Chuck Podesta is SVP/CIO of Fletcher Allen Health Care of Burlington, VT.

What lessons did you learn as your single hospital expanded into a health system?
I’ve worked with systems in the past, so I was prepared from a due diligence standpoint to understand what we were getting into. The interesting thing has been is being at the beginning of a system being born as opposed to going to work at an organization that already had created the system. That part has been really, really exciting.
From a learning standpoint — and I’ll just speak from an IT perspective right now — it’s how you merge the cultures of the different organizations, both from a leadership perspective and staff perspective. We haven’t merged all four hospitals’ IT under IS from a cost center perspective, but I am the system CIO over those organizations.
I work very hard to get our leadership within IS to work with their leadership in their organizations and staff-to-staff communication as well. We’re geographically disparate from each other, so it makes it a little bit more difficult. That part has gone really well. That’s been the biggest thing that we’ve done.
We created an IT council that’s a high-level group of the high-level IT folks. Then we did a sub-group that’s made up of low-level managers but also some staff that are working together across the system and looking at things like linking email and some of the nuts and bolts things that need to be done behind the scenes.
That’s brought these teams together, working on the same projects. What we’re finding is that the more and more that you do that, it’s going to make it easier as we get to the more difficult projects of implementing different types of technologies in these organizations.
Every hospital has the challenge of trying to look at new tools to support risk-sharing arrangements and population health management, but you’re also faced with trying to combined the financials to give a view that makes sense and to understand the physician relationships.
Absolutely. If you look at the last time we talked in July 2009, we were Fletcher Allen Health Care academic medical center, Burlington, Vermont. Now we’re a four-hospital system. We also are 50 percent owner of OneCare, which is a Medicare Shared Savings Program with Dartmouth-Hitchcock. There’s 14 hospitals involved in basically the entire state of Vermont, about 50,000 covered lives that are under that right now. A very large Medicare Shared Savings.
We’ve got the issues around exactly what you mentioned — the data analytics, advanced population analytics that we’re implementing. We’ve got some unique stuff going on there, along with working with two health information exchanges, because we are not only in Vermont, we’re also in northern New York. We work closely with VITL in Vermont and Hixny in northern New York. They’re working together to link their two HIEs together to benefit us as well.
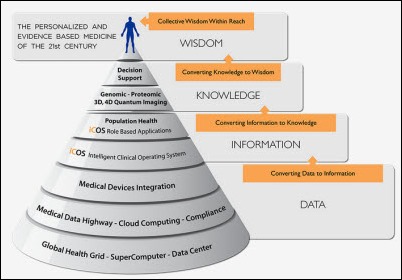
On the advanced population analytics side, we’ve joined a group called Northern New England Accountable Care Collaborative. That’s made of Eastern Maine, Maine, Dartmouth-Hitchcock, and now ourselves. It’s a unique opportunity. They take our CMS claims data in and using VITL, we move our EHR data into that data warehouse. We can also have access to the de-identified data of the other organizations. Instead of just looking at populations of 300,000 or 600,000, now we can look at populations that are in the millions. The bigger the denominator, the better off you’re going to be.
People claim that healthcare is behind technologically, but we have business models that seem to change every five years, government involvement and reporting, and insurance company requirements. Everybody wants something different on the back end and yet you’re trying to keep the front end running. Is that sustainable? I can’t think of any other industry where there’s so much change that isn’t to support the business, but to meet new minimum external requirements.
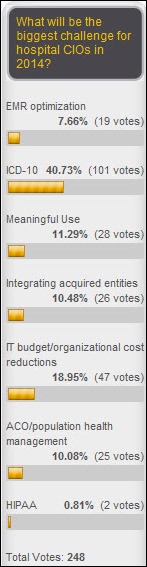
I think over the next year we’re going to find out whether this is sustainable or not. If you look at the priorities that we have right now, we have ICD-10 coming. We’ve got Meaningful Use Stage 2, then Stage 3. Privacy and security is huge with the passage of the final Omnibus Rule and we’ve got to spend a lot of time there. We’ve got our system IT priorities that we need to put in place, and then also our OneCare ACO IT priorities that need to be put in place.
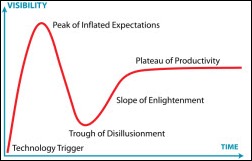
You add all those up and just look at the care and feeding of an Epic EHR and the priorities that go into that, it’s daunting. I joke a little with my senior leader that in the past, we were able to do a business planning session, have the IT strategy follow the business plan, and do a three- to five-year IT strategic plan. That’s no longer the case. I can’t even do a six-month strategic plan.
What I’m trying to get my organization to do is to talk a lot about how do you survive, how do you manage, how do you lead in an organization that every single priority is a high priority? In the past, you could make a list and start at one and go to 10. You might have four or five projects that are twos. But in this particular case, they’re all ones. The federal government deadlines on a lot of these things are all coming to a head.
How do you get your organization to work in that type of environment? That’s been amazing from a cultural standpoint. What you’re going to see across the country is some organizations will be nimble enough to do that and then others won’t.
Given the low likelihood of success and the fact that CIOs aren’t typically given extra resources, will it be harder for CIOs to keep their jobs?
Absolutely. If they don’t set the expectations with their senior leader colleagues … even though I mentioned earlier that I make a joke about not being able to do a six-month strategic plan, I’m actually pretty serious about that. If my senior leader colleagues — my boss, my CEO, the board – are expecting a three-year plan and I’m not clear on what our priorities are, even over the next couple of months, and to get them to understand, then I’m setting myself up for failure. I know that has happened to other CIOs across the country.
This coming year, year and a half, I think there’s a lot of CEOs out there that expect all this stuff to get done. If the CIO is not clear with the individual that they report to, that based on the resources that they have, these are the things that we can get done and these are the things that we can’t get done. We’re also in a situation where you can’t add any more resources. I can’t go to my boss and say, give me 10 more FTEs and I can do 10 more things. It’s just unsustainable from that standpoint.
It will be interesting. I think there will be a lot of turnover in the next year to 18 months or so as the Medicare penalties kick in as well in 2015. There will be a lot of CIO turnover, I believe.
In the past, that type of environment is where health systems start thinking about outsourcing their IT departments because consulting firms claim they can do more with the same resources and still make a profit. Do you think the environment is going to swing back what seemed to be a diminishing trend of health systems looking outside to have their IT run by someone else?
Yes. What you’re going to see first, though, is just from the healthcare industry in general, the mergers and acquisitions that are happening. I firmly believe that within the next five years, there’s probably going to be 100 to 200 health systems in the United States. They will be regionally focused. Bigger is going to be better in this new world of population health management. That’s happening all over the United States.
What you’ll see first is merging the IT shops. How that all shakes out will take a little bit of time and outsourcing may play a role in that. But I see those IS organizations working hard to come together first. They may look at outsourcing, but I just don’t think that’s going to be as high a priority as merging these various organizations.
What types of health IT-related businesses do you think will benefit from that consolidation scenario and which ones do you think will suffer from it?
The call center can be outsourced and consolidated probably fairly easily. We’re doing that now across our system. That’s probably one of the easier ones. If you look at field service, network, server management, and data centers, for example, there’s a lot of savings there. Looking at how you merge your data centers and cut some costs there. That’s the easy part.
The harder part is on the application side. If you’ve got more than one Epic organization coming together … you’ve seen one Epic organization, you’ve seen one Epic organization. They all have their different nuances. But most of the systems are coming together. You have an Epic organization and the other one might be a Cerner, and you’ve got to go through a process of, are you going to keep them that way, or are you going to put Cerner in the other organization, or are you going to choose Epic?
That is going to be much more difficult to do. The application people that support those applications, the retraining associated with that, is just going to be really, really difficult to do and very costly. For these large organizations coming together, you’re talking hundreds of millions of dollars. You’re seeing it now — some of the bigger organizations are doing implementations and mergers and acquisitions at the same time.
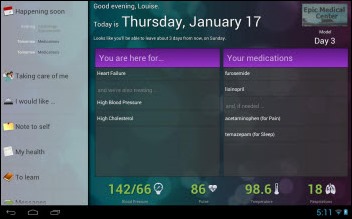
There was a lot of buzz recently about your health system announcing plans that it expected to lose a lot of money but also that it would be doing a lot of hiring to support Epic. Internally, is Epic providing the expected benefits and return on investment, or are executives privately questioning whether the cost was worth it?
If you had asked that question a year ago … to be honest with you, I was questioning it. A lot of that was self-inflicted. It didn’t have to do with Epic. We had implemented Epic. We had gone live. We spent a lot of time on the ambulatory side and really got that humming.
Then we didn’t take care of the inpatient side of things. The inpatient side got very stale. It got very customized. I think we had 70 different flowsheets across the organization. Data wasn’t landing in the database where it should be to get reports out. We ran into that with Meaningful Use. It was very difficult for us.
About a year and a half ago, I hired a CMIO. He came in and one of the ideas he had was that we needed to go to 2012 upgrade. He said, why don’t we just take all 7,000 enhancements and go back to model as close as we can? Originally when we thought about that, we were like, what are you, crazy? Typically when you do an Epic upgrade, you look at 50, maybe 100 enhancements. You never get to all the enhancements from an Epic upgrade typically.
This was a radical change from that. When we approached Epic, they were really noncommittal on whether we should do that. But the more we talked about it, they gave us the green light. Last spring, we started that process. We went live in October. It completely changed. It was a non-event over a weekend. The training wasn’t too difficult. It became a better system.
Now we’re relying on Epic to do the R&D instead of us building things that Epic’s already building in future releases. We found ourselves doing that when we looked at 2012. We were building things in 2010 that already existed in 2012. It just didn’t make any sense at all.
We got creative on the how we used consultants during that period. We needed some help and we used some firms come in and help us from a resource perspective, because you imagine a whole change going from an 80-20 customized system to more of an 80-20 in the opposite direction model versus a custom system. The changes that we needed to make were huge.
We worked with a national company, but their local headquarters are here in Vermont. It’s a perfect marriage. They were Allscripts at the time. Their name is MBA HealthGroup. They were nervous based on where Allscripts was going and we needed help, so they came forward. We started talking about us sponsoring them with Epic so that they could create an Epic practice. In return, they would send people, get them certified, and bring them on site at a very reduced rate, about a 50 percent reduction in what you normally would pay.
After a six-month period, we would have the right to hire, which we thought was great. We view that as a creative win-win situation with them. They’re offering it across the country now to certain organizations. We used them for our training in the Epic space. We hired two of the individuals at the end of the project. We were able to pick the best and brightest out of the group and hire them. That was a win all the way around.
We’re also reaching out to the local colleges and universities here and getting lists of engineering, math, and science majors with 3.5 and above and encouraging them to apply for open positions. We’ve hired a couple of kids right out of college. They have been amazing. The productivity is just … they learn so fast. What we’ve found is you can’t give them a deadline, because if you do, they’ll wait up until the last minute and then get it done. They can do it a lot faster than the deadline that you give them. Just give them the work and don’t give them a deadline and you’ll get much more out of them. That’s been fantastic and we’re continuing that type of program as well.
What are your biggest challenges and opportunities over the next one to two years?
Looking at the next year,we’ve got ICD-10. We’ve got Meaningful Use Stage 2. Privacy and security, which is constant vigilance on that.
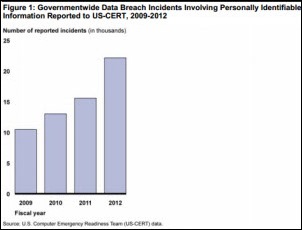
Every time you turn around, you see another breach. Everybody’s going to have a breach at some point. At some point, somebody’s going to do something stupid and it won’t be malicious and you’re going to have a breach. But the ones that I see that could be avoided, those are the ones that really get me going. The non-encryption of a mobile device. It makes no sense to me as to why people haven’t done that.
The breaches that are happening, those are the only ones we know about. There’s so many out there that we don’t know about. It’s going to be more and more difficult because OCR is certainly going to ramp up the audits and the fines are going to start coming out. That’s a big one.
Then the accountable care IT infrastructure that we’re building with the health information exchange and population analytics. Then trying to look at synergies across our system from an IT perspective and where we can save some money and increase services across the four hospitals. My expectation is that the next time we talk, we’ll be larger than a four-hospital system.
All that stuff has to get done in the next 12 months. Otherwise we’ll be behind the curve on what we need to get done. A lot of other organizations are in the same situation whether they realize it or not. They have these same priorities, especially if they have an ACO or are part of an ACO. Whether they realize it or not, all that stuff is coming to a head over the next 12 months.
Do you have any final thoughts?
I can’t say enough about the privacy and security side of it. A lot of the technology that we use today enables physicians and nurses and clinicians to take care of patients. These systems are helping to give us higher quality, eliminate errors, and impact patient safety. That’s been great and it’s been worthwhile.
But we have a mission — we should have a mission — to protect the privacy of the information within these electronic health records. I can’t go to a bedside and take care of a patient directly, but I can certainly involve myself directly in the privacy and security programs of this organization. I think more and more CIOs that do that and get directly involved in the privacy and security, understand it, make sure you have a chief information security officer, get the tools that you need, figure out a way to justify those, and get those in. For our patients, that’s the one thing that a CIO can directly impact.
Comments Off on HIStalk Interviews Chuck Podesta, SVP/CIO, Fletcher Allen Health Care





















































The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en