
HIStalk Announcements and Requests
 Some goodies you may have missed this week on HIStalk Practice include: Practice Fusion defends its practice of emailing patients to request physician reviews. Parents want to email their pediatricians and they want it to be free. The Rothman Institute will implement White Plume ePASS. Female doctors provide better quality care than their male counterparts. A physician is charged with breaking and entering after she broke into an office, set up a temporary practice, and began seeing patients. Hayes Management Consulting VP Rob Drewniak outlines a process to prevent breaches with HIPAA compliance. Dr. Gregg offers a Top 10 and a Bottom 10 List on HIT adoption. Linda Fischer, EMR manager for Boulder Community Hospital Physician Clinics, discusses her Greenway Medical EMR implementation, including details on the selection process, EHR data migration, obtaining physician buy-in, and quality care initiatives. In lieu of sending Halloween candy, please treat me to your email address to subscribe to the latest HIStalk Practice updates. Thanks for reading.
Some goodies you may have missed this week on HIStalk Practice include: Practice Fusion defends its practice of emailing patients to request physician reviews. Parents want to email their pediatricians and they want it to be free. The Rothman Institute will implement White Plume ePASS. Female doctors provide better quality care than their male counterparts. A physician is charged with breaking and entering after she broke into an office, set up a temporary practice, and began seeing patients. Hayes Management Consulting VP Rob Drewniak outlines a process to prevent breaches with HIPAA compliance. Dr. Gregg offers a Top 10 and a Bottom 10 List on HIT adoption. Linda Fischer, EMR manager for Boulder Community Hospital Physician Clinics, discusses her Greenway Medical EMR implementation, including details on the selection process, EHR data migration, obtaining physician buy-in, and quality care initiatives. In lieu of sending Halloween candy, please treat me to your email address to subscribe to the latest HIStalk Practice updates. Thanks for reading.
Here are a couple of on-the-spot interviews Bonny and Catherine of Aventura conducted at ACEP13 in Seattle last week. They just turned on the video recorder and let the folks say whatever they wanted about IT.
From an ED physician:
Technology is struggling to match what physicians and other clinicians actually want to have happen. When people say all the time, “Is this a great system?” then yes, it’s a great system, but not in this particular setting. There’s many, many, many times a mismatch between what the clinicians want to have done and what the technology can do. There’s innocence on both sides. That’s what my experience has been with this technology. This innocence of mismatch, where the technical people are extremely good at what they do, the hospital people and clinicians are very good at what they do, but this matching of the two is really not working nearly as well as everybody thinks it is. As an example of why there’s this disconnect between documentation and clinicians is my assessment of a patient begins way before anybody thinks it does. It begins when I hear that patient screaming out of the corner of my eye as he’s brought in. I’m not documenting then. I’m not even seeing the patient yet, but that’s when my assessment begins. When I walk into the room, the smells and everything, that’s all part of my assessment, but many times that does not get documented.
From a resident:
I’m a fourth-year EM resident. Our workflow is that we will typically sign up for patients at the doctor’s station and go and see the patient, which takes about five to 10 minutes. Then come back, put our orders in, see other patients, and then we’ll frequently come back and either document or dictate in between patients. Aventura seems like a good application. Friendly, very fast. Sounds like it would be helpful.
Acquisitions, Funding, Business, and Stock

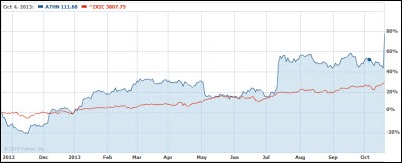
Microsoft turns in Q1 numbers: revenue up 16 percent, EPS $0.62 vs. $0.53, beating expectations.

McKesson files Q2 numbers: revenue up 10.7 percent, adjusted EPS $2.08 vs. $1.79, beating expectations on both. Technology Solutions revenue was up 7.7 percent although software revenue was down 9 percent. The company also announced that it will acquire a majority stake in Germany-based drug wholesaler Celesio for $8.3 billion “to form a global leader in healthcare services.” John Hammergren, asked about whether the company will keep the technology business, waffled by saying results are good and there are no plans to change the mix, but MCK isn’t married to any particular strategy and has a responsibility to revisit that decision constantly.

Covisint reports its first quarterly results after its recent IPO: revenue up 19 percent, adjusted EPS –$0.08 vs. –$0.15.

Hospital health information management provider IOD Incorporated acquires ApeniMED, a Minneapolis-based company offering healthcare interoperability solutions.
Accelera Innovations secures a $200 million equity investment agreement from Lambert Private Equity. I’ve never mentioned Accelera even once on HIStalk and I admit I’ve never heard of them. Their website looks like something kid with FrontPage might have created in 2002, playing annoying music (unless you’re an “Arrested Development” fan, in which case you’ll enjoy Europe’s “The Final Countdown” because it will remind you of a G.O.B. magic trick ) following someone loudly and pedantically reciting a company pitch. Frankly, I’m struggling to believe the accuracy of the story that someone invested $200 million in this operation.

Quality Systems reports Q2 results: revenue down four percent to $118 million, EPS $0.22 vs. $0.31, missing analyst estimates on both. CEO and President Steven T. Plochocki says the results are indicative that the reorganization plan put in place during fiscal 2013 is beginning to gain traction. He also notes that revenue, bookings, and system sales were up from the first quarter.

The Wellness Network acquires hospital patient education software company Logicare.

Cureatr, which offers secure messaging solutions for providers, secures $5.7 million in Series A financing.
Miami Children’s Hospital signs a deal to allow HealthFusion to offer South Florida pediatricians an MCH-specific version of the company’s iPad-based MediTouch EHR that will connect to the hospital’s systems.
Sales

Trinitas Regional Medical Center (NJ) selects EDCO Health Information Solutions to implement Solarity technology and indexing services for medical records scanned at patient discharge.
Elmwood at the Springs Healthcare Center (OH) selects VersaSuite for EHR/PM for its long term acute care facilities.
Rush Health (IL) endorses athenahealth’s EHR and PM services for its 300 affiliated private physician members.
The State of California Office of Health Information Integrity selects iBlueButton from Humetrix for its HIE pilot.
The Berlin Visiting Nurse Association (CT) will replace McKesson Homecare with Brightree’s home health platform.
Children’s Hospital of Philadelphia signs a five-year contract with OnPoint Medical Diagnostics for its MRI Quality Assurance software.
VA Midwest Health Care Network chooses Visage 7 Enterprise Imaging Platform enterprise viewer for regional diagnostic interpretation and image access throughout its 11 hospitals. The organization also chooses Medicalis for enterprise workflow and Acuo for its vendor-neutral archive.
People

Athenahealth names Amy Abernethy, MD, PhD (Duke University Medical Center) to its board.
Vermont IT Leaders elects Paul Harrington (Vermont Medical Society) chair of its board.
Announcements and Implementations
Care at Home (CA) deploys AtHoc’s Home Care Alerts emergency mobile solutions.
Spectrum Health (MI) automates the exchange of patient information via CCD between its HealthMEDX post-acute care EMR and its Cerner and Epic platforms.
HIMSS names Texas Health Resources a winner of the 2013 Enterprise HIMSS Davies Award of Excellence for its use of HIT. CIO Ed Marx is a regular contributor to HIStalk.

Boston Children’s Hospital launches Wired Informatics to provide enterprise-grade NLP solutions for hospitals and other healthcare entities and introduces its flagship product Invenio, which extracts and leverages knowledge contained in clinical notes.

Partners Healthcare’s Center for Connected Health launches Wellocracy, a clinically-based source of self-help technologies for consumers, including health and fitness trackers and mobile apps.
Government and Politics
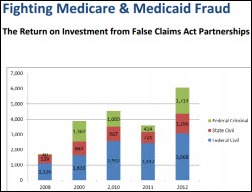
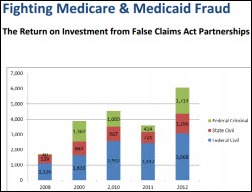
Finally some good news from the government: every dollar invested to investigate and prosecute healthcare fraud returns at least $20, based on data collected from 2008 to 2012.
A bipartisan group of House lawmakers introduces the Sensible Oversight for Technology which Advances Regulatory Efficiency (SOFTWARE) Act that would clarify regulations for mobile medical apps, EHRs, and other HIT technologies. The legislation builds on the FDA’s final guidance on mobile healthcare apps.
Healthcare.gov contactors tell a Congressional panel that it’s not entirely their fault the site doesn’t work as well as hoped – the government should have supervised them better and tested more thoroughly before setting the go-live date. An SVP of Canada-based CGI stuck with the story that user volume was greater than expected and said it was CMS’s job to do end-to-end testing, not the company’s. Andy Slavitt of Optum, which owns contractor QSSI, said the government decided late in the game to require users to create an account before viewing insurance plans and the company’s function for that didn’t work well in the site’s first few days. Rep. Anna Eschoo (D-CA), who represents the Silicon Valley, said blaming user volume is a “lame excuse” that “really sticks in my craw,” adding that Amazon doesn’t crash the week before Christmas.
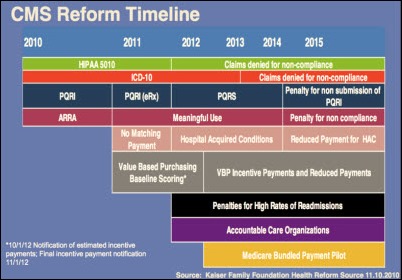
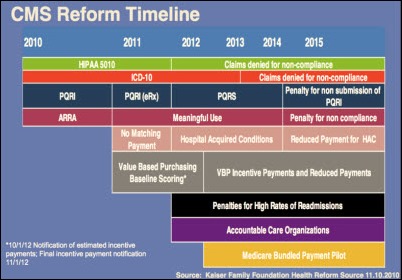
John Halamka’s conclusion about Healthcare.gov: “… Nine women cannot create a baby in a month. There is a minimum gestation period for IT projects and our policymakers should learn from the lessons of the Health Insurance Exchange and re-calibrate the timelines shown in the graphic above [the CMS reform timeline] so that everyone is successful.” Or as one of my hospital programmers always told me years ago when pressed to make a delivery date, “You can take the cake out of the oven any time you want, but don’t blame me when you don’t like it.”

The VA’s Office of the Inspector General finds that three ED patients died at the Memphis VA after receiving substandard care, one because the doctor violated policy by hand-writing an order for a drug to which the patient was allergic, a situation that CPOE would undoubtedly have warned about.
Innovation and Research
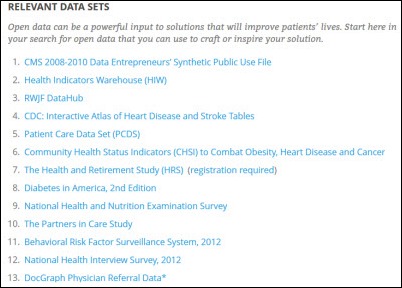
The Merck | Heritage Provider Network Innovation Challenge offers $240,000 in total prizes for creating tools that help people with heart disease or diabetes follow their care plans. Submissions are due November 10, 2013.
A peHUB article called “Disrupting healthcare – on whose terms?” says that companies with no healthcare background who jump into healthcare IT investments have a big performance disadvantage. It concludes, “These data clearly show a massive advantage for firms with healthcare expertise when making healthcare investments. And why shouldn’t they? Don’t we assume, for instance, that energy investors do better at energy investments vs. those firms without any energy focus or experience? Healthcare is at least as complex and regulated an ecosystem as energy and yet it repeatedly experiences cycles of outsiders driving up investor frenzy.”
Technology
Verizon Enterprise Solutions releases Converged Health Management, a remote patient-monitoring platform that allows patients to use biometric devices to capture vital signs and automatically transmit details to their providers.
Other
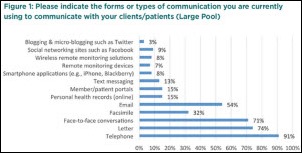
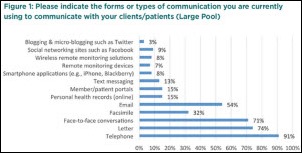
Providers rely on telephone calls, letters, and face-to-face conversations more than any other method to communicate with patients, despite the increased use of newer technologies such as text messaging, social networking sites, portals, and emails.

HIMSS announces keynote speakers for the mHealth Summit in December: FDA Commissioner Margaret Hamburg, Qualcom CEO Paul Jacobs, Denmark’s Minister of Health, and Nobel Peace Prize Winner Muhammed Yunus. I’ll be reporting from the conference, as will Travis from HIStalk Connect. HIStalk will have a microscopic, sparsely furnished booth in the exhibit hall because they were nice enough to give us one, which will be capably manned (or womanned) by the fabulous Lorre. She may have nobody to talk to since I’m not certain the mHealth Summit draws a lot HIStalk readers, but if you’re going, find our micro-booth (#1305, right beside a slightly larger booth and company called AT&T) and say hello.
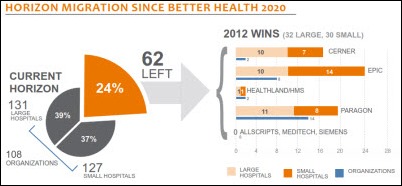
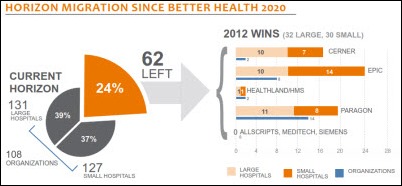
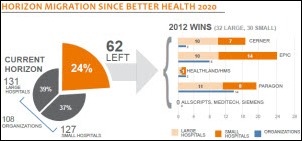
More on the summary of KLAS’s report on McKesson Paragon, which concluded that the product isn’t ready for big hospitals in important areas (like clinical functionality and an integrated ambulatory system) and has experienced a pretty big drop in KLAS scores since 2010, but customers seem satisfied to wait for the three-year roadmap to bring it up to their expectations. The graphic above shows that 32 large hospitals bought Horizon replacements in 2012, with 10 each choosing Cerner and Epic and 11 choosing Paragon, with cost being a big driver for the Paragon wins. Among smaller Horizon hospitals, Epic was the big winner, probably through acquisition if I had to guess since I doubt those hospitals could afford Epic otherwise except though an affiliate agreement. Allscripts, Meditech, and Siemens didn’t get a single Horizon replacement deal, with the most startling fact in that statement being the inability of Meditech to execute in what should be a receptive market.

Brian Stowe, the former Epic project manager charged with taking sexually explicit photos of passed out women (of whom six of the eight were his Epic co-workers,) pleads guilty to taking photos and video of a 17-year-old girl asleep in his bed and will be sentenced in January to a minimum of 15 years in prison. He still faces 62 felony counts.
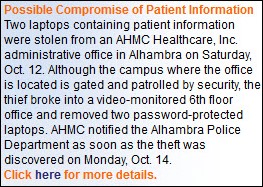
A thief breaks into the offices of AHMC Healthcare (CA), making off with two unencrypted laptops on which was stored the information of 729,000 patients. The hospital has expressed a sudden interest in encryption, which the near-certain $1.5 million fine might have covered. Apparently hospitals are unable to muster the technical expertise and financial motivation to encrypt computers until after they’ve been inevitably burned and fined, so it costs them even more. Police arrested a vagrant for the theft on Wednesday, but the laptops are still missing.
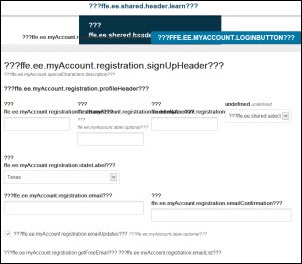
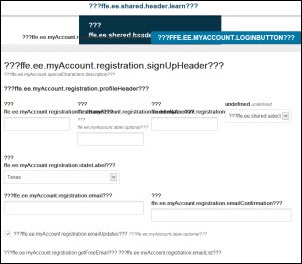
 After reading Tweets and news stories about all the folks who have been able to find more affordable healthcare coverage options on the Healthcare.gov website, I decided to once again attempt the application process. Unfortunately I did not get farther than the second screen, which contained a lot of gibberish. I guess I’ll give Jeff Zients, Verizon, and all the newly recruited techies a bit more time to fix things.
After reading Tweets and news stories about all the folks who have been able to find more affordable healthcare coverage options on the Healthcare.gov website, I decided to once again attempt the application process. Unfortunately I did not get farther than the second screen, which contained a lot of gibberish. I guess I’ll give Jeff Zients, Verizon, and all the newly recruited techies a bit more time to fix things.
Weird News Andy says he is singing “La Cucaracha” to himself as he enjoys this story: cockroach farming is booming in China as the country finds them both delectable as a culinary treat and miraculous as a a basis for drug development, with hospitals using them to treat burns and a pharmaceutical manufacturer claiming its cockroach syrup cures ulcers and TB.
Sponsor Updates
- NVoq announces the general availability of its SayIt 8.2 release.
- Strata Decision Technology hosts 400 attendees in Chicago this week at its annual summit.
- Wolters Kluwer Health introduces Lippincott’s CoursePoint, a digital course solution for nursing education.
- DocuTAP will integrate Wolters Kluwer Health’s Health Language applications into its EMR solutions for the urgent care environment.
- Intelligent InSites will hold its InSites Build 2013 conference October 29-30 in Fargo, ND.
- Greythorn will offer an October 29 webinar on Radiant implementation and optimization.
EPtalk by Dr. Jayne
Let’s face it, consultants are a fact of life in our industry. Most of us are trying to do more than we possibly can with the staff we have in place. We’re trying to cope with an ever-changing regulatory landscape. We’re feeling the squeeze between immovable deadlines and vendors who aren’t delivering required code as early as we want them to. Sometimes we can’t hire new FTEs quick enough or we may not have anyone with the skill sets needed to help us stay compliant. And so, we turn to consultants.
A reader mentioned last week that his or her company was not in favor of paying meal and incidental expenses for consultants and asserted that the consultant’s employer should pay those expenses since it is already charging a hefty per-hour fee. The comment sparked several replies, so I decided to reach out to some of my friends who are consultants to see what they think. I’ve been on both sides of the story as I’ve hired consultants and been one, but I’ll hold on my thoughts for now.
Most of the consultants I talked to this week feel that their clients have a skewed view of what consultants actually are paid. Even though a consulting firm or vendor may charge $200 or $300 an hour, it’s unlikely that the individual field consultants are taking home even a third of that. Although many senior consultants do quite well, many junior consultants spend up to 50 weeks a year away from home. Divide the pay by the hours away from home and family and the paycheck starts to look even less great.
Companies have to cover for the time that their consultants are engaged in non-billable activities such as training, staff development, continuing education, and maintaining competency with EHR vendor software. Increasingly clients are refusing to pay for consultant travel time (or imposing ridiculous travel caps that don’t even cover flying time) and that has to be covered as well. One consultant I’ve used repeatedly tells the story of going to a small town in a remote western state, where he had to take four flights (to stay under the client’s air fare cap) and then drive four hours to get there. The total travel day was close to 18 hours and then of course he had to get home. The client had a three-hour round trip travel cap. I’m pretty sure the client knows they’re a four-hour drive from the nearest airport.
One of my favorite niche firms works with a single EHR vendor and maintains a very small group of consultants. All of them are nurses and the CEO is a nurse as well. Most of them continue to maintain their licensure and attend CNE so they can stay current with clinical topics. It makes them extremely effective and I’m happy to pay a higher per-hour fee for them because I know I’m getting the quality input I need for projects that need both nursing or other clinical expertise and a high degree of vendor-specific knowledge. I’m also happy to pay more for a small firm that I know runs lean and has little administrative bloat because I know they pay their workers well.
Unfortunately, the health system I work for has what can only be described as Enron-style accounting and they are constantly late in paying the consulting invoices even when all supporting documentation is provided in a neat and timely package. I wish the accountants understood the value of these consultants – they are super busy and don’t need my business to stay afloat and I’m afraid eventually they’ll stop working for me because it is simply too much of a bother.
Due to the size and scope of some of our projects, I’ve had engagements with the 800-pound gorillas of the consulting world as well. Although there have been a handful of consultants that have tried to take advantage of expense policies, the majority have been fair in what they submit for reimbursement. For those who have been a little too cavalier with their spending, it’s been fairly easy to address it with management. I haven’t yet run across anyone operating like the George Clooney character in “Up in the Air” where he pushes his expense reports to maximize his airline mileage. If you’ve ever been a road warrior and haven’t seen the movie, I’d recommend it.
The best defense against ridiculous expense reports is negotiating a good contract with the consulting firm. Know what you are willing to pay for, but be fair. Know what typical hotel rates are in your area and make sure you are allowing your consultants to stay somewhere that you would consider staying yourself. I’ve heard horror stories (and seen pictures) of “client recommended” hotels that I can’t imagine a hospital administrator would expect his own family to accept. If you have a corporate discount, make sure consultants have the codes, and if there is a limit to the number of rooms that can be booked at the corporate rate, that they book well in advance.
As far as meal allowances, they seem fair for the companies I’ve worked with. I don’t begrudge my consultants the coffee and snacks they submit because they’re working their tails off for me. Some of them can deliver in a week what my IT department takes a month to deliver, so the expense is well worth it. One of our IT buildings is away from the main hospital campus and there aren’t any close restaurants. I always have lunch delivered for the consultants so they don’t have to waste time trying to find food and worry about their logistics. But when I negotiate engagements, that is taken into account and their maximum daily meal reimbursement is adjusted accordingly. If you don’t want to pay for alcohol because you’re a faith-based organization, write it into the contract or hire a consulting firm that doesn’t allow alcohol to be submitted.
As I’ve mentioned before, I did a fair amount of consulting while I was building my CMIO skills and still do a couple of jobs a year with the full permission of my hospital. Ethics and professionalism are what keep consultants from abusing the system. Having been in those shoes, if I find someone milking it, I’m going to send them packing. On the flip side, I’ve been abused by clients and it’s never pleasant. At one site where I was engaged for a couple of months, my “handler” would routinely book my schedule with 10-hour days containing back-to-back meetings that didn’t allow for restroom breaks, let alone lunch breaks. I would hit the local supermarket before going on site and stock up on granola bars, fruit, and drinks. The same client didn’t even have cups or utensils in the break room, so I had to travel with my own mess kit if I brought restaurant leftovers.
Another client scheduled a business dinner after a full work day. The agenda was for me to meet with providers and address their concerns regarding an upcoming implementation. It was at a fairly expensive celebrity chef restaurant and I was looking forward to it. However when the bill arrived, the client asked for separate checks and made me pay for my own. Needless to say that blew my expense account for the day (actually three days’ worth) and I had to cover it out of pocket. Had I been on my own that evening, I probably would have had a turkey sandwich and a handful of grapes. Maybe some chips if I was feeling wild and crazy. Most of would agree these examples are pretty extreme, but unfortunately I’m not the only one who has had those experiences.
If you’re looking to cut down on consulting expenses, look at whether you really need consultants on site. Those who work projects remotely don’t submit meal or travel expenses and often they are more productive when your staff isn’t interrupting them or trying to pick their brains on unrelated projects. One consultant friend keeps me laughing with stories of his prowess at slaying scope creep since his client’s analysts are hell-bent on involving him in work that has nothing to do with his engagement just because they know he has the skills. He could probably deliver his analytics build faster if he was working from his bachelor pad than sitting in your cube farm among squeaky chairs, gossipy employees, and those who bring colds and flu to the office.
That’s another thing – nice clients have a plan for when consultants get sick or have family emergencies. They are understanding. They don’t make you feel bad when your daughter breaks her arm and you have to accompany her to the operating room (true story from a former grad school roommate.) They may even offer to have a physician evaluate you and make sure you aren’t near death alone in your hotel room after you get food poisoning at a dinner they catered. I’ve written prescriptions (with appropriate examination and documentation, of course) to treat minor illnesses and helped consultants get care after sports injuries. Just because they’re consultants doesn’t mean they’re invincible.
If clients really have a problem with consultant expenses because they object to having to pass them on to patients, I recommend they look at their own policies as well as consulting policies. One hospital where I’m on staff provides a 64-ounce mug to each new employee, who can then fill it with free beverages throughout the work day. Although it was instituted as a staff perk, I can’t help but wonder what the patients think as they see staff slurping their way through the day from mugs that are less than clean. You can bet that’s being passed onto the patient bill, as are the employee health care expenses from obesity and diabetes since I rarely see people filling up with diet pop, that’s for sure. Then there’s the lost productivity for the trips to refill.
While we’re at it to cut costs and save healthcare, let’s cut out frivolous marketing, overkill signage, and anything having to do with “centers of excellence.” I bet we could lower some hospital bills right there. But let’s not take it out on consultants who are working hard on our behalf.
What do you think about consultants and their expenses? Email me.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.













































The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en