Bruce Springer is president and CEO of OneHealth Solutions of Solana Beach, CA.

Tell me about yourself and the company.
I’ve been in the healthcare software industry for about 20 years. One of the early companies I started and co-founded was WebMD in 1996 in Atlanta. Since then, I’ve served as a CEO and board member for numerous healthcare technology and startup companies. After serving as a board member for OneHealth last year, I was asked to join as CEO of the company.
The company is a social health platform company that works with health plans, employers, providers, and patients. Typically working with them to help improve health outcomes and lower costs utilizing social media, clinical tools, and gaming to better manage chronic patient populations.
Why is patient engagement such a hot topic all of a sudden?
Partly it’s due to government regulations. You look at Meaningful Use and you look at many of the different QA programs. Patient self-management, self-engagement is becoming a critical component of any one of those programs. As the risk is starting to shift from the insurance company to the employer and now down to the provider, they’re realizing that they can’t manage that care in these high-cost centers in the physician office, the clinics, and then the hospitals. They need a new way to get the patient engaged into reducing their own cost and managing their own conditions. That will greatly improve the outcomes for the whole industry.
But engagement is only a piece of it. In the past, engagement was a call from a nurse in the call center once a month to check in on you, or a direct mail piece to your mailbox. But is that really engagement? If you don’t get them to consistently or persistently engage and create better habits, you’re not going to change behavior. And if you don’t change behavior, you’re not going to really reduce the cost of the system.
There’s a theory that patient engagement increases the involvement of people who are already motivated, but doesn’t do a whole lot for that vast majority who rack up most of the expense. Do you agree with that?
I very much agree with that. One of the approaches that we’ve had at OneHealth is to engage them anonymously. They can join into communities where they don’t feel threatened, or maybe they have a shame-based behavioral mental health condition that they don’t want to share with others. The ability to do that where they’re not known and there’s no fear of retribution, no concern for confidentiality, where they can get in and work on the things that matter most to them, that their employer, their doctor may not even know about.
We’ve integrated behavioral and mental health-related capabilities with medical conditions to help patients be able to engage where they want to engage, versus many disease management programs where you start at Step 1 and you go through Step 10. Why not engage somebody where they want to engage on the thing that’s most meaningful for them that they want to change? Then if you help them there, you’re going to make a radical difference on their overall health.
We always look at things like diabetes. Our diabetes community is driven by weight management, depression, other things. It’s not because I’m a diabetic, but 50 percent of diabetics are also depressed. If you don’t deal with those depression-related issues, it’s going to be very hard for you to get somebody to take their meds, adhere to their care plan, lose the weight, and do the work that they need to manage their diabetes. You have to look at the underlying issue and help them support that issue. That’s why you don’t get meaningful engagement across broader populations.
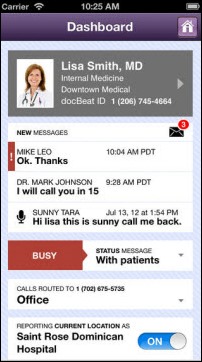
I tried the site this morning and it was really easy and encouraged people to register anonymously if they prefer. I like that users can click their current mood, find cohorts to interact with, and set behavioral goals. What are users finding most valuable of the site’s functions?
Everybody’s different. It depends on where they’re willing to begin their journey. The emotional indexing that you talked about is something we present every time you check in. That is a scale of one to five, how you’re emotionally doing, will potentially create a bad behavior. Then we measure that scale against the communities that you’ve joined to determine the concern or the level of intervention needed to help that member avoid that emotional feeling driving to a bad decision.
For instance, this company was started with alcoholism, managing chronic conditions around substance abuse. Somebody’s craving at that point in time. If you don’t intervene, they’re going to probably drink. It’s allowed the platform to have a 24/7 intervention. When you check in craving, your network, our coaches — we have our own OneHealth coaches — will now engage you at that point, at the very instant where you’re having that emotional feeling, before you actually create a bad behavior that corresponds to it. We get 97 percent utilization of the emotional check-in on a daily basis for those members that check in.
We have challenges that are highly popular. Right now we’re running a nutrition challenge where people are taking pictures of their plates of food at dinner. Our nutritionist will review them and say, here’s things you could have done better, here’s a way to better manage and balance that meal. Then we create teams and they support each other and have a good time.
We just had a stress challenge where you were picking something in your life that causes stress and creating an anchor around it and an intention to solve it. Then every day, we had chat rooms and meditation rooms for folks to come in and just relax for five to 10 minutes during their busy day. Our coaches would give them tips every day, different tip on things that they could be doing in their life to reduce their stress.
The challenge communities have become a very active component of the program as well as our expert discussions. For each of our communities, we have a physician or psychologist who’s an expert in that field. Weekly, they’re getting on and doing live video chats about new things, content, things that they should be looking for that particular disease or community that they’re in, or the co-morbid things that they’re dealing with. We record every one of those expert discussions and we put them back on a podcast, so if you miss it live, you have the opportunity to come back. As well as our group chats. We have video chat capability for up to 50 individuals at any one time. People participate in our chats and our group programs on a daily basis.
Just connecting with others, supporting others, finding others in need, and engaging them and helping them through their journey online. That’s the most powerful part of the social community. Are you more willing to talk about your disease or your issue with somebody at your work or somebody in your home who may be a trigger for the reasons why you have those particular issues, or are you more willing to work with somebody who has the exact same issue, has been through the exact same program that you have, and is trying and working towards their own journey for curing or managing that condition, or better yet, a peer who has already achieved it and is helping another peer, help them achieve their own goals? That’s probably the most powerful piece — the social network and the interconnectivity of like users.
Do people interact differently a Facebook-like setting than they would either in a small group meeting or on the phone with a provider?
Very much so. It’s funny because our members say to us, Facebook is the place I go when I want people to believe what I want them to believe. OneHealth is a place I go where I am who I am. I’m not going to put up my mental health, my depression, my stress anxiety disorders on Facebook and let people know that I have it. But on OneHealth is the place I go where I am who I really am and I really am trying to get help for it.
If you look at most social networks, 98 percent of users on social networks are lurkers. They’re not really the folks that are engaging and driving content. They’re consuming content, reading other people’s stories, reading other people’s pictures. There’s benefit from that in a healthcare setting, because now they’re reading about people who are dealing with the conditions they are. They’re getting educated about it. They may not personally engage.
But once we get them engaged — whether it is getting them to an expert discussion, getting them into a meeting, connecting to one of our health coaches, connecting to their peers — once they start making relationships, our little nudge to get them into the program is they have the ability to empathically respond. On Facebook, you can “like” something. On our site, you can like it, you can understand it, you can say, “I felt like that, too. I’ve been there before.” You can relate to the person just by pulling down and clicking a button, opening somebody up to the discourse with the other members.
Once they do that, they start getting integrated into the platform. They start getting social. Once they start getting social, then we’ve got the opportunity to create consistent engagement to drive results.
I assume it’s insurance companies and employers that foot the bill. Does providing that peer support pay off for the folks who are paying for it?
It does. We’ve done studies. We did a pilot program with Aetna around acute substance abuse addicts that were high cost, high acuity to their system. We ran a pilot study where we took a cohort and then they took a cohort through their traditional care management process. They attributed us with reducing readmissions by 58 percent and gave us $9,000 in medical savings in the first year. We did a claim run on every one of the members.
One of the interesting things in that cohort, folks with substance abuse, was we didn’t stop people from relapsing. People still relapsed. These were highly acute substance abuse members. When they did relapse, they came back to OneHealth for support versus going to a clinic, going to a high-cost center. Most of the folks we did keep sustained in their sobriety, but those that did fall off, they came back and used the social support of OneHealth to mitigate the cost of the health system. We have numerous studies like that across different entities.
But to your point, yes, we started with health plans because they have a large population of members that we could provide this out to to be able to get the data so we can provide clinical evidence about our efficacy, our return on investment, which we believe is both medical savings, reduction in medical loss ratios, as well as operational savings. Can we manage a broader percent of the population at a lower cost than using a call center or a direct mail piece? People use us for multiple ways to save dollars, both medical and/or operational savings.
Once we expanded the platform to include integrated behavioral and medical conditions, we then started working with self-insured, large employers. We started working with Carlson, Safeway, Tyco and others on a direct basis.
We also have over 30 providers now that are working with us, either because they’re taking risk towards an ACO model and they’re looking at ways to manage populations outside of the acute care setting and integrating behavioral, where they’re traditionally a condition based on a medical condition, integrating the behavioral management component into that process. Those are folks like Memorial Hermann in Texas and Boston Medical Center that are working with us on lots of different programs and lots of different types. We will start putting up some white papers on the results with them fairly shortly.
Do you have any concluding thoughts?
The industry of population health management is obviously growing and it’s got lots of different components. To truly manage these populations that are at risk, we believe the social media component has got a place in that world, especially when you’re looking at it from a peer support model.
You can really drive highly effective engagement. You get people who otherwise wouldn’t engage with the industry to engage. You have the opportunity to do a lot of unique things that are hard to do through a call center or a phone-based service. It has the opportunity to play a significant importance in behavior change, reducing costs, and driving value to the health system.
Comments Off on HIStalk Interviews Bruce Springer, CEO, OneHealth Solutions
















































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…